- Print this page
- Share this page
Download a PDF of this document in full.
Foreword
The State Insurance Regulatory Authority has reissued the 4th edition of the NSW workers compensation guidelines for the evaluation of permanent impairment (catalogue no. WC00970) (the Guidelines) for assessing the degree of permanent impairment arising from an injury or disease within the context of workers’ compensation. When a person sustains a permanent impairment, trained medical assessors must use the Guidelines to ensure an objective, fair and consistent method of evaluating the degree of permanent impairment.
The reissued Guidelines have been made to include some minor changes including changes consequent to the enactment of the Personal Injury Commission Act 2020 (PIC Act). No changes are made to the provisions in these guidelines relating to the evaluation of permanent impairment as developed in consultation with the medical Colleges under s 377(2) of the Workplace Injury Management and Workers Compensation Act 1998 and as set out in cl 13 of the Guidelines.
The Guidelines are based on a template that was developed through a national process facilitated by Safe Work Australia. They were initially developed for use in the NSW system and incorporate numerous improvements identified by the then WorkCover NSW Whole Person Impairment Coordinating Committee over 13 years of continuous use. Members of this committee and of the South Australia Permanent Impairment Committee (see list in Appendix 2) dedicated many hours to thoughtfully reviewing and improving the Guidelines. This work is acknowledged and greatly appreciated.
The methodology in the Guidelines is largely based on the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 5th Edition (AMA5). The AMA guides are the most authoritative and widely used in evaluating permanent impairment around the world. Australian medical specialists representing Australian medical associations and colleges have extensively reviewed AMA5 to ensure it aligns with clinical practice in Australia.
The Guidelines consist of an introductory chapter followed by chapters dedicated to each body system.
The Introduction is divided into three parts. The first outlines the background and development of the Guidelines, including reference to the relevant legislative instrument that gives effect to the Guidelines. The second covers general assessment principles for medical practitioners applying the Guidelines in assessing permanent impairment resulting from work-related injury or disease. The third addresses administrative issues relating to the use of the Guidelines.
As the template national guideline has been progressively adapted from the NSW Guideline and is to be adopted by other jurisdictions, some aspects have been necessarily modified and generalised. Some provisions may differ between different jurisdictions. For further information, please see the Comparison of Workers’ Compensation Arrangements in Australia and New Zealand report, which is available on Safe Work Australia’s website.
Publications such as this only remain useful to the extent that they meet the needs of users and those who sustain a permanent impairment. It is, therefore, important that the protocols set out in the Guidelines are applied consistently and methodically. Any difficulties or anomalies need to be addressed through modification of the publication and not by idiosyncratic reinterpretation of any part. All queries on the Guidelines or suggestions for improvement should be addressed to SIRA at contact@sira.nsw.gov.au.
Part 1 - Intent and legislative basis for these guidelines
1.1 The reissued 4th edition of the NSW workers compensation guidelines for the evaluation of permanent impairment (catalogue no. WC00970) (the Guidelines) is made under s376 of the Workplace Injury Management and Workers Compensation Act 1998 (WIMWC Act) and commence on 1 March 2021 when the Personal Injury Commission is established. The Guidelines are to be used within the NSW workers compensation system to evaluate permanent impairment arising from work-related injuries and diseases.
The Guidelines adopt the 5th edition of the American Medical Association’s Guides to the Evaluation of Permanent Impairment (AMA5) in most cases. Where there is any deviation, the difference is defined in the Guidelines and the procedures detailed in each section are to prevail.
1.2 The Guidelines replace the WorkCover Guides for the evaluation of permanent impairment, 4th edition, which was issued on 1 April 2016, and subject to the PIC Act apply to assessments of permanent impairment conducted on or after 1 March 2021.
When conducting a permanent impairment assessment in accordance with the Guidelines, assessors are required to use the version current at the time of the assessment.
1.3 The Guidelines are based on a template that was developed through a national process facilitated by Safe Work Australia. The template national guideline is based on similar guidelines developed and used extensively in the NSW workers compensation system. Consequently, provisions in the Guidelines are the result of extensive and in-depth deliberations by groups of medical specialists convened to review AMA5 in the Australian workers compensation context. In NSW it is a requirement under s377(2) of the WIMWC Act that the guidelines are developed in consultation with relevant medical colleges. The groups that contributed to the development of the Guidelines is acknowledged and recorded at Appendix 2. The template national guideline has been adopted for use in multiple Australian jurisdictions.
1.4 Use of the Guidelines is monitored by the jurisdictions that have adopted it. The Guidelines may be reviewed if significant anomalies or insurmountable difficulties in their use become apparent.
1.5 The Guidelines are intended to assist a suitably qualified and experienced medical practitioner in assessing a claimant’s degree of permanent impairment.
Part 2 - Principles of assessment
1.6 The following is a basic summary of some key principles of permanent impairment assessments:
a. Assessing permanent impairment involves clinical assessment of the claimant as they present on the day of assessment taking account the claimant’s relevant medical history and all available relevant medical information to determine:
- whether the condition has reached Maximum Medical Improvement (MMI)
- whether the claimant’s compensable injury/condition has resulted in an impairment
- whether the resultant impairment is permanent
- the degree of permanent impairment that results from the injury
- the proportion of permanent impairment due to any previous injury, pre-existing condition or abnormality,
- if any, in accordance with diagnostic and other objective criteria as outlined in these Guidelines.
b. Assessors are required to exercise their clinical judgement in determining a diagnosis when assessing permanent impairment and making deductions for pre-existing injuries/conditions.
c. In calculating the final level of impairment, the assessor needs to clarify the degree of impairment that results from the compensable injury/condition. Any deductions for pre-existing injuries/conditions are to be clearly identified in the report and calculated. If, in an unusual situation, a related injury/condition has not previously been identified, an assessor should record the nature of any previously unidentified injury/condition in their report and specify the causal connection to the relevant compensable injury or medical condition.
d. The referral for an assessment of permanent impairment is to make clear to the assessor the injury or medical condition for which an assessment is sought – see also paragraphs 1.43 and 1.44 in the Guidelines.
1.7 Medical assessors are expected to be familiar with chapters 1 and 2 of AMA5, in addition to the information in this introduction.
1.8 The degree of permanent impairment that results from the injury/condition must be determined using the tables, graphs and methodology given in the Guidelines and the AMA5, where appropriate.
1.9 The Guidelines may specify more than one method that assessors can use to establish the degree of a claimant’s permanent impairment. In that case, assessors should use the method that yields the highest degree of permanent impairment. (This does not apply to gait derangement – see paragraphs 3.5 and 3.10 in the Guidelines).
1.10 AMA5 is used for most body systems, with the exception of psychiatric and psychological disorders, chronic pain, and visual and hearing injuries.
1.11 AMA5 Chapter 14, on mental and behavioural disorders, has been omitted. The Guidelines contain a substitute chapter on the assessment of psychiatric and psychological disorders which was written by a group of Australian psychiatrists.
1.12 AMA5 Chapter 18, on pain, is excluded entirely at the present time. Conditions associated with chronic pain should be assessed on the basis of the underlying diagnosed condition, and not on the basis of the chronic pain. Where pain is commonly associated with a condition, an allowance is made in the degree of impairment assigned in the Guidelines. Complex regional pain syndrome should be assessed in accordance with Evaluation of permanent impairment arising from chronic pain in the Guidelines.
1.13 On the advice of medical specialists (ophthalmologists), assessments of visual injuries are conducted according to the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 4th Edition (AMA4).
1.14 The methodology for evaluating permanent impairment due to hearing loss is in Hearing Loss of the Guidelines, with some reference to AMA5 Chapter 11 (pp 245–251) and also the tables in the National Acoustic Laboratories (NAL) Report No. 118, Improved Procedure for Determining Percentage Loss of Hearing, January 1988.
1.15 Assessments are only to be conducted when the medical assessor considers that the degree of permanent impairment of the claimant is unlikely to improve further and has attained maximum medical improvement. This is considered to occur when the worker’s condition is well stabilised and is unlikely to change substantially in the next year with or without medical treatment.
1.16 If the medical assessor considers that the claimant’s treatment has been inadequate and maximum medical improvement has not been achieved, the assessment should be deferred and comment made on the value of additional or different treatment and/or rehabilitation – subject to paragraph 1.34 in the Guidelines.
1.17 Impairments arising from the same injury are to be assessed together. Impairments resulting from more than one injury arising out of the same incident are to be assessed together to calculate the degree of permanent impairment of the claimant.
1.18 The Combined Values Chart in AMA5 (pp 604–06) is used to derive a percentage of whole person impairment (WPI) that arises from multiple impairments. An explanation of the chart’s use is found on pp 9–10 of AMA5. When combining more than two impairments, the assessor should commence with the highest impairment and combine with the next highest and so on.
1.19 The exception to this rule is in the case of psychiatric or psychological injuries. Where applicable, impairments arising from primary psychological and psychiatric injuries are to be assessed separately from the degree of impairment that results from any physical injuries arising out of the same incident. The results of the two assessments cannot be combined.
1.20 In the case of a complex injury, where different medical assessors are required to assess different body systems, a ‘lead assessor’ should be nominated to coordinate and calculate the final degree of permanent impairment as a percentage of WPI resulting from the individual assessments.
1.21 Psychiatric and psychological injuries in the NSW workers compensation system are defined as primary psychological and psychiatric injuries in which work was found to be a substantial contributing factor.
1.22 A primary psychiatric condition is distinguished from a secondary psychiatric or psychological condition, which arises as a consequence of, or secondary to, another work related condition (eg depression associated with a back injury). No permanent impairment assessment is to be made of secondary psychiatric and psychological impairments. As referenced in section Multiple impairments, impairments arising from primary psychological and psychiatric injuries are to be assessed separately from the degree of impairment that results from physical injuries arising out of the same incident. The results of the two assessments cannot be combined.
1.23 AMA5 (p 11) states:
Given the range, evolution and discovery of new medical conditions, these Guidelines cannot provide an impairment rating for all impairments… In situations where impairment ratings are not provided, these Guidelines suggest that medical practitioners use clinical judgment, comparing measurable impairment resulting from the unlisted condition to measurable impairment resulting from similar conditions with similar impairment of function in performing activities of daily living.’ The assessor must stay within the body part/region when using analogy.The assessor’s judgment, based upon experience, training, skill, thoroughness in clinical evaluation, and ability to apply the Guidelines criteria as intended, will enable an appropriate and reproducible assessment to be made of clinical impairment.
1.24 Many tables in AMA5 (eg in the spine section) give class values for particular impairments, with a range of possible impairment values in each class. Commonly, the tables require the assessor to consider the impact of the injury or illness on activities of daily living (ADL) in determining the precise impairment value. The ADL which should be considered, if relevant, are listed in AMA5 Table 1–2 (p 4). The impact of the injury on ADL is not considered in assessments of the upper or lower extremities.
1.25 The assessment of the impact of the injury or condition on ADL should be verified, wherever possible, by reference to objective assessments – for example, physiotherapist or occupational therapist functional assessments and other medical reports.
1.26 Occasionally the methods of the Guidelines will result in an impairment value which is not a whole number (eg an assessment of peripheral nerve impairment in the upper extremity). All such values must be rounded to the nearest whole number before moving from one degree of impairment to the next (eg from finger impairment to hand impairment, or from hand impairment to upper extremity impairment) or from a regional impairment to a WPI. Figures should also be rounded before using the combination tables. This will ensure that the final WPI will always be a whole number. The usual mathematical convention is followed where rounding occurs – values less than 0.5 are rounded down to the nearest whole number and values of 0.5 and above are rounded up to the next whole number. The method of calculating levels of binaural hearing loss is shown in Hearing impairment, paragraph 9.15, Chapter 9 in the Guidelines.
1.27 The degree of permanent impairment resulting from pre-existing impairments should not be included in the final calculation of permanent impairment if those impairments are not related to the compensable injury. The assessor needs to take account of all available evidence to calculate the degree of permanent impairment that pre-existed the injury.
1.28 In assessing the degree of permanent impairment resulting from the compensable injury/condition, the assessor is to indicate the degree of impairment due to any previous injury, pre-existing condition or abnormality. This proportion is known as ‘the deductible proportion’ and should be deducted from the degree of permanent impairment determined by the assessor. For the injury being assessed, the deduction is 1/10th of the assessed impairment, unless that is at odds with the available evidence.
1.29 Assessments of permanent impairment are to be conducted without assistive devices, except where these cannot be removed. The assessor will need to make an estimate as to what is the degree of impairment without such a device, if it cannot be removed for examination purposes. Further details may be obtained in the relevant sections of the Guidelines.
1.30 Impairment of vision should be measured with the claimant wearing their prescribed corrective spectacles and/or contact lenses, if this was usual for them before the injury. If, as a result of the injury, the claimant has been prescribed corrective spectacles and/or contact lenses for the first time, or different spectacles and/or contact lenses than those prescribed pre-injury, the difference should be accounted for in the assessment of permanent impairment.
1.31 In circumstances where the treatment of a condition leads to a further, secondary impairment, other than a secondary psychological impairment, the assessor should use the appropriate parts of the Guidelines to evaluate the effects of treatment, and use the Combined Values Chart (AMA5, pp 604–06) to arrive at a final percentage of WPI.
1.32 Where the effective long-term treatment of an illness or injury results in apparent substantial or total elimination of the claimant’s permanent impairment, but the claimant is likely to revert to the original degree of impairment if treatment is withdrawn, the assessor may increase the percentage of WPI by 1%, 2% or 3%. This percentage should be combined with any other impairment percentage, using the Combined Values Chart. This paragraph does not apply to the use of analgesics or anti-inflammatory medication for pain relief.
1.33 Where a claimant has declined treatment which the assessor believes would be beneficial, the impairment rating should be neither increased nor decreased – see paragraph 1.35 for further details.
1.34 If the claimant has been offered, but has refused, additional or alternative medical treatment that the assessor considers likely to improve the claimant’s condition, the medical assessor should evaluate the current condition without consideration of potential changes associated with the proposed treatment. The assessor may note the potential for improvement in the claimant’s condition in the evaluation report, and the reasons for refusal by the claimant, but should not adjust the level of impairment on the basis of the claimant’s decision.
1.35 Similarly, if a medical assessor forms the opinion that the claimant’s condition is stable for the next year, but that it may deteriorate in the long term, the assessor should make no allowance for this deterioration.
1.36 AMA5 (p 19) states:
Consistency tests are designed to ensure reproducibility and greater accuracy. These measurements, such as one that checks the individual’s range of motion are good but imperfect indicators of people’s efforts. The assessor must use their entire range of clinical skill and judgment when assessing whether or not the measurements or test results are plausible and consistent with the impairment being evaluated. If, in spite of an observation or test result, the medical evidence appears insufficient to verify that an impairment of a certain magnitude exists, the assessor may modify the impairment rating accordingly and then describe and explain the reason for the modification in writing.
This paragraph applies to inconsistent presentation only.
1.37 As a general principle, the assessor should not order additional radiographic or other investigations purely for the purpose of conducting an assessment of permanent impairment.
1.38 However, if the investigations previously undertaken are not as required by the Guidelines, or are inadequate for a proper assessment to be made, the medical assessor should consider the value of proceeding with the evaluation of permanent impairment without adequate investigations.
1.39 In circumstances where the assessor considers that further investigation is essential for a comprehensive evaluation to be undertaken, and deferral of the evaluation would considerably inconvenience the claimant (eg when the claimant has travelled from a country region specifically for the assessment), the assessor may proceed to order the appropriate investigations provided that there is no undue risk to the claimant. The approval of the referring body for the additional investigation will be required to ensure that the costs of the test are met promptly.
Part 3 - Administrative process
1.40 An assessor will be a registered medical practitioner recognised as a medical specialist.
- ‘Medical practitioner’ means a person registered in the medical profession under the Health Practitioner Regulation National Law (NSW) No. 86a, or equivalent Health Practitioner Regulation National Law in their jurisdiction with theAustralian Health Practitioner Regulation Agency.
- ‘Medical specialist’ means a medical practitioner recognised as a specialist in accordance with the Health Insurance Regulations 1975, Schedule 4, Part 1, who is remunerated at specialist rates under Medicare.
The assessor will have qualifications, training and experience relevant to the body system being assessed. The assessor will have successfully completed requisite training in using the Guidelines for each body system they intend on assessing. They will be listed as a trained assessor of permanent impairment for each relevant body system(s) on the SIRA website.
1.41 An assessor may be one of the claimant’s treating practitioners or an assessor engaged to conduct an assessment for the purposes of determining the degree of permanent impairment.
1.42 Information for claimants regarding independent medical examinations and assessments of permanent impairment should be supplied by the referring body when advising of the appointment details.
1.43 On referral, the medical assessor should be provided with all relevant medical and allied health information, including results of all clinical investigations related to the injury/condition in question.
1.44 Most importantly, assessors must have available to them all information about the onset, subsequent treatment, relevant diagnostic tests, and functional assessments of the person claiming a permanent impairment. The absence of required information could result in an assessment being discontinued or deferred. AMA5 Chapter 1, Section 1.5 (p 10) applies to the conduct of assessments and expands on this concept.
1.45 The Guidelines and AMA5 indicate the information and investigations required to arrive at a diagnosis and to measure permanent impairment. Assessors must apply the approach outlined in the Guidelines.
Referrers must consult this publication to gain an understanding of the information that should be provided to the assessor in order to conduct a comprehensive evaluation of impairment.
1.46 A report of the evaluation of permanent impairment should be accurate, comprehensive and fair. It should clearly address the question(s) being asked of the assessor. In general, the assessor will be requested to address issues of:
- current clinical status, including the basis for determining maximum medical improvement
- the degree of permanent impairment that results from the injury/condition, and
- the proportion of permanent impairment due to any previous injury, pre-existing condition or abnormality, if applicable.
1.47 The report should contain factual information based on all available medical information and results of investigations, the assessor’s own history-taking and clinical examination. The other reports or investigations that are relied upon in arriving at an opinion should be appropriately referenced in the assessor’s report.
1.48 As the Guidelines are to be used to assess permanent impairment, the report of the evaluation should provide a rationale consistent with the methodology and content of the Guidelines. It should include a comparison of the key findings of the evaluation with the impairment criteria in the Guidelines. If the evaluation was conducted in the absence of any pertinent data or information, the assessor should indicate how the impairment rating was determined with limited data.
1.49 The assessed degree of impairment is to be expressed as a percentage of WPI.
1.50 The report should include a conclusion of the assessor, including the final percentage of WPI. This is to be included as the final paragraph in the body of the report, and not as a separate report or appendix. The report must include a copy of all calculations and a summary table. A template reporting format is provided in the WorkCover Guidelines on independent medical examinations and reports.
1.51 Reports are to be provided within 10 working days of the assessment being completed, or as agreed between the referrer and the assessor.
1.52 The degree of permanent impairment that results from the injury must be determined using the tables, graphs and methodology given in the Guidelines, as presented in the training in the use of the Guidelines and the applicable legislation. If it is not clear that a report has been completed in accordance with the Guidelines, clarification may be sought from the assessor who prepared the report.
1.53 An assessor who is identified as frequently providing reports that are not in accord with the Guidelines, or not complying with other service standards as set by SIRA, may be subject to SIRA performance monitoring procedures and be asked to show cause as to why their name should not be removed from the list of trained assessors on the SIRA website.
1.54 Assessors are referred to the Medical Board of Australia’s Good Medical Practice: A Code of Conduct for Doctors in Australia, 8.7 Medico-legal, insurance and other assessments.
1.55 Assessors are reminded that they have an obligation to act in an ethical, professional and considerate manner when examining a claimant for the determination of permanent impairment.
1.56 Effective communication is vital to ensure that the claimant is well informed and able to maximally cooperate in the process. Assessors should:
- ensure that the claimant understands who the assessor is and the assessor’s role in the evaluation
- ensure that the claimant understands how the evaluation will proceed
- take reasonable steps to preserve the privacy and modesty of the claimant during the evaluation
- not provide any opinion to the claimant about their claim.
1.57 Complaints received in relation to the behaviour of an assessor during an evaluation will be managed in accordance with the process outlined in the WorkCover Guidelines on independent medical examinations and reports and SIRA performance monitoring procedures.
1.58 Where there is a discrepancy or inconsistency between medical reports that cannot be resolved between the parties, the Personal Injury Commission has the jurisdiction to determine disputes about assessed degree of permanent impairment.
Footnotes
* As of 1 September 2015, the workers compensation insurance regulatory functions of WorkCover NSW have been assumed by the State Insurance Regulatory Authority (SIRA).
AMA5 Chapter 16 (p 433) applies to the assessment of permanent impairment of the upper extremities, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
2.1 The upper extremities are discussed in AMA5 Chapter 16 (pp 433–521). This chapter provides guidelines on methods of assessing permanent impairment involving these structures. It is a complex chapter that requires an organised approach with careful documentation of findings.
2.2 Evaluation of anatomical impairment forms the basis for upper extremity impairment (UEI) assessment. The rating reflects the degree of impairment and its impact on the ability of the person to perform ADL. There can be clinical conditions where evaluation of impairment may be difficult. Such conditions are evaluated by their effect on function of the upper extremity, or, if all else fails, by analogy with other impairments that have similar effects on upper limb function.
The approach to assessment of the upper extremity and hand
2.3 Assessment of the upper extremity mainly involves clinical evaluation. Cosmetic and functional evaluations are performed in some situations. The impairment must be permanent and stable. The claimant will have a defined diagnosis that can be confirmed by examination.
2.4 The assessed impairment of a part or region can never exceed the impairment due to amputation of that part or region. For an upper limb, therefore, the maximum evaluation is 60% whole person impairment (WPI), the value for amputation through the shoulder.
2.5 Range of motion (ROM) is assessed as follows:
- A goniometer or inclinometer must be used, where clinically indicated.
- Passive ROM may form part of the clinical examination to ascertain clinical status of the joint, but impairment should only be calculated using active ROM measurements. Impairment values for degree measurements falling between those listed must be adjusted or interpolated.
- If the assessor is not satisfied that the results of a measurement are reliable, repeated testing may be helpful in this situation.
- If there is inconsistency in ROM, then it should not be used as a valid parameter of impairment evaluation. Refer to paragraph 1.36 in the Introduction.
- If ROM measurements at examination cannot be used as a valid parameter of impairment evaluation, the assessor should then use discretion in considering what weight to give other available evidence to determine if an impairment is present.
2.6 To achieve an accurate and comprehensive assessment of the upper extremity, findings should be documented on a standard form. AMA5 Figures 16-1a and 16-1b (pp 436–37) are extremely useful both to document findings and to guide the assessment process.
2.7 The hand and upper extremity are divided into regions: thumb, fingers, wrist, elbow and shoulder. Close attention needs to be paid to the instructions in AMA5 Figures 16-1a and 16-1b (pp 436–37) regarding adding or combining impairments.
2.8 AMA5 Table 16-3 (p 439) is used to convert upper extremity impairment to WPI. When the Combined Values Chart is used, the assessor must ensure that all values combined are in the same category of impairment (that is WPI, upper extremity impairment percentage, hand impairment percentage and so on). Regional impairments of the same limb (eg several upper extremity impairments) should be combined before converting to percentage WPI. (Note that impairments relating to the joints of the thumb are added rather than combined – AMA5 Section 16.4d ‘Thumb ray motion impairment’, p 454.)
Specific interpretation of AMA5 - the hand and upper extremity impairment of the upper extremity due to peripheral nerve disorders
2.9 If an upper extremity impairment results solely from a peripheral nerve injury, the assessor should not also evaluate impairment(s) from AMA5 Section 16.4 ‘Abnormal motion’ (pp 450–79) for that upper extremity. AMA5 Section 16.5 should be used for evaluating such impairments.
For evaluating peripheral nerve lesions, use AMA5 Table 16-15 (p 492) together with AMA5 tables 16-10 and 16-11 (pp 482 and 484).
The assessment of carpal tunnel syndrome post-operatively is undertaken in the same way as assessment without operation.
2.10 When applying AMA5 tables 16-10 (p 482) and 16-11 (pp 482 and 484) the examiner must use clinical judgement to estimate the appropriate percentage within the range of values shown for each severity grade. The maximum value is not applied automatically.
Impairment due to other disorders of the upper extremity
2.11 AMA5 Section 16.7 ‘Impairment of the upper extremity due to other disorders’ (pp 498–507) should be used only when other criteria (as presented in AMA5 sections 16.2–16.6, pp 441–98) have not adequately encompassed the extent of the impairments. Impairments from the disorders considered in AMA5 Section 16.7 are usually estimated using other criteria. The assessor must take care to avoid duplication of impairments.
2.12 AMA5 Section 16.7 (impairment of the upper extremities due to other disorders) notes ‘the severity of impairment due to these disorders is rated separately according to Table 16-19 through 16-30 and then multiplied by the relative maximum value of the unit involved, as specified in Table 16-18’. This statement should not include tables 16-25 (carpal instability), 16-26 (shoulder instability) and 16-27 (arthroplasty), noting that the information in these tables is already expressed in terms of upper extremity impairment.
2.13 Strength evaluation, as a method of upper extremity impairment assessment, should only be used in rare cases and its use justified when loss of strength represents an impairing factor not adequately considered by more objective rating methods. If chosen as a method, the caveats detailed on AMA5 p 508 under the heading ‘16.8a Principles’ need to be observed – ie decreased strength cannot be rated in the presence of decreased motion, painful conditions, deformities and absence of parts (eg thumb amputation).
Conditions affecting the shoulder region
2.14 Most shoulder disorders with an abnormal range of movement are assessed according to AMA5 Section 16.4 ‘Evaluating abnormal motion’. (Please note that AMA5 indicates that internal and external rotation of the shoulder are to be measured with the arm abducted in the coronal plane to 90 degrees, and with the elbow flexed to 90 degrees. In those situations where abduction to 90 degrees is not possible, symmetrical measurement of rotation is to be carried out at the point of maximal abduction.)
Rare cases of rotator cuff injury, where the loss of shoulder motion does not reflect the severity of the tear, and there is no associated pain, may be assessed according to AMA5 Section 16.8c ‘Strength evaluation’. Other specific shoulder disorders where the loss of shoulder motion does not reflect the severity of the disorder, associated with pain, should be assessed by comparison with other impairments that have similar effect(s) on upper limb function.
As noted in AMA5 Section 16.7b ‘Arthroplasty’, ‘In the presence of decreased motion, motion impairments are derived separately and combined with the arthroplasty impairment’. This includes those arthroplasties in AMA5 Table 16-27 designated as (isolated).
Please note that in AMA5 Table 16-27 (p 506) the figure for resection arthroplasty of the distal clavicle (isolated) has been changed to 5% upper extremity impairment, and the figure for resection arthroplasty of the proximal clavicle (isolated) has been changed to 8% upper extremity impairment.
Please note that in AMA5 Table 16-18 (p 499) the figures for impairment suggested for the sternoclavicular joint have been changed from 5% upper extremity impairment and 3% whole person impairment, to 25% upper extremity impairment and 15% whole person impairment.
2.15 Ruptured long head of biceps shall be assessed as an upper extremity impairment (UEI) of 3%UEI or 2%WPI where it exists in isolation from other rotator cuff pathology. Impairment for ruptured long head of biceps cannot be combined with any other rotator cuff impairment or with loss of range of movement.
2.16 Diagnosis of impingement is made on the basis of positive findings on appropriate provocative testing and is only to apply where there is no loss of range of motion. Symptoms must have been present for at least 12 months. An impairment rating of 3% UEI or 2% WPI shall apply.
Fractures involving joints
2.17 Displaced fractures involving joint surfaces are generally to be rated by range of motion. If, however, this loss of range is not sufficient to give an impairment rating, and movement is accompanied by pain and there is 2mm or more displacement, allow 2% UEI (1% WPI).
Epicondylitis of the elbow
2.18 This condition is rated as 2% UEI (1% WPI). In order to assess impairment in cases of epicondylitis, symptoms must have been present for at least 18 months. Localised tenderness at the epicondyle must be present and provocative tests must also be positive. If there is an associated loss of range of movement, these figures are not combined, but the method giving the highest rating is used.
Resurfacing procedures
2.19 No additional impairment is to be awarded for resurfacing procedures used in the treatment of localised cartilage lesions and defects in major joints.
Calculating motion impairment
2.20 When calculating impairment for loss of range of movement, it is most important to always compare measurements of the relevant joint(s) in both extremities. If a contralateral ‘normal/uninjured’ joint has less than average mobility, the impairment value(s) corresponding to the uninvolved joint serves as a baseline and is subtracted from the calculated impairment for the involved joint. The rationale for this decision should be explained in the assessor’s report (see AMA5 Section 16.4c, p 543).
Complex regional pain syndrome (upper extremity)
2.21 Complex regional pain syndrome types 1 and 2 should be assessed using the method in Chapter 17 of the Guidelines.
AMA5 Chapter 17 (p 523) applies to the assessment of permanent impairment of the lower extremities, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
3.1 The lower extremities are discussed in AMA5 Chapter 17 (pp 523–564). This section is complex and provides a number of alternative methods of assessing permanent impairment involving the lower extremity. An organised approach is essential.
The approach to assessment of the lower extremity
3.2 Assessment of the lower extremity involves physical evaluation, which can use a variety of methods. In general, the method should be used that most specifically addresses the impairment present. For example, impairment due to a peripheral nerve injury in the lower extremity should be assessed with reference to that nerve rather than by its effect on gait.
3.3 There are several different forms of evaluation that can be used, as indicated inAMA5 sections 17.2b to 17.2n (pp 528–54). AMA5 Table 17-2 (p 526) indicates which evaluation methods can be combined and which cannot. It may be possible to perform several different evaluations, as long as they are reproducible and meet the conditions specified below and in AMA5. The most specific method of impairment assessment should be used. (Please note that in Table 17-2, the boxes in the fourth row (on muscle strength) and seventh column (on amputation) should be closed boxes [x] rather than open boxes [ ].)
3.4 It is possible to use an algorithm to aid in the assessment of lower extremity impairment (LEI). Use of a worksheet is essential. Table 3.5 at the end of this chapter is such a worksheet and may be used in assessment of permanent impairment of the lower extremity.
3.5 In the assessment process, the evaluation giving the highest impairment rating is selected. That may be a combined impairment in some cases, in accordance with the AMA5 Table 17-2 ‘Guide to the appropriate combination of evaluation methods’, using the Combined Values Chart on pp 604–06 of AMA5.
3.6 When the Combined Values Chart is used, the assessor must ensure that all values combined are in the same category of impairment rating (ie percentage of WPI, percentage of lower extremity impairment, foot impairment percentage, and so on). Regional impairments of the same limb (eg several lower extremity impairments) should be combined before converting to a percentage of whole person impairment (WPI).
3.7 AMA5 Table 17-2 (p 526) AMA5) needs to be referred to frequently to determine which impairments can be combined and which cannot. The assessed impairment of a part or region can never exceed the impairment due to amputation of that part or region. For the lower limb, therefore, the maximum evaluation is 40% WPI, the value for proximal above-knee amputation.
Specific interpretation of AMA5 – the lower extremity
3.8 When true leg length discrepancy is determined clinically (see AMA5 Section 17.2b, p 528), the method used must be indicated (eg tape measure from anterior superior iliac spine to the medial malleolus). Clinical assessment of leg length discrepancy is an acceptable method, but if full-length computerised tomography films are available, they should be used in preference. Such an examination should not be ordered solely for determining leg lengths.
3.9 Note that the figures for lower limb impairment in AMA5 table 17-4 (p 528) are incorrect. The correct figures are shown below.
AMA5 Table 17-4: Impairment due to limb length discrepancy
| Discrepancy (cm) | Whole person (lower extremity) impairment (%) |
|---|---|
| 0-1.9 | 0 |
| 2-2.9 | 3 (8) |
| 3-3.9 | 5 (13) |
| 4-4.9 | 7 (18) |
| 5+ | 8 (19) |
3.10 Assessment of gait derangement is only to be used as a method of last resort. Methods of impairment assessment most fitting the nature of the disorder should always be used in preference. If gait derangement (AMA5 Section 17.2c, p 529) is used, it cannot be combined with any other evaluation in the lower extremity section of AMA5.
3.11 Any walking aid used by the subject must be a permanent requirement and not temporary.
3.12 In the application of AMA5 Table 17-5 (p 529), delete item ‘b’, as the Trendelenburg sign is not sufficiently reliable.
3.13 AMA5 Section 17.2d (p 530) is not applicable if the limb other than that being assessed is abnormal (eg if varicose veins cause swelling, or if there is another injury or condition which has contributed to the disparity in size).
3.14 Note that the figures for lower limb impairment given in AMA5 Table 17-6 (p 530) are incorrect. The correct figures are shown below.
AMA5 Table 17-6: Impairment due to unilateral leg muscle atrophy
| Difference in circumference (cm) | Impairment degree | Whole person (lower extremity) impairment (%) |
|---|---|---|
| a. Thigh: The circumference is measured 10cm above the patella, with the knee fully extended and the muscles relaxed. | ||
| 0-0.9 | None | 0 (0) |
| 1-1.9 | Mild | 2 (6) |
| 2-2.9 | Moderate | 4 (11) |
| 3+ | Severe | 5 (12) |
| Difference in circumference (cm) | Impairment degree | Whole person (lower extremity) impairment (%) |
|---|---|---|
| b. Calf: The maximum circumference on the normal side is compared with the circumference at the same level on the affected side. | ||
| 0-0.9 | None | 0 (0) |
| 1-1.9 | Mild | 2 (6) |
| 2-.29 | Moderate | 4 (11) |
| 3+ | Severe | 5 (12) |
3.15 The Medical Research Council gradings for muscle strength are universally accepted. They are not linear in their application, but ordinal. Only the six grades (0–5) should be used, as they are reproducible among experienced assessors. The descriptions in AMA5 Table 17-7 (p 531) are correct. The results of electrodiagnostic methods and tests are not to be considered in evaluating muscle testing, which can be performed manually. AMA5 Table 17-8 (p 532) is to be used for this method of evaluation.
3.16 Although range of motion (ROM) appears to be a suitable method for evaluating impairment (see AMA5 Section 17.2f, pp 533–38), it may be subject to variation because of pain during motion at different times of examination, possible lack of cooperation by the person being assessed and inconsistency. If there is such inconsistency, then ROM cannot be used as a valid parameter of impairment evaluation.
AMA5 Table 17-10 (p 537) is misleading as it has valgus and varus deformity in the same table as restriction of movement, possibly suggesting that these impairments may be combined. This is not the case. Any valgus/ varus deformity present which is due to the underlying lateral or medial compartment arthritis, cannot be combined with loss of range of movement. Therefore, when faced with an assessment in which there is a rateable loss of range of movement as well as a rateable deformity, calculate both impairments and use the greater. Valgus and varus knee angulation are to be measured in a weight-bearing position using a goniometer. It is important to bear in mind that valgus and/or varus alignments of the knee may be constitutional. It is also important to always compare with the opposite knee.
3.17 If range of motion is used as an assessment measure, then AMA5 Tables 17-9 to 17 14 (p 537) are selected for the joint or joints being tested. If a joint has more than one plane of motion, the impairment assessments for the different planes should be added. For example, any impairment of the six principal directions of motion of the hip joint are added (see AMA5, p 533).
In AMA5 Table 17-10 (p 537), on knee impairment, the sentence should read: ‘Deformity measured by femoral-tibial angle; 3° to 9° valgus is considered normal’.
In AMA5 Table 17-11 (ankle motion) the range for mild flexion contracture should be one to 10°, for moderate flexion contracture it should be 11° to 19°, and for severe flexion contracture it should be 20° plus.
The revised Table 17-11 is below.
AMA5 Table 17-11: Ankle motion impairment estimates
| Whole person (lower extremity) [foot] impairment | |||
|---|---|---|---|
| Motion | Mild 3% (7%) [10%] | Moderate 6% (15%) [21%] | Severe 12% (30%) [43%] |
| Plantar flexion capability | 11°-20° | 1°-10° | None |
| Flexion contracture | 1°-10° | 11°-19° | 20°+ |
| Extension | 10°-0° (neutral) | - | - |
When calculating impairment for loss of range of movement, it is most important to always compare measurements of the relevant joint(s) in both extremities. If a contralateral ‘normal/uninjured’ joint has less than average mobility, the impairment value(s) corresponding to the uninvolved joint serves as a baseline, and is subtracted from the calculated impairment for the involved joint. The rationale for this decision should be explained in the assessor’s report (see AMA5 Section 16.4c, p 454).
3.18 Ankylosis is to be regarded as the equivalent to arthrodesis in impairment terms only. For the assessment of impairment, when a joint is ankylosed (AMA5 section 17.2g, pp 538-543), the calculation to be applied is to select the impairment if the joint is ankylosed in optimum position (see table 3.1 below), and then if not ankylosed in the optimum position, by adding (not combining) the values of percentage of WPI using tables 17-15 to 17-30 (pp 538-543 AMA5).
Table 3.1: Impairment for ankylosis in the optimum position
| Joint | Whole person % | Lower extremity % | Ankle or foot % |
|---|---|---|---|
| Hip | 20 | 50 | - |
| Knee | 27 | 67 | - |
| Pantalar | 19 | 47 | 67 |
| Ankle | 15 | 37 | 53 |
| Triple | 6 | 15 | 21 |
| Subtalar | 4 | 10 | 14 |
Note that the figures in Table 3.1 suggested for ankle impairment are greater than those suggested in AMA5.
Ankylosis of the ankle in the neutral/optimal position equates with 15 (37) [53]% impairment as per Table 3.1. Table 3.1(a) is provided below as a guide to evaluate additional impairment owing to variation from the neutral position. The additional amounts at the top of each column are added to the figure for impairment in the neutral position. In keeping with the value given on page 541 of AMA5, the maximum impairment for ankylosis of the ankle remains at 25 (62) [88]% impairment.
Table 3.1(a): Impairment for ankylosis in variation from the optimum position
| Whole person (lower extremity) [foot] impairment | ||||
|---|---|---|---|---|
| Position | 2 (5) [7]% | 4 (10) [14]% | 7 (17) [24]% | 10 (25) [35]% |
| Dorsiflexion | 5°-9° | 10°-19° | 20°-29° | 30°+ |
| Plantar flexion | - | 10°-19° | 20°-29° | 30°+ |
| Varus | 5°-9° | 10°-19° | 20°-29° | 30°+ |
| Valgus | - | 10°-19° | 20°-29° | 30°+ |
| Internal rotation | 0°-9° | 10°-19° | 20°-29° | 30°+ |
| External rotation | 15°-19° | 20°-29° | 30°-39° | 40°+ |
3.19 Impairment due to arthritis (AMA5 Section 17.2n, pp 544–45) following a work-related injury is uncommon, but may occur in isolated cases. The presence of arthritis may indicate a pre-existing condition and this should be assessed and an appropriate deduction made (see Chapter 1).
3.20 The presence of osteoarthritis is defined as cartilage loss. Cartilage loss can be measured by properly aligned plain X-ray, or by direct vision (arthroscopy), but impairment can only be assessed according to the radiologically determined cartilage loss intervals shown in AMA5 Table 17-31 (p 544). When assessing impairment of the knee joint, which has three compartments, only the compartment with the major impairment is used in the assessment. That is, measured impairments in the different compartments cannot be added or combined.
3.21 Detecting the subtle changes of cartilage loss on plain radiography requires comparison with the normal side. All joints should be imaged directly through the joint space, with no overlapping of bones. If comparison views are not available, AMA5 Table 17-31 (p 544) is used as a guide to assess joint space narrowing.
3.22 One should be cautious in making a diagnosis of cartilage loss on plain radiography if secondary features of osteoarthritis, such as osteophytes, subarticular cysts or subchondral sclerosis are lacking, unless the other side is available for comparison. The presence of an intra-articular fracture with a step in the articular margin in the weight-bearing area implies cartilage loss.
3.23 The accurate radiographic assessment of joints always requires at least two views. In some cases, further supplementary views will optimise the detection of joint space narrowing or the secondary signs of osteoarthritis.
Sacro-iliac joint: Being a complex joint, modest alterations are not detected on radiographs, and cross sectional imaging may be required. Radiographic manifestations accompany pathological alterations. The joint space measures between 2mm and 5mm. Osteophyte formation is a prominent characteristic of osteoarthritis of the sacro-iliac joint.
Hip: An anteroposterior view of the pelvis and a lateral view of the affected hip are ideal. If the affected hip joint space is narrower than the asymptomatic side, cartilage loss is regarded as being present. If the anteroposterior view of the pelvis has been obtained with the patient supine, it is important to compare the medial joint space of each hip, as well as superior joint space, as this may be the only site of apparent change. If both sides are symmetrical, then other features, such as osteophytes, subarticular cyst formation, and calcar thickening, should be taken into account to make a diagnosis of osteoarthritis.
Knee – Tibio-femoral joint: The best view for assessment of cartilage loss in the knee is usually the erect intercondylar projection, as this profiles and stresses the major weight-bearing area of the joint, which lies posterior to the centre of the long axis. The ideal X-ray is a posteroanterior view, with the patient standing, knees slightly flexed, and the X-ray beam angled parallel to the tibial plateau (Rosenberg view). Both knees can be readily assessed with the one exposure. It should be recognised that joint space narrowing in the knee does not necessarily equate with articular cartilage loss, as deficiency or displacement of the menisci can also have this effect. Secondary features, such as subchondral bone change and past surgical history, must also be taken into account.
Knee – Patello-femoral joint: This should be assessed in the ‘skyline’ view, again preferably with the other side for comparison. The X-ray should be taken with 30 degrees of knee flexion to ensure that the patella is load-bearing and has engaged the articular surface femoral groove.
- Footnote to AMA5 Table 17-31 (p 544) regarding patello-femoral pain and crepitation:
- This item is only to be used if there is a history of direct injury to the front of the knee, or in cases of patellar translocation/dislocation without direct anterior trauma. This item cannot be used as an additional impairment when assessing arthritis of the knee joint itself, of which it forms a component. If patello-femoral crepitus occurs in isolation (ie with no other signs of arthritis) following either of the above, then it can be combined with other diagnosis-based estimates (AMA5 Table 17-33, p 546). Signs of crepitus need to be present at least one year post-injury.
- Note: Osteoarthritis of the patello-femoral joint cannot be used as an additional impairment when assessing arthritis of the knee joint itself, of which it forms a component.
Ankle: The ankle should be assessed in the mortice view (preferably weight-bearing), with comparison views of the other side, although this is not as necessary as with the hip and knee.
Subtalar: This joint is better assessed by CT (in the coronal plane) than by plain radiography. The complex nature of the joint does not lend itself to accurate and easy plain X-ray assessment of osteoarthritis.
Talonavicular and calcaneocuboid: Anteroposterior and lateral views are necessary. Osteophytes may assist in making the diagnosis.
Intercuneiform and other intertarsal joints: Joint space narrowing may be difficult to assess on plain radiography. CT (in the axial plane) may be required. Associated osteophytes and subarticular cysts are useful adjuncts to making the diagnosis of osteoarthritis in these small joints.
Great toe metatarsophalangeal: Anteroposterior and lateral views are required. Comparison with the other side may be necessary. Secondary signs may be useful.
Interphalangeal: It is difficult to assess small joints without taking secondary signs into account. The plantar-dorsal view may be required to get through the joints, in a foot with flexed toes.
3.24 If arthritis is used as the basis for assessing impairment, then the rating cannot be combined with gait disturbance, muscle atrophy, muscle strength or range of movement assessments. It can be combined with a diagnosis-based estimate (AMA5 Table 17-2, p 526).
3.25 Where there has been amputation of part of a lower extremity Table 17-32 (p 545, AMA5) applies. In that table, the references to three inches for below the knee amputation should be converted to 7.5cm.
3.26 AMA5 Section 17.2j (pp 545–49) lists a number of conditions that fit a category of diagnosis-based estimates. They are listed in AMA5 Tables 17-33, 17-34 and 17-35 (pp 546–49). When using this table it is essential to read the footnotes carefully. The category of mild cruciate and collateral ligament laxity has inadvertently been omitted in Table 17-33. The appropriate rating is 5 (12)% whole person (lower extremity) impairment.
3.27 It is possible to combine impairments from Tables 17-33, 17-34 and 17-35 for diagnosis-related estimates with other components (eg nerve injury) using the Combined Values Chart (AMA5, pp 604–06) after first referring to the Guidelines for the appropriate combination of evaluation methods (see Table 3.5).
3.28 Pelvic fractures: Pelvic fractures are to be assessed as per Table 4.3 in Chapter 4 the Guidelines, and not as per AMA5 Table 17-33 (p 546).
Hip: The item in relation to femoral neck fracture ‘malunion’ is not to be used in assessing impairment. Use other available methods.
Femoral osteotomy:
- Good result: 10 (25)
- Poor result: Estimate according to examination and arthritic degeneration
Tibial plateau fractures: Table 3.2 of the Guidelines (below), replaces the instructions for tibial plateau fractures in AMA5 Table 17-33 (p 546).
Table 3.2: Impairment for tibial plateau fractures
In deciding whether the fracture falls into the mild, moderate or severe categories, the assessor must take into account:
- the extent of involvement of the weight-bearing area of the tibial plateau
- the amount of displacement of the fracture(s)
- the amount of comminution present.
| Grade | Whole person (lower extremity) impairment (%) |
|---|---|
| Undisplaced | 2 (5) |
| Mild | 5 (12) |
| Moderate | 10 (25) |
| Severe | 15 (37) |
Patello-femoral joint replacement: Assess the knee impairment in the usual way and combine with 9% WPI (22% LEI) for isolated patello-femoral joint replacement.
Total ankle replacement:
Table 3.3: Rating for ankle replacement results
The points system for rating total ankle replacements is to be the same as for total hip and total knee replacements, with the following impairment ratings:
| Result | WPI (LEI) % |
|---|---|
| Good result: 85–100 points: | 12 (30) |
| Fair result: 50–84 points: | 16 (40) |
| Poor result: <50 points: | 20 (50) |
| Number of points | ||
|---|---|---|
| a. Pain | ||
| None | 50 | |
| Slight | ||
| Stairs only | 40 | |
| Walking and stairs | 30 | |
| Moderate | ||
| Occasional | 20 | |
| Continual | 10 | |
| Severe | 0 | |
| b. Range of motion | ||
| i. Flexion | ||
| > 20° | 15 | |
| 11° - 20° | 10 | |
| 5° - 10° | 5 | |
| < 5° | 0 | |
| ii. Extension: | ||
| > 10° | 10 | |
| 5° - 10° | 5 | |
| < 5° | 0 | |
| c. Range of motion | ||
| i. Limp | ||
| None | 10 | |
| Slight | 7 | |
| Moderate | 4 | |
| Severe | 0 | |
| ii. Supportive device | ||
| None | 5 | |
| Cane | 3 | |
| One crutch | 1 | |
| Two crutches | 0 | |
| iii. Distance walked | ||
| Unlimited | 5 | |
| Six blocks | 4 | |
| Three blocks | 3 | |
| Indoors | 2 | |
| Bed or chair | 0 | |
| iv. Stairs | ||
| Normal | 5 | |
| Using rail | 4 | |
| One at a time | 2 | |
| Unable to climb | 0 | |
| Sub-total: | ||
| Deductions (minus) d and e | Number of points |
|---|---|
| d. Varus | |
| < 5° | 0 |
| 5° - 10° | 10 |
| > 10° | 15 |
| e. Valgus | |
| < 5° | 0 |
| 5° - 10° | 10 |
| > 10° | 15 |
| Sub-total: | |
Tibia-os calcis angle: The table given below for the impairment of loss of the tibia-os calcis angle is to replace AMA5 Table 17-29 (p 542) and the section in AMA5 Table 17-3 (p 546) dealing with loss of tibia-os calcis angle. These two sections are contradictory, and neither gives a full range of loss of angle.
Table 3.4 Impairment for loss of the tibia-os calcis angle
| Angle (degree) | Whole person (lower extremity) [foot] impairment (%) |
|---|---|
| 110-100 | 5 (12) [17] |
| 99-90 | 8 (20) [28] |
| <90 | +1 (2) [3] per degree, up to 15 (37) [54] |
Hindfoot intra-articular fractures: In the interpretation of AMA5 Table 17-33 (p 547, AMA5), reference to the hindfoot, intra-articular fractures, the words subtalar bone, talonavicular bone, and calcaneocuboid bone imply that the bone is displaced on one or both sides of the joint mentioned. To avoid the risk of double assessment, if avascular necrosis with collapse is used as the basis of impairment assessment, it cannot be combined with the relevant intra-articular fracture in Table 17-33, column 2. In Table 17-33, column 2, metatarsal fracture with loss of weight transfer means dorsal displacement of the metatarsal head.
Plantar fasciitis: If there are persistent symptoms and clinical findings after 18 months, this is rated as 2% LEI (1% WPI).
Resurfacing procedures: No additional impairment is to be awarded for resurfacing procedures used in the treatment of localised cartilage lesions and defects in major joints.
3.29 AMA5 tables 17-34 and 17-35 (pp 548–49) use a different concept of evaluation. A point score system is applied, and then the total points calculated for the hip (or knee) joint are converted to an impairment rating from Table 17-33. Tables 17-34 and 17-35 refer to hip and knee joint replacements respectively. Note that, while all the points are added in Table 17-34, some points are deducted when Table 17-35 is used. (Note that hemiarthroplasty rates the same as total joint replacement.)
3.30 In respect of ‘distance walked’ under ‘b. Function’ in AMA5 Table 17-34 (p 548), the distance of six blocks should be construed as 600 metres, and three blocks as 300 metres.
Note that AMA5 Table 17-35 (p 549) is incorrect. The correct table is shown below:
AMA5 Table 17-35: Rating knee replacement results
| Number of points | ||
|---|---|---|
| a. Pain | ||
| None | 50 | |
| Mild or occasional | 45 | |
| Stairs only | 40 | |
| Walking and stairs | 30 | |
| Moderate | ||
| Occasional | 20 | |
| Continual | 10 | |
| Severe | 0 | |
| b. Range of motion | ||
| Add 1 point per 5° up to 125° | 25 (maximum) | |
| c. Stability (maximum movement in any position) | ||
| Anterioposterior | ||
| < 5mm | 10 | |
| 5 - 9mm | 5 | |
| > 9mm | 0 | |
| Mediolateral | ||
| 5° | 15 | |
| 6° - 9° | 10 | |
| 10° - 14° | 5 | |
| > 14° | 0 | |
| Sub-total: | ||
| Deductions (minus) d, e, f | Number of points |
|---|---|
| d. Flexion contracture | |
| 5° - 9° | 2 |
| 10° - 15° | 5 |
| 16° - 20° | 10 |
| > 20° | 20 |
| e. Extension lag | |
| < 10° | 5 |
| 10° - 20° | 10 |
| > 20° | 15 |
| f. Tibio-femoral alignment* | |
| > 15° valgus | 20 |
| 11° - 15° valgus | 3 points per degree |
| 5° - 10° valgus | 0 |
| 0° - 4° valgus | 3 points per degree |
| Any varus | 20 |
| Deductions sub-total: | |
* Refer to the unaffected limb to take into account any constitutional variation.
3.32 When assessing the impairment due to peripheral nerve injury (AMA5, pp 550–52) assessors should read the text in this section. Note that separate impairments for the motor, sensory and dysaesthetic components of nerve dysfunction in AMA5 Table 17-37 (p 552) are to be combined.
3.33 Note that the (posterior) tibial nerve is not included in Table 17-37, but its contribution can be calculated by subtracting ratings of common peroneal nerves from sciatic nerve ratings.
3.34 Peripheral nerve injury impairments can be combined with other impairments, but not those for gait derangement, muscle atrophy, muscle strength or complex regional pain syndrome, as shown in AMA5 Table 17-2 (p 526). Motor and sensory impairments given in Table 17-37 are for complete loss of function and assessors must still use Table 16-10 and 16-11 in association with Table 17-37.
3.35 Complex regional pain syndrome types 1 and 2 are to be assessed using the method in Chapter 17 of the Guidelines.
3.36 Lower extremity impairment due to vascular disorders (AMA5, pp 553–54) is evaluated using AMA5 Table 17-38 (p 554). Note that Table 17-38 gives values for lower extremity impairment, not WPI. In that table, there is a range of lower extremity impairments within each of the classes 1 to 5. As there is a clinical description of which conditions place a person’s lower extremity in a particular class, the assessor has a choice of impairment rating within a class, the value of which is left to the clinical judgement of the assessor.
3.37 When measuring dorsiflexion at the ankle, the test is carried out initially with the knee in extension and then repeated with the knee flexed to 45 degrees. The average of the maximum angles represents the dorsiflexion range of motion (AMA5 Figure 17-5, p 535).
Table 3.5: Lower extremity worksheet
| Item | Impairment | AMA5 table | AMA5 page | Potential impairment | Selected impairment |
|---|---|---|---|---|---|
| 1 | Limb length discrepancy | 17-4 | 528 | ||
| 2 | Gait derangement | 17-5 | 529 | ||
| 3 | Unilateral muscle atrophy | 17-6 | 530 | ||
| 4 | Muscle weakness | 17-8 | 532 | ||
| 5 | Range of motion | 17-9 to 17-14 | 537 | ||
| 6 | Joint ankylosis | 17-15 to 17-30 | 538-543 | ||
| 7 | Arthritis | 17-31 | 544 | ||
| 8 | Amputation | 17-32 | 545 | ||
| 9 | Diagnosis-based estimates | 17-33 to 17-35 | 546-549 | ||
| 10 | Skin loss | 17-36 | 550 | ||
| 11 | Peripheral nerve deficit | 17-37 | 552 | ||
| 12 | Complex regional pain syndrome | Section 16.5e | 495-497 | ||
| 13 | Vascular disorder | 17-38 | 554 | ||
| Combined impairment rating (refer to AMA5 Table 17-2, p526 for permissible combinations) | |||||
Potential impairment is the impairment percentage for that method of assessment. Selected impairment is the impairment, or impairments selected, that can be legitimately combined with other lower extremity impairments to give a final lower extremity impairment rating.
AMA5 Chapter 15 (p 373) applies to the assessment of permanent impairment of the spine, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing.
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
- The Guidelines take precedence over AMA5.
Introduction
4.1 The spine is discussed in Chapter 15 of AMA5 (pp 373–431). That chapter presents two methods of assessment, the diagnosis-related estimates method and the range of motion method. Evaluation of impairment of the spine is only to be done using diagnosis-related estimates (DREs).
4.2 The DRE method relies especially on evidence of neurological deficits and less common, adverse structural changes, such as fractures and dislocations. Using this method, DREs are differentiated according to clinical findings that can be verified by standard medical procedures.
4.3 The assessment of spinal impairment is made when the person’s condition has stabilised and has reached maximum medical improvement. This is considered to occur when the worker’s condition is well stabilised and unlikely to change substantially in the next year, with or without medical treatment. If surgery has been performed, the outcome of the surgery as well as structural inclusions must be taken into consideration when making the assessment.
Assessment of the spine
4.4 The assessment should include a comprehensive, accurate history, a review of all pertinent records available at the assessment, a comprehensive description of the individual’s current symptoms and their relationship to activities of daily living (ADL); a careful and thorough physical examination; and all findings of relevant laboratory, imaging, diagnostic and ancillary tests available at the assessment. Imaging findings that are used to support the impairment rating should be concordant with symptoms and findings on examination. The assessor should record whether diagnostic tests and radiographs were seen or whether they relied solely on reports.
4.5 The DRE model for assessment of spinal impairment should be used. The range of motion model (AMA5 sections 15.8–15.13 inclusive, pp 398–427) should not be used.
4.6 If a person has spinal cord or cauda equina damage, including bowel, bladder and/or sexual dysfunction, he or she is assessed according to the method described in AMA5 Section 15.7 and AMA5 Table 15.6 (a)–(g) (pp 395–98).
4.7 If an assessor is unable to distinguish between two DRE categories, then the higher of those two categories should apply. The reasons for the inability to differentiate should be noted in the assessor’s report.
4.8 Possible influence of future treatment should not form part of the impairment assessment. The assessment should be made on the basis of the person’s status at the time of interview and examination, if the assessor is convinced that the condition is stable and permanent. Likewise, the possibility of subsequent deterioration, as a consequence of the underlying condition, should not be factored into the impairment evaluation. Commentary can be made regarding the possible influence, potential or requirements for further treatment, but this does not affect the assessment of the individual at the time of impairment evaluation.
4.9 All spinal impairments are to be expressed as a percentage of WPI.
4.10 AMA5 Section 15.1a (pp 374–77) is a valuable summary of history and physical examination, and should be thoroughly familiar to all assessors.
4.11 The assessor should include in the report a description of how the impairment rating was calculated, with reference to the relevant tables and figures used.
4.12 The optimal method to measure the percentage compression of a vertebral body is a well-centred plain X-ray. Assessors should state the method they have used. The loss of vertebral height should be measured at the most compressed part and must be documented in the impairment evaluation report. The estimated normal height of the compressed vertebra should be determined, where possible, by averaging the heights of the two adjacent (unaffected and normal) vertebrae.
Specific interpretation of AMA5
4.13 The range-of-motion (ROM) method is not used, hence any reference to this is omitted (includingAMA5 Table 15-7, p 404).
4.14 Motion segment integrity alteration can be either increased translational or angular motion, or decreased motion resulting from developmental changes, fusion, fracture healing, healed infection or surgical arthrodesis. Motion of the individual spine segments cannot be determined by a physical examination, but is evaluated with flexion and extension radiography.
4.15 The assessment of altered motion segment integrity is to be based upon a report of trauma resulting in an injury, and not on developmental or degenerative changes.
4.16 When routine imaging is normal and severe trauma is absent, motion segment disturbance is rare. Thus, flexion and extension imaging is indicated only when a history of trauma or other imaging leads the physician to suspect alteration of motion segment integrity.
DRE definitions of clinical findings
4.17 The preferred method for recording ROM is as a fraction or percentage of the range or loss of the range. For example, either ‘cervical movement was one half (or 50%) of the normal range of motion’ or ‘there was a loss of one half (or 50%) of the normal range of movement of the cervical spine’.
4.18 DRE II is a clinical diagnosis based upon the features of the history of the injury and clinical features. Clinical features which are consistent with DRE II and which are present at the time of assessment include radicular symptoms in the absence of clinical signs (that is, non-verifiable radicular complaints), muscle guarding or spasm, or asymmetric loss of range of movement. Localised (not generalised) tenderness may be present. In the lumbar spine, additional features include a reversal of the lumbosacral rhythm when straightening from the flexed position and compensatory movement for an immobile spine, such as flexion from the hips. In assigning category DRE II, the assessor must provide detailed reasons why the category was chosen.
4.19 Asymmetric or non-uniform loss of ROM may be present in any of the three planes of spinal movement. Asymmetry during motion caused by muscle guarding or spasm is included in the definition.
Asymmetric loss of ROM may be present for flexion and extension. For example, if cervical flexion is half the normal range (loss of half the normal range) and cervical extension is one-third of the normal range (loss of two thirds of the range), asymmetric loss of ROM may be considered to be present.
4.20 While imaging and other studies may assist medical assessors in making a diagnosis, the presence of a morphological variation from ‘normal’ in an imaging study does not confirm the diagnosis. To be of diagnostic value, imaging studies must be concordant with clinical symptoms and signs. In other words, an imaging test is useful to confirm a diagnosis, but an imaging study alone is insufficient to qualify for a DRE category (excepting spinal fractures).
4.21 The clinical findings used to place an individual in a DRE category are described in AMA5 Box 15-1 (pp 382–83).
The reference to ‘electro-diagnostic verification of radiculopathy’ should be disregarded.
(The use of electro-diagnostic procedures such as electromyography is proscribed as an assessment aid for decisions about the category of impairment into which a person should be placed. It is considered that competent assessors can make decisions about which DRE category a person should be placed in from the clinical features alone. The use of electro-diagnostic differentiators is generally unnecessary).
4.22 The cauda equina syndrome is defined in Box 15.1 in Chapter 15 of AMA5 (p 383) as ‘manifested by bowel or bladder dysfunction, saddle anaesthesia and variable loss of motor and sensory function in the lower limbs’. For a cauda equina syndrome to be present there must be bilateral neurological signs in the lower limbs and sacral region. Additionally, there must be a radiological study which demonstrates a lesion in the spinal canal, causing a mass effect on the cauda equina with compression of multiple nerve roots. The mass effect would be expected to be large and significant. A lumbar MRI scan is the diagnostic investigation of choice for this condition. A cauda equina syndrome may occasionally complicate lumbar spine surgery when a mass lesion will not be present in the spinal canal on radiological examination.
4.23 The cauda equina syndrome and neurogenic bladder disorder are to be assessed by the method prescribed in the spine chapter of AMA5 Section 15.7 (pp 395–98). For an assessment of neurological impairment of bowel or bladder, there must be objective evidence of spinal cord or cauda equina injury.
Applying the DRE method
4.24 The specific procedures and directions section of AMA5 Section 15.2a (pp 380–81) indicates the steps that should be followed to evaluate impairment of the spine (excluding references to the ROM method). Table 4.1 below is a simplified version of that section, incorporating the amendments listed above.
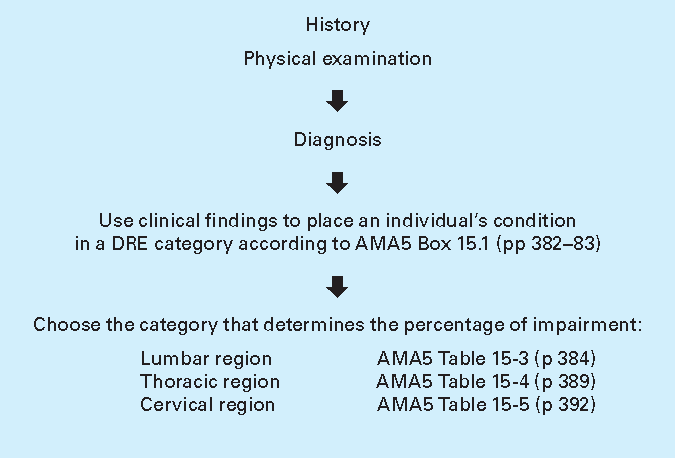
4.25 Common developmental findings, spondylosis, spondylolisthesis and disc protrusions without radiculopathy occur in 7%, 3% and up to 30% of cases involving individuals up to the age of 40 respectively (AMA5, p 383). Their presence does not of itself mean that the individual has an impairment due to injury.
4.26 Loss of sexual function should only be assessed where there is other objective evidence of spinal cord, cauda equina or bilateral nerve root dysfunction. The ratings are described in AMA5 Table 15-6 (pp 396–97). There is no additional impairment rating system for loss of sexual function in the absence of objective neurological findings. Loss of sexual function is not assessed as an ADL.
4.27 Radiculopathy is the impairment caused by malfunction of a spinal nerve root or nerve roots. In general, in order to conclude that radiculopathy is present, two or more of the following criteria should be found, one of which must be major (major criteria in bold):
- loss or asymmetry of reflexes
- muscle weakness that is anatomically localised to an appropriate spinal nerve root distribution
- reproducible impairment of sensation that is anatomically localised to an appropriate spinal nerve root distribution
- positive nerve root tension (AMA5 Box 15-1, p 382)
- muscle wasting – atrophy (AMA5 Box 15-1, p 382)
- findings on an imaging study consistent with the clinical signs (AMA5, p 382).
4.28 Radicular complaints of pain or sensory features that follow anatomical pathways but cannot be verified by neurological findings (somatic pain, non-verifiable radicular pain) do not alone constitute radiculopathy.
4.29 Global weakness of a limb related to pain or inhibition or other factors does not constitute weakness due to spinal nerve malfunction.
4.30 Vertebral body fractures and/or dislocations at more than one vertebral level are to be assessed as follows:
- Measure the percentage loss of vertebral height at the most compressed part for each vertebra, then
- Add the percentage loss at each level:
- total loss of more than 50% = DRE IV
- total loss of 25% to 50% = DRE III
- total loss of less than 25% = DRE II
- If radiculopathy is present then the person is assigned one DRE category higher.
One or more end plate fractures in a single spinal region without measurable compression of the vertebral body are assessed as DRE category II.
Posterior element fractures (excludes fractures of transverse processes and spinous processes) at multiple levels are assessed as DRE Ill.
4.31 Displaced fractures of transverse or spinous processes at one or more levels are assessed as DRE category II because the fracture does not disrupt the spinal canal (AMA5, p 385) and do not cause multilevel structural compromise.
4.32 Within a spinal region, separate spinal impairments are not combined. The highest-value impairment within the region is chosen. Impairments in different spinal regions are combined using the combined values chart (AMA5, pp 604-06).
If there are adjacent vertebral fractures at the transition zones (C7/T1, T12/L1), the methodology in paragraph 4.30 in the Guidelines is to be adopted. For fractures of C7 and T1, use the WPI ratings for the cervical spine (AMA5 Chapter 15, Table 15-5, p 392). For fractures of T12 and L1, use the WPI rating for the thoracic spine (AMA5 Chapter 15, Table 15-4, p 389).
4.33 Impact of ADL. Tables 15-3, 15-4 and 15-5 of AMA5 give an impairment range for DREs II to V. Within the range, 0%, 1%, 2% or 3% WPI may be assessed using paragraphs 4.34 and 4.35 below. An assessment of the effect of the injury on ADL is not solely dependent on self-reporting, but is an assessment based on all clinical findings and other reports.
4.34 The following diagram should be used as a guide to determine whether 0%, 1%, 2% or 3% WPI should be added to the bottom of the appropriate impairment range. This is only to be added if there is a difference in activity level as recorded and compared to the worker’s status prior to the injury.
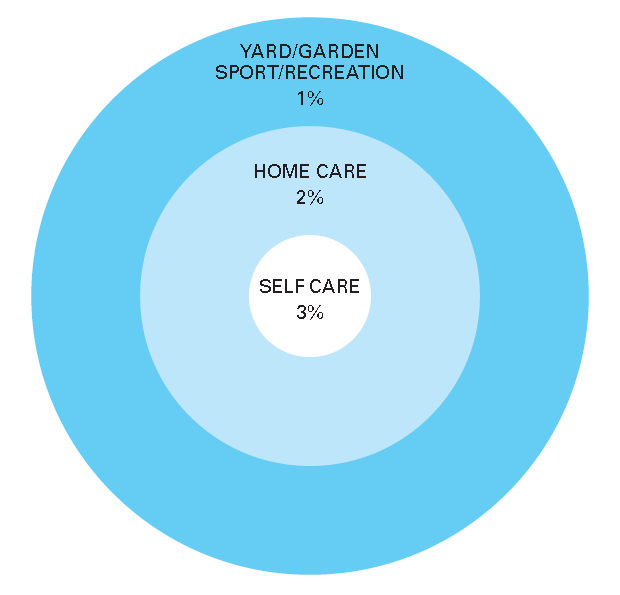
4.35 The diagram is to be interpreted as follows:
Increase base impairment by:
- 3% WPI if the worker’s capacity to undertake personal care activities such as dressing, washing, toileting and shaving has been affected
- 2% WPI if the worker can manage personal care, but is restricted with usual household tasks, such as cooking, vacuuming and making beds, or tasks of equal magnitude, such as shopping, climbing stairs or walking reasonable distances
- 1% WPI for those able to cope with the above, but unable to get back to previous sporting or recreational activities, such as gardening, running and active hobbies etc.
4.36 For a single injury, where there has been more than one spinal region injured, the effect of the injury on ADL is assessed once only.
For injuries to one spinal region on different dates, the effect of the injury on ADL is assessed for the first injury. If, following the second injury, there is a worsening in the ability to perform ADL, the appropriate adjustments are made within the range. For example, if WPI for ADL is assessed as 1% following the first injury and 3% after the second injury, then WPI for ADL for the second injury is assessed as 2%.
For injuries to different spinal regions on different dates, where there is a worsening of ability to perform ADL after the second injury, additional impairment may be assessed. For example, if ADL for a cervical spine injury is assessed as 1%, and an assessment of a subsequent lumbar spine injury determined 3% WPI for ADL, then WPI for impact on ADLs for the lumbar injury is assessed as 2% WPI.
4.37 Effect of surgery: AMA5 tables 15-3 to 15-5 (pp 384, 389 and 392) do not adequately account for the effect of surgery on the impairment rating for certain disorders of the spine. The assessor should note that:
- Surgical decompression for spinal stenosis is DRE category III (AMA5 Table 15-3, 15-4 or 15-5)
- Operations where the radiculopathy has resolved are considered under the DRE category III (AMA5 Table 15-3, 15-4 or 15-5).
- Operations for spinal fusion (successful or unsuccessful) are considered under DRE category IV (AMA5 Table 15-3, 15-4 or 15-5)
- DRE category V is not to be used following spinal fusion where there is a persisting radiculopathy. Instead, use Table 4.2 in the Guidelines
- Radiculopathy persisting after surgery is not accounted for by AMA5 Table 15-3, and incompletely by tables 15-4 and 15-5, which only refer to radiculopathy that has improved following surgery.
Table 4.2 indicates the additional ratings which should be combined with the rating determined using the DRE method where an operation for an intervertebral disc prolapse, spinal canal stenosis or spinal fusion has been performed.
Example 15-4 in AMA5 (p 386) should therefore be ignored.
| Procedures | Cervical | Thoracic | Lumbar |
|---|---|---|---|
| Spinal surgery with residual symptoms and radiculopathy (refer to 4.27 in the Guidelines) | 3% | 2% | 3% |
| Second and further levels | 1% each additional level | 1% each additional level | 1% each additional level |
| Second operation | 2% | 2% | 2% |
| Third and subsequent operations | 1% each | 1% each | 1% each |
In summary, to calculate whole person impairment (WPI) for persisting radiculopathy (as per definition) following surgery:
- Select the appropriate DRE category from Table 15-3, 15-4, or 15-5;
- Determine a WPI value within the allowed range in Table 15-3, 15-4 or 15-5 according to the impact on the worker’s ADL
- Combine this value with the appropriate additional amount from Table 4.2 to determine the final WPI.
4.38 Disc replacement surgery: The impairment resulting from this procedure is to be equated to that from a spinal fusion.
4.39 Arthritis: See paragraphs 3.19 – 3.24, Chapter 3 of the Guidelines.
4.40 Posterior spacing or stabilisation devices: The insertion of such devices does not warrant any additional WPI.
4.41 Spinal cord stimulator or similar device: The insertion of such devices does not warrant any additional WPI.
4.42 Impairment due to pelvic fractures should be evaluated with reference to the following table, which replaces AMA5 Table 15-19.
| Disorder | Whole person impairment |
|---|---|
| 1. Non-displaced, healed fractures | 0 |
| 2. Fractures of the pelvic bones (including sacrum) | |
| i. maximum residual displacement <1cm | 2 |
| ii. maximum residual displacement 1 to 2cm | 5 |
| iii. maximum residual displacement >2cm | 8 |
| iv. bilateral pubic rami fractures, as determined by the most displaced fragment: | |
| a. maximum residual displacement ≥2cm | 5 |
| b. maximum residual displacement >2cm | 8 |
| 3. Traumatic separation of the pubic symphysis | |
| i. <1cm | 5 |
| ii. 1 to 2cm | 8 |
| iii. >2cm | 12 |
| iv. internal fixation/ankylosis | 5 |
| 4. Sacro-lliac joint dislocations or fracture dislocations | |
| i. maximum residual displacement ≥1cm | 8 |
| ii. maximum residual displacement>1cm | 12 |
| iii. internal fixation/ankylosis | 5 |
| 5a. If two out of three joints are internally fixed/ankylosed | 8 |
| 5b. If all three joints are internally fixed/ankylosed | 10 |
| 6. Fractures of the coccyx | |
| i. healed, (and truly) displaced fracture | 1 |
| ii. excision of the coccyx | 5 |
| 7. Fractures of the acetabulum: Evaluate based on restricted range of hip motion |
The rating of WPI is evaluated based on radiological appearance at maximum medical improvement, whether or not surgery has been performed. Multiple injuries of the pelvis should be assessed separately and combined, with the maximum WPI for pelvic fractures being 20%.
AMA5 Chapter 13 (p 305), applies to the assessment of permanent impairment of the nervous system, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
5.1 AMA5 Chapter 13 ‘The central and peripheral nervous system’ (pp 305–56), provides guidelines on methods of assessing permanent impairment involving the central nervous system. It is logically structured and consistent with the usual sequence of examination of the nervous system. Cerebral functions are discussed first, followed by the cranial nerves, station, gait and movement disorders, the upper extremities related to central impairment, the brain stem, the spinal cord and the peripheral nervous system, including neuromuscular junction and muscular system. A summary concludes the chapter.
5.2 Spinal cord injuries are to be assessed using AMA5Chapter 15. Table 15-6 (pp 396–97) is to be used for evaluation of spinal cord injuries. These impairments, once selected, are then combined with the corresponding additional spinal impairment from DRE categories II–V for cervical and lumbar impairment and categories II–IV for thoracic impairment to obtain an exact total value.
5.3 Impairments of the peripheral nervous system are assessed by using the relevant parts of the upper extremity, lower extremity and spine sections of AMA5.
The approach to assessment of permanent neurological impairment
5.4 AMA5 Chapter 13 disallows combination of cerebral impairments. However, for the purpose of the Guidelines, cerebral impairments should be evaluated and combined as follows:
- consciousness and awareness
- mental status, cognition and highest integrative function
- aphasia and communication disorders
- emotional and behavioural impairments.
The assessor should take care to be as specific as possible and not to double-rate the same impairment, particularly in the mental status and behavioural categories.
These impairments are to be combined using the Combined Values Chart (AMA5, pp 604–06). These impairments should then be combined with other neurological impairments indicated in AMA5 Table 13-1 (p 308).
5.5 AMA5 sections 13.5–13.6 (pp 336–40) should be used for cerebral, basal ganglia, cerebellar or brain stem impairments. This section, therefore, covers hemiplegia, monoplegia (arm or leg), and upper or lower limb impairment due to incoordination, or movement disorder due to brain injury.
5.6 If a person has a spinal injury with spinal cord or cauda equina, bilateral nerve root or lumbosacral plexus injury causing bowel, bladder and/or sexual dysfunction, he or she is assessed according to the method described in AMA5Section 15.7 and Table 15-6 (a)–(g) (pp 395–98).
5.7 Complex regional pain syndrome types 1 and 2 are to be assessed using the method in Chapter 17 of the Guidelines.
5.8 AMA5 Chapter 13, on the nervous system, lists many impairments where the range for the associated WPI is 0–9% or 0–14%. Where there is a range of impairment percentages listed, the assessor should nominate an impairment percentage based on the complete clinical circumstances revealed during the consultation, and in relation to all other available information.
Specific interpretation of AMA5
5.9 In assessing disturbances of mental status and integrative functioning; and emotional or behavioural disturbances; disturbances in the level of consciousness and awareness; disturbances of sleep and arousal function; and disorders of communication (AMA5 sections 13.3a, 13.3c, 13.3d, 13.3e and 13.3f; pp 309–311 and 317–327), the assessor should make ratings based on clinical assessment and the results of neuropsychometric testing, where available.
For traumatic brain injury, there should be evidence of a severe impact to the head, or that the injury involved a high-energy impact.
Clinical assessment must include at least one of the following:
- significant medically verified abnormalities in the Glasgow Coma Scale score
- significant medically verified duration of post-traumatic amnesia
- significant intracranial pathology on CT scan or MRI.
Neuropsychological testing should be conducted by a registered clinical neuropsychologist who is a member, or is eligible for membership, of the Australian Psychological Society’s College of Clinical Neuropsychology. Neuropsychological test data is to be considered in the context of the overall clinical history, examination and radiological findings, and not in isolation.
5.10 Assessment of arousal and sleep disorders (AMA5 Section 13.3c, pp 317–319): refers to assessment of primary sleep disorders following neurological injury. The assessor should make ratings of arousal and sleep disorders based on the clinical assessment that would normally have been done for clinically significant disorders of this type (ie sleep studies or similar tests).
5.11 Olfaction and taste: The assessor should use AMA5 Chapter 11, Section 11.4c (p 262) to assess olfaction and taste, for which a maximum of 5% WPI is allowable for total loss of either sense. The effect on activities of daily living should be considered.
5.12 Visual impairment assessment (AMA4 Chapter 8, pp 209–22): An ophthalmologist should assess all impairments of visual acuity, visual fields, extra-ocular movements or diplopia.
5.13 Trigeminal nerve assessment (AMA5, p 331): Sensory impairments of the trigeminal nerve should be assessed with reference to AMA5 Table 13-11 (p 331). The words ‘sensory loss or dysaesthesia’ should be added to the table after the words ‘neuralgic pain’ in each instance. Lesions of the ophthalmic division of the trigeminal nerve with impairment of corneal sensation should be apportioned with extra weighting.
If present, motor loss for the trigeminal nerve should be assessed in terms of its impact on mastication and deglutition (AMA5, p 262).
For bilateral injury to the trigeminal nerves, assess each side separately and combine the assessed WPIs.
5.14 Spinal accessory nerve: AMA5 provides insufficient reference to the spinal accessory nerve (cranial nerve XI). This nerve supplies the trapezius and sternomastoid muscles. For loss of use of the nerve to trapezius, the assessor should refer to AMA5 Chapter 16 on upper limb assessment, and a maximum of 10% impairment of the upper limb may be assigned. For additional loss of use of sternomastoid, a maximum of 3% upper limb impairment may be added.
5.15 Impairment of sexual function caused by severe traumatic brain injury is to be assessed using AMA5 Table 13-21 (p 342). For spinal cord, nerve root or more peripheral nerve injury, sexual impairment should only be assessed where there is appropriate objective evidence of spinal cord, cauda equina or bilateral nerve root dysfunction, or lumbosacral plexopathy.
5.16 Impairment due to miscellaneous peripheral nerves should be evaluated with reference to the following table.
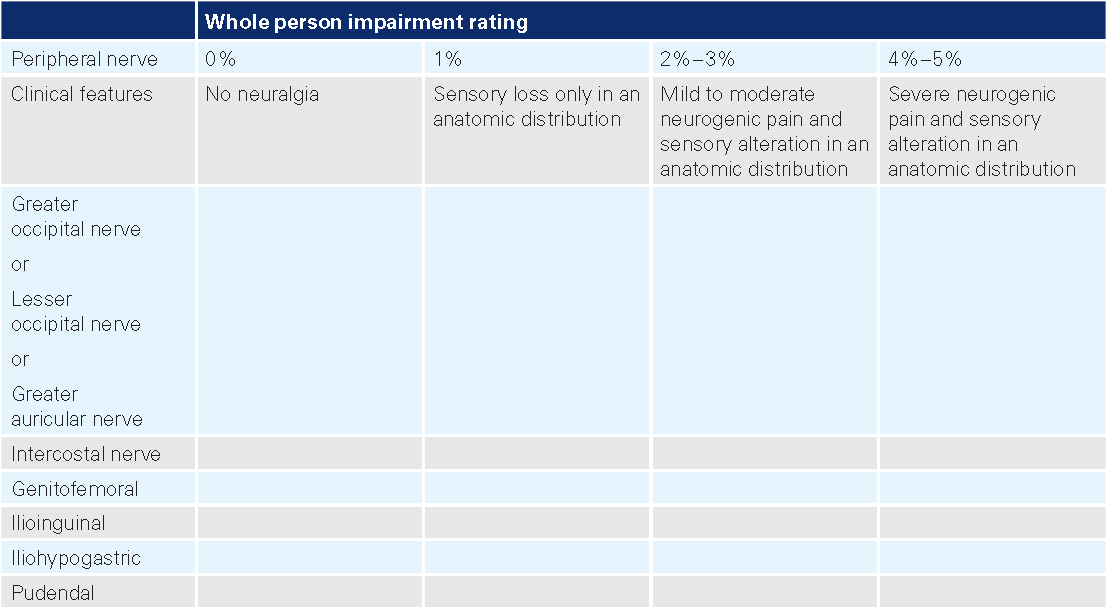
AMA5 Chapter 11 (p 245), applies to the assessment of permanent impairment of the ear (with the exception of hearing impairment), nose, throat and related structures, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing.
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
6.1 AMA5 Chapter 11 (pp 245–75) details the assessment of the ear, nose, throat and related structures. With the exception of hearing impairment, which is dealt with in Chapter 9 of the Guidelines, AMA5 Chapter 11 should be followed in assessing permanent impairment, with the variations included below.
6.2 The level of impairment arising from conditions that are not work-related needs to be assessed by the medical assessor and taken into consideration in determining the level of permanent impairment. The level at which pre-existing conditions and lifestyle activities, such as smoking, contribute to the level of permanent impairment requires judgement on the part of the clinician undertaking the impairment assessment. The manner in which any deduction for these is applied needs to be recorded in the assessing specialist’s report.
The ear
6.3 Equilibrium is assessed according to AMA5 Section 11.2b (pp 252–55), but add these words to AMA5 Table 11-4, class 2 (p 253): ‘without limiting the generality of the above, a positive Hallpikes test is a sign and an objective finding’.
The face (AMA5, pp 255-59)
6.4 AMA5 Table 11-5 (p 256) should be replaced with Table 6.1, below, when assessing permanent impairment due to facial disorders and/or disfigurement.
| Class 1 0-5% impairment of the whole person | Class 2 6-10% impairment of the whole person | Class 3 11-15% impairment of the whole person | Class 4 16-50% impairment of the whole person |
|---|---|---|---|
Facial abnormality limited to disorder of cutaneous structures, such as visible scars (not hypertrophic or atrophic) or abnormal pigmentation (refer toAMA5 Chapter 8 for skin disorders) or mild, unilateral, facial paralysis affecting most branches or nasal distortion that affects physical appearance or partial loss or deformity of the outer ear. | Facial abnormality involves loss of supporting structure of part of the face, with or without cutaneous disorder (eg depressed cheek, nasal, or frontal bones) or near complete loss of definition of the outer ear. | Facial abnormality involves absence of normal anatomic part or area of face, such as loss of eye or loss of part of nose, with resulting cosmetic deformity, combine with any functional loss, eg vision (AMA4 Chapter 8) or severe unilateral facial paralysis affecting most branches or mild, bilateral, facial paralysis affecting most branches. | Massive or total distortion of normal facial anatomy with disfigurement so severe that it precludes social acceptance or severe, bilateral, facial paralysis affecting most branches or loss of a major portion of or entire nose. |
Note: Tables used to classify the examples in AMA5 Section 11.3 (pp 256-59) should also be ignored and assessors should refer to the modified table above for classification.
6.5 In AMA5 example 11-11 (p 257), add the words ‘visual impairment related to enophthalmos must be assessed by an Ophthalmologist’.
The nose, throat and related structures
6.6 In regard to sleep apnoea (third paragraph of AMA5 Section 11.4a, p 259), a sleep study and an examination by an ear, nose and throat specialist is mandatory before assessment by an approved assessor.
6.7 The assessment of sleep apnoea is addressed in AMA5 Section 5.6 (p 105) and assessors should refer to this chapter, as well as paragraphs 8.8 - 8.10 in Chapter 8 of the Guidelines.
6.8 AMA5 Table 11-6, ‘Criteria for rating impairment due to air passage defects’ (p 260), should be replaced with Table 6.2, below, when assessing permanent impairment due to air passage defects.
Table 6.2: Criteria for rating permanent impairment due to air passage defects
| Percentage impairment of the whole person | |
|---|---|
| Class 1a 0-5% | There are symptoms of significant difficulty in breathing through the nose. Examination reveals significant partial obstruction of the right and/ or left nasal cavity or nasopharynx or significant septal perforation. |
| Class 1 0-10% | Dyspnea does not occur at rest and dyspnea is not produced by walking freely on a level surface, climbing stairs freely or performance of other usual activities of daily living and dyspnea is not produced by stress, prolonged exertion, hurrying, hill climbing, or recreational or similar activities requiring intensive effort* and examination reveals partial obstruction of the oropharynx, laryngopharynx, larynx, upper trachea (to the fourth cartilaginous ring), lower trachea, bronchi or complete (bilateral) obstruction of the nose or nasopharynx. |
| Class 2 11-29% | Dyspnea does not occur at rest and dyspnea is not produced by walking freely on a level surface, climbing one flight of stairs or performance of other usual activities of daily living but dyspnea is produced by stress, prolonged exertion, hurrying, hill climbing, or recreational or similar activities (except sedentary forms) and examination reveals partial obstruction of the oropharynx, laryngopharynx, larynx, upper trachea (to the fourth cartilaginous ring), lower trachea, bronchi or complete (bilateral) obstruction of the nose or nasopharynx. |
| Class 3 11-29% | Dyspnea does not occur at rest and dyspnea is produced by walking freely more than one or two level blocks, climbing one flight of stairs, even with periods of rest, or performance of other usual activities of daily living and dyspnea is produced by stress, prolonged exertion, hurrying, hill climbing, or recreational or similar activities and examination reveals partial obstruction of the oropharynx, laryngopharynx, larynx, upper trachea (to the fourth cartilaginous ring), lower trachea or bronchi. |
| Class 4 50-89% | Dyspnea occurs at rest, although individual is not necessarily bedridden and dyspnea is aggravated by the performance of any of the usual activities of daily living (beyond personal cleansing, dressing or grooming) and examination reveals partial obstruction of the oropharynx, laryngopharyx, larynx, upper trachea (to the fourth cartilaginous ring), lower trachea, and/or bronchi. |
| Class 5 90%+ | Severe dyspnea occurs at rest and spontaneous respiration is inadequate and respiratory ventilation is required and examination reveals partial obstruction of the oropharynx, laryngopharynx, larynx, upper trachea (to the fourth cartilaginous ring), lower trachea or bronchi. |
* Prophylactic restriction of activity, such as strenuous competitive sport, does not exclude subject from class 1.
Note: Individuals with successful permanent tracheostomy or stoma should be rated at 25% WPI. AMA5 example 11-16 (p 261), ‘Partial obstruction of the larynx affecting only one vocal cord’, is better linked to voice (AMA5 Section 11.4e).
6.9 When using AMA5 Table 11-7 ‘Relationship of dietary restrictions to permanent impairment’ (p 262), the first WPI category is to be 0–19%, not 5–19%.
6.10 Regarding the first sentence of the ‘Examining procedure’ subsection of AMA5 (pp 263–64): the examiner should have sufficient hearing for the purpose- disregard ‘normal hearing as defined in the earlier section of this chapter on hearing’.
6.11 ‘Examining procedure’ (AMA5, pp 263-64), second paragraph: ‘The examiner should base judgements of impairment on two kinds of evidence: (1) attention to and observation of the individual’s speech in the office – for example, during conversation, during the interview, and while reading and counting aloud – and (2) reports pertaining to the individual’s performance in everyday living situations’. Disregard the next sentence: ‘The reports or the evidence should be supplied by reliable observers who know the person well.’
6.12 ‘Examining procedure’ (AMA5, pp 263-64): where the word ‘American’ appears as a reference, substitute ‘Australian’, and change measurements to the metric system (eg 8.5 inches = 22 centimetres).
6.13 Substitute the word ‘laryngopharyngeal’ for ‘gastroesophageal’ in all examples where it appears.
6.14 Example 11.25 (AMA5, p 269) ‘Impairment rating’, second sentence: add the words “including respiratory impairment” into the sentence to read ‘Combine with appropriate ratings due to other impairments including respiratory impairment to determine whole person impairment’.
6.15 Disregard AMA5 Table 11-10 (pp 272–75), except for impairment of olfaction and/or taste, and hearing impairment as determined in the Guidelines.
AMA5 Chapter 7 (p 143) applies to the assessment of permanent impairment of the urinary and reproductive systems, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
7.1 AMA5 Chapter 7 (pp 143–71) provides clear details for assessment of the urinary and reproductive systems. Overall, the chapter should be followed in assessing permanent impairment, with the variations included below.
7.2 For both male and female sexual dysfunction, identifiable pathology should be present for an impairment percentage to be given.
Urinary diversion
7.3 AMA5 Table 7-2 (p 150) should be replaced with Table 7.1, below, when assessing permanent impairment due to urinary diversion disorders. This table includes ratings for neobladder and continent urinary diversion.
7.4 Continent urinary diversion is defined as a continent urinary reservoir constructed of small or large bowel with a narrow catheterisable cutaneous stoma through which it must be emptied several times a day.
| Diversion type | % Impairment of the whole person |
|---|---|
| Ureterointestinal | 10 |
| Cutaneous ureterostomy | 10 |
| Nephrostomy | 15 |
| Neobladder/replacement cystoplasty | 15 |
| Continent urinary diversion | 20 |
Bladder
7.5 AMA5 Table 7-3 (p 151) should be replaced with Table 7.2, below, when assessing permanent impairment due to bladder disease. This table includes ratings involving urge and total incontinence (defined in 7.8 of the Guidelines).
| Class 1 0-15% impairment of the whole person | Class 2 16-40% impairment of the whole person | Class 3 41-70% impairment of the whole person |
|---|---|---|
Symptoms and signs of bladder disorder and requires intermittent treatment and normal functioning between malfunctioning episodes | Symptoms and signs of bladder disorder eg urinary frequency (urinating more than every two hours), severe nocturia (urinating more than three times a night), urge incontinence more than once a week and requires continuous treatment | Abnormal (ie under or over) reflex activity (eg intermittent urine dribbling, loss of control, urinary urgency and urge incontinence once or more each day) and/or no voluntary control of micturition, reflex or areflexic bladder on urodynamics and/or total incontinence eg fistula. |
7.6 AMA5 example 7-16 (p 151) should be reclassified as an example of class 2, as the urinary frequency is more than every two hours and continuous treatment would be expected.
Urethra
7.7 AMA5 Table 7-4 (p 153) should be replaced with Table 7.3 below when assessing permanent impairment due to urethral disease. This table includes ratings involving stress incontinence.
Urinary incontinence
7.8 Urge urinary incontinence is the involuntary loss of urine associated with a strong desire to void. Stress urinary incontinence is the involuntary loss of urine occurring with clinically demonstrable raised intra-abdominal pressure. It is expected that urinary incontinence of a regular or severe nature (necessitating the use of protective pads or appliances) will be assessed as follows:
| Stress urinary incontinence (demonstrable clinically) | 11-25%, according to severity |
| Urge urinary incontinence | 16-40%, according to severity |
| Mixed (urge and stress) incontinence | 16-40%, according to severity |
| Nocturnal enuresis or wet in bed | 16-40%, according to severity |
| Total incontinence (continuously wet - eg from fistula) | 50-70% |
The highest scoring condition is to be used to assess impairment - combinations are not allowed.
Male reproductive organs
7.9 On page 157 of AMA5, the box labelled ‘class 3, 21–35% impairment of the whole person’ should read ‘class 3, 20% impairment of the whole person’, as the descriptor ‘no sexual function possible’ does not allow a range. (The correct value is shown in AMA5 Table 7-5, p 156). Note, however, that there is a loading for age, so a rate higher than 20% is possible.
7.10 AMA5 Table 7-7 (p 159) should be replaced with Table 7.4, below, when assessing permanent impairment due to testicular, epididymal and spermatic cord disease. This table includes rating for infertility and equates impairment with female infertility (see Table 7.5 in the Guidelines). Infertility in either sex must be considered to be of equal impact, age for age.
7.11 Male infertility is defined as azoospermia or other cause of inability to cause impregnation, even with assisted contraception techniques.
7.12 Loss of sexual function related to spinal injury should only be assessed as an impairment where there is other objective evidence of spinal cord, cauda equina or bilateral nerve root dysfunction. The ratings described in AMA5 Table 13-21 (p 342) are used in this instance. There is no additional impairment rating system for loss of sexual function in the absence of objective clinical findings.
Table 7.4: Criteria for rating permanent impairment due to testicular, epididymal and spermatic cord disease
| Class 1 0-10% impairment of the whole person | Class 2 11-15% impairment of the whole person | Class 3 16-35% impairment of the whole person |
|---|---|---|
Testicular, epididymal or spermatic cord disease symptoms and signs and anatomic alteration and no continuous treatment required and no seminal or hormonal function or abnormalities or solitary testicle | Testicular, epididymal or spermatic cord disease symptoms and signs and anatomic alteration and cannot effectively be controlled by treatment and detectable seminal or hormonal abnormalities | Trauma or disease produces bilateral anatomic loss of the primary sex organs or no detectable seminal or hormonal function or infertility |
Female reproductive organs
7.13 AMA5 Table 7-11 (p 167) should be replaced with Table 7.5, below, when assessing permanent impairment due to fallopian tube and ovarian disease. This table includes rating for infertility and equates impairment with male infertility (see Table 7.4, above). Infertility in either sex must be considered to be of equal impact, age for age.
7.14 Female infertility: A woman in the childbearing age is infertile when she is unable to conceive naturally. This may be due to anovulation, tubal blockage, cervical or vaginal blocking or an impairment of the uterus.
Table 7.5: Criteria for rating permanent impairment due to fallopian tube and ovarian disease
| Class 1 0-15% impairment of the whole person | Class 2 16-25% impairment of the whole person | Class 3 26-35% impairment of the whole person |
|---|---|---|
Fallopian tube or ovarian disease or deformity symptoms and signs do not require continuous treatment or only one functioning fallopian tube or ovary in the premenopausal period or bilateral fallopian tube or ovarian functional loss in the postmenopausal period | Fallopian tube or ovarian disease or deformity symptoms and signs require continuous treatment, but tubal patency persists and ovulation is possible | Fallopian tube or ovarian disease deformity symptoms and signs and total tubal patency loss or failure to produce ova in the premenopausal period or bilateral fallopian tube or bilateral ovarian loss in the premenopausal period; infertility |
AMA5 Chapter 5 (p 87) applies to the assessment of permanent impairment of the respiratory system, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
8.1 AMA5 Chapter 5 provides a useful summary of the methods for assessing permanent impairment arising from respiratory disorders.
8.2 The level of impairment arising from conditions that are not work-related needs to be assessed by the medical assessor and taken into consideration in determining the level of permanent impairment. The level at which pre-existing conditions and lifestyle activities, such as smoking, contribute to the level of permanent impairment requires judgement on the part of the clinician undertaking the impairment assessment. The manner in which any deduction for these is applied needs to be recorded in the assessing specialist’s report.
Examinations, clinical studies and other tests for evaluating respiratory disease (AMA5 Section 5.4)
8.3 AMA5 tables 5-2b, 5-3b, 5-4b, 5-5b, 5-6b and 5-7b (pp 95–100) give the lower limits of normal values for pulmonary function tests. These are used in AMA5 Table 5-12 (p 107) to determine the impairment classification for respiratory disorders.
8.4 Classes 2, 3 and 4 in Table 5-12 list ranges of whole person impairment (WPI). The assessor should nominate the nearest whole percentage based on the complete clinical circumstances when selecting within the range.
Asthma (AMA5 Section 5.5)
8.5 In assessing permanent impairment arising from occupational asthma, the assessor will require evidence from the treating physician that:
- at least three lung function tests have been performed over a six-month period and that the results were consistent and repeatable over that period
- the worker has received maximal treatment and is compliant with his or her medication regimen.
8.6 Bronchial challenge testing should not be performed as part of the impairment assessment. Therefore, in AMA5 Table 5-9 (p 104), ignore column 4 (PC20 mg/mol or equivalent, etc.).
8.7 Permanent impairment due to asthma is rated by the score for the best post-bronchodilator forced expiratory volume in one second (FEV1) (score in column 2, AMA5 Table 5-9) plus per cent of FEV1 (score in column 3) plus minimum medication required (score in column 5). The total score derived is then used to assess the per cent impairment in AMA5 Table 5-10 (p 104).
Obstructive sleep apnoea (AMA Section 5.6)
8.8 This section needs to be read in conjunction with AMA5 sections 11.4 (p 259) and 13.3c (p 317).
8.9 Before permanent impairment can be assessed, the person must have appropriate assessment and treatment by an ear, nose and throat surgeon and a respiratory physician who specialises in sleep disorders.
8.10 The degree of permanent impairment due to sleep apnoea should be calculated with reference to AMA5 Table 13-4 (p 317).
Hypersensitivity pneumonitis (AMA5 Section 5.7)
8.11 Permanent impairment arising from disorders included in this section are assessed according to the impairment classification in AMA5 Table 5-12 (p 107).
Pneumoconiosis (AMA5 Section 5.8)
8.12 This section is excluded from the Guidelines, as these are the subject of the Dust Diseases Legislation.
Lung cancer (AMA5 Section 5.9)
8.13 Permanent impairment due to lung cancer should be assessed at least six months after surgery. AMA5 Table 5-12 (p 107), not Table 5-11, should be used for assessment of permanent impairment.
8.14 Persons with residual lung cancer after treatment are classified in respiratory impairment class 4 (AMA5 Table 5-12).
Permanent impairment due to respiratory disorders (AMA5 Section 5.10)
8.15 AMA5 Table 5-12 should be used to assess permanent impairment for respiratory disorders. The pulmonary function tests listed in Table 5-12 must be performed under standard conditions. Exercise testing is not required on a routine basis.
8.16 An isolated abnormal diffusing capacity for carbon monoxide (DCO) in the presence of otherwise normal results of lung function testing should be interpreted with caution and its aetiology should be clarified.
AMA5 Chapter 11 (p 245) applies to the assessment of permanent impairment of hearing, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- the appropriate chapter(s) of the Guidelines for the body system they are assessing.
- the National Acoustic Laboratories Report No. 118 January 1988 ‘Improved procedure for determining percentage loss of hearing’.
The Guidelines take precedence over AMA5.
Assessment of hearing impairment (hearing loss)
9.1 A worker may present for assessment of hearing loss for compensation purposes before having undergone all or any of the health investigations that generally occur before assessment of permanent impairment. For this reason, and to ensure that conditions other than ‘occupational hearing impairment’ are precluded, the medical assessment should be undertaken by an ear, nose and throat specialist or other appropriately qualified medical specialist. The medical assessment needs to be undertaken in accordance with the hearing impairment section of AMA5 Table 11-10 (pp 272–275). The medical specialist performing the assessment must examine the worker. The medical specialist’s assessment must be based on medical history and ear, nose and throat examination, evaluation of relevant audiological tests, and evaluation of other relevant investigations available to the medical assessor. Only medical specialists can sign medical reports.
9.2 Disregard AMA5 sections 11.1b and 11.2 (pp 246–55), but retain Section 11.1a, ‘Interpretation of symptoms and signs’ (p 246).
9.3 Some of the relevant tests are discussed in the AMA5 hearing impairment evaluation summary in AMA5 Table 11-10 (pp 272–75). The relevant row for the Guidelines is the one headed ‘hearing impairment’, with the exception of the last column, headed ‘degree of impairment’. The degree of impairment is determined according to the Guidelines.
9.4 The level of hearing impairment caused by non-work-related conditions is assessed by the medical specialist and considered when determining the level of work-related hearing impairment. While this requires medical judgement on the part of the examining medical specialist, any non-work-related deductions should be recorded in the report.
9.5 Disregard AMA5 tables 11-1, 11-2 and 11-3 (pp 247–50). For the purposes of the Guidelines, National Acoustic Laboratory (NAL) tables from the NAL Report No. 118, ‘Improved procedure for determining percentage loss of hearing’ (January 1988) are adopted as follows:
- Tables RB 500-4000 (pp 11–16)
- Tables RM 500-4000 (pp 18–23)
- Appendices 1 and 2 (pp 8–9)
- Appendices 5 and 6 (pp 24–26)
- Tables EB 4000–8000 (pp 28–30) (The extension tables)
- Table EM 4000–8000 (pp 32–34) (The extension tables)
Where an assessor uses the extension tables, they must provide an explanation of the worker’s ‘special requirement to be able to hear at frequencies above 4000 Hz’ (NAL Report No.118, p 6).
In the presence of significant conduction hearing loss, the extension tables do not apply.
AMA5 Table 11-3 is to be replaced by Table 9.1 at the end of this chapter.
Hearing impairment
9.6 Impairment of a worker’s hearing is determined according to evaluation of the individual’s binaural hearing impairment (BHI).
9.7 Permanent hearing impairment should be evaluated when the condition is stable. Prosthetic devices (that is, hearing aids) must not be worn during the evaluation of hearing sensitivity.
9.8 Hearing threshold level for pure tones is defined as the number of decibels above standard audiometric zero for a given frequency at which the listener’s threshold of hearing lies when tested in a suitable sound attenuated environment. It is the reading on the hearing level dial of an audiometer that is calibrated according to Australian Standard AS 2586 1983.
9.9 Evaluation of binaural hearing impairment is determined by using the tables in the 1988 NAL publication with allowance for presbyacusis according to the presbyacusis correction table, if applicable, in the same publication.
The binaural tables RB 500-4000 (NAL publication, pp 11–16) are to be used. The extension tables EB 4000- 8000 (NAL publication, pp 28–30) may be used when the worker has a ‘special requirement to be able to hear at frequencies above 4000 Hz’ (NAL publication, p 6). Where an assessor uses the extension tables, they must provide an explanation of the worker’s special requirement to be able to hear at frequencies above 4000 Hz. For the purposes of calculating binaural hearing impairment, the better and worse ear may vary as between frequencies.
Where it is necessary to use the monaural tables, the binaural hearing impairment (BHI) is determined by the
formula:
BHI = [4 x (better ear hearing loss)] + worse ear hearing loss ÷ 5
9.10 Presbyacusis correction (NAL publication, p 24) only applies to occupational hearing loss contracted by a gradual process (eg occupational noise-induced hearing loss and/or occupational solvent-induced hearing loss). Please note that when calculating by formula for presbyacusis correction (eg when the worker is older than 81), use the formula shown in Appendix 6, line 160 of the NAL publication (p 26), which uses the correct number of 1.79059. Note: there is a typographical error in Table P on p 25 of the NAL publication, where the number 1.79509 is incorrectly used.
9.11 Binaural hearing impairment and severe tinnitus: Up to 5 per cent may be added to the work-related binaural hearing impairment for severe tinnitus caused by a work-related injury:
- after presbyacusis correction, if applicable
- before determining whole person impairment (WPI).
Assessment of severe tinnitus is based on a medical specialist’s assessment.
9.12 Only hearing ear: A worker has an ‘only hearing ear’ if he or she has suffered a non-work related severe or profound sensorineural hearing loss in the other ear. If a worker suffers a work-related injury causing a hearing loss in the only hearing ear of x dB HL at a relevant frequency, the worker’s work-related binaural hearing impairment at that frequency is calculated from the binaural tables using x dB as the hearing threshold level in both ears. Deduction for presbyacusis, if applicable, and addition for severe tinnitus, is undertaken according to the Guidelines.
9.13 When necessary, binaural hearing impairment figures should be rounded to the nearest 0.1%. Rounding up should occur if equal to or greater than 0.05%, and rounding down should occur if equal to or less than 0.04%.
9.14 Table 9.1 in the Guidelines (below) is used to convert binaural hearing impairment, after deduction for presbyacusis if applicable and after addition for severe tinnitus, to WPI.
- The current level of binaural hearing impairment is established by the relevant specialist.
- Convert this to WPI using Table 9.1 in the Guidelines.
- Calculate the proportion of the current binaural hearing impairment that was accounted for by the earlier assessment and express it as a percentage of the current hearing impairment.
- The percentage of current hearing impairment that remains is the amount to be compensated.
- This needs to be expressed in terms of WPI for calculation of compensation entitlement.
Example:
- The current binaural hearing impairment is 8%.
- The WPI is 4%.
- The binaural hearing impairment for which compensation was paid previously is 6%, which is 75% of the current binaural hearing impairment of 8%.
- The remaining percentage, 25% is the percentage of WPI to be compensated.
- Twenty-five per cent of the WPI of 4% is 1% WPI.
| % Binaural hearing impairment | % Whole person impairment | % Binaural hearing impairment | % Whole person impairment |
|---|---|---|---|
| 0.0 - 5.9 | 0 | 51.1 - 53.0 | 26 |
| 6.0 - 6.7 | 3 | 53.1 - 55.0 | 27 |
| 6.8 - 8.7 | 4 | 55.1 - 57.0 | 28 |
| 8.8 - 10.6 | 5 | 57.1 - 59.0 | 29 |
| 10.7 - 12.5 | 6 | 59.1 - 61.0 | 30 |
| 12.6 - 14.4 | 7 | 61.1 - 63.0 | 31 |
| 14.5 - 16.3 | 8 | 63.1 - 65.0 | 32 |
| 16.4 - 18.3 | 9 | 65.1 - 67.0 | 33 |
| 18.4 - 20.4 | 10 | 67.1 - 69.0 | 34 |
| 20.5 - 22.7 | 11 | 69.1 - 71.0 | 35 |
| 22.8 - 25.0 | 12 | 71.1 - 73.0 | 36 |
| 25.1 - 27.0 | 13 | 73.1 - 75.0 | 37 |
| 27.1 - 29.0 | 14 | 75.1 - 77.0 | 38 |
| 29.1 - 31.0 | 15 | 77.1 - 79.0 | 39 |
| 31.1 - 33.0 | 16 | 79.1 - 81.0 | 40 |
| 33.1 - 35.0 | 17 | 81.1 - 83.0 | 41 |
| 35.1 - 37.0 | 18 | 83.1 - 85.0 | 42 |
| 37.1 - 39.0 | 19 | 85.1 - 87.0 | 43 |
| 39.1 - 41.0 | 20 | 87.1 - 89.0 | 44 |
| 41.1 - 43.0 | 21 | 89.1 - 91.0 | 45 |
| 43.1 - 45.0 | 22 | 91.1 - 93.0 | 46 |
| 45.1 - 47.0 | 23 | 93.1 - 95.0 | 47 |
| 47.1 - 49.0 | 24 | 95.1 - 97.0 | 48 |
| 49.1 - 51.0 | 25 | 97.1 - 99.0 | 49 |
| 99.1 - 100 | 50 |
9.16 AMA5 examples 11.1, 11.2 and 11.3 (pp 250–51) are replaced by examples 9.1–9.7, below, which were developed by the working party.
| Element | Example no. |
|---|---|
| General use of binaural table - NAL 1988 | 1, 2 |
| 'Better ear' - 'worse ear' crossover | 1, 2 |
| Assessable audiometric frequencies | 7 - also 1, 2, 4, 5, 6 |
| Tinnitus | 1, 2, 3, 4 |
| Presbycusis | All examples |
| Binaural hearing impairment | All examples |
| Conversion to WPI | All examples |
| Gradual process injury | 3 |
| Noise-induced hearing loss | 1, 2, 3, 5, 6, 7 |
| Solvent-induced hearing loss | 3 |
| Acute occupational hearing loss | 4, 5 |
| Acute acoustic trauma | 5 |
| Pre-existing non-occupational hearing loss | 6 |
| Only hearing ear | 6 |
| NAL 1988 extension table use | 7 |
| Multiple causes of hearing loss | 3, 5, 6 |
| Head injury | 4 |
AMA4 Chapter 8 (p 209) applies to the assessment of permanent impairment of the visual system, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA4 for the body system they are assessing.
The Guidelines take precedence over AMA4 and AMA5.
Introduction and approach to assessment
10.1 The visual system must be assessed by an ophthalmologist.
10.2 AMA4 Chapter 8 (pp 209–22) is adopted for the Guidelines, without significant change.
10.3 AMA4 is used rather than AMA5 for the assessment of permanent impairment of the visual system because:
- the equipment recommended for use in AMA5 is expensive and not owned by most privately practising ophthalmologists (eg the Goldman apparatus for measuring visual fields)
- the assessments recommended in AMA5 are considered too complex, raising a risk that resulting assessments may be of a lower standard than if the AMA4 method is used
- there is little emphasis on diplopia in AMA5, yet this is a relatively frequent problem
- many ophthalmologists are familiar with the Royal Australian College of Ophthalmologists’ impairment guide, which is similar to AMA4.
10.4 Impairment of vision should be measured with the injured worker wearing their prescribed corrective spectacles and/or contact lenses, if that was normal for the injured worker before the workplace injury. If, as a result of the workplace injury, the injured worker has been prescribed corrective spectacles and/or contact lenses for the first time, or different spectacles and/or contact lenses than those prescribed before injury, the difference should be accounted for in the assessment of permanent impairment.
10.5 The ophthalmologist should perform, or review, all tests necessary for the assessment of permanent impairment rather than relying on tests, or interpretations of tests, done by the orthoptist or optometrist.
10.6 An ophthalmologist should assess visual field impairment in all cases.
10.7 In AMA4 Section 8.5 ‘Other conditions’ (p 222), the reference to ‘additional 10% impairment’ means 10% WPI, not 10% impairment of the visual system.
AMA5 Chapter 14 is excluded and replaced by this chapter. Before undertaking an impairment assessment, users of the Guidelines must be familiar with (in this order):
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing.
The Guidelines replace the psychiatric and psychological chapter in AMA5.
Introduction
11.1 This chapter lays out the method for assessing psychiatric impairment. The evaluation of impairment requires a medical examination.
11.2 Evaluation of psychiatric impairment is conducted by a psychiatrist who has undergone appropriate training in this assessment method.
11.3 Permanent impairment assessments for psychiatric and psychological disorders are only required where the primary injury is a psychological one. The psychiatrist needs to confirm that the psychiatric diagnosis is the injured worker’s primary diagnosis.
Diagnosis
11.4 The impairment rating must be based upon a psychiatric diagnosis (according to a recognised diagnostic system) and the report must specify the diagnostic criteria upon which the diagnosis is based. Impairment arising from any of the somatoform disorders (DSM IV TR, pp 485–511) are excluded from this chapter.
11.5 If pain is present as the result of an organic impairment, it should be assessed as part of the organic condition under the relevant table. This does not constitute part of the assessment of impairment relating to the psychiatric condition. The impairment ratings in the body organ system chapters in AMA5 make allowance for any accompanying pain.
11.6 It is expected that the psychiatrist will provide a rationale for the rating based on the injured worker’s psychiatric symptoms. The diagnosis is among the factors to be considered in assessing the severity and possible duration of the impairment, but is not the sole criterion to be used. Clinical assessment of the person may include information from the injured worker’s own description of his or her functioning and limitations, and from family members and others who may have knowledge of the person. Medical reports, feedback from treating professionals and the results of standardised tests – including appropriate psychometric testing performed by a qualified clinical psychologist and work evaluations – may provide useful information to assist with the assessment. Evaluation of impairment will need to take into account variations in the level of functioning over time. Percentage impairment refers to whole person impairment (WPI).
Permanent impairment
11.7 A psychiatric disorder is permanent if, in your clinical opinion, it is likely to continue indefinitely. Regard should be given to:
- the duration of impairment
- the likelihood of improvement in the injured worker’s condition
- whether the injured worker has undertaken reasonable rehabilitative treatment
- any other relevant matters.
Effects of treatment
11.8 Consider the effects of medication, treatment and rehabilitation to date. Is the condition stable? Is treatment likely to change? Are symptoms likely to improve? If the injured worker declines treatment, this should not affect the estimate of permanent impairment. The psychiatrist may make a comment in the report about the likely effect of treatment or the reasons for refusal of treatment.
Co-morbidity
11.9 Consider comorbid features (eg bi-polar disorder, personality disorder, substance abuse) and determine whether they are directly linked to the work-related injury, or whether they were pre-existing or unrelated conditions.
Pre-existing impairment
11.10 To measure the impairment caused by a work-related injury or incident, the psychiatrist must measure the proportion of WPI due to a pre-existing condition. Pre-existing impairment is calculated using the same method for calculating current impairment level. The assessing psychiatrist uses all available information to rate the injured worker’s pre-injury level of functioning in each of the areas of function. The percentage impairment is calculated using the aggregate score and median class score using the conversion table below. The injured worker’s current level of WPI% is then assessed, and the pre-existing WPI% is subtracted from their current level, to obtain the percentage of permanent impairment directly attributable to the work-related injury. If the percentage of pre-existing impairment cannot be assessed, the deduction is 1/10th of the assessed WPI.
Psychiatric impairment rating scale (PIRS)
11.11 Behavioural consequences of psychiatric disorder are assessed on six scales, each of which evaluates an area of functional impairment:
- Self care and personal hygiene (Table 11.1) - Activities of daily living
- Social and recreational activities (Table 11.2) - Activities of daily living
- Travel (Table 11.3) - Activities of daily living
- Social functioning (relationships) (Table 11.4)
- Concentration, persistence and pace (Table 11.5)
- Employability (Table 11.6).
11.12 Impairment in each area is rated using class descriptors. Classes range from 1 to 5, in accordance with severity. The standard form must be used when scoring the PIRS. The examples of activities are examples only. The assessing psychiatrist should take account of the person’s cultural background. Consider activities that are usual for the person’s age, sex and cultural norms.
| Class 1 | No deficit, or minor deficit attributable to the normal variation in the general population. |
|---|---|
| Class 2 | Mild impairment: Able to live independently; looks after self adequately, although may look unkempt occasionally; sometimes misses a meal or relies on take-away food. |
| Class 3 | Moderate impairment: Can't live independently without regular support. Needs prompting to shower daily and wear clean clothes. Does not prepare own meals, frequently misses meals. Family member or community nurse visits (or should visit) 2-3 times per week to ensure minimum level of hygiene and nutrition. |
| Class 4 | Severe impairment: Needs supervised residential care. If unsupervised, may accidentally or purposefully hurt self. |
| Class 5 | Totally impaired: Needs assistance with basic functions, such as feeding and toileting. |
| Class 1 | No deficit, or minor deficit attributable to the normal variation in the general population: regularly participates in social activities that are age, sex and culturally appropriate. May belong to clubs or associations and is actively involved with these. |
|---|---|
| Class 2 | Mild impairment: Occasionally goes to such events eg without needing a support person, but does not become actively involved (eg dancing, cheering favourite team). |
| Class 3 | Moderate impairment: Rarely goes out to such events, and mostly when prompted by family or close friend. Will not go out without a support person. Not actively involved, remains quiet and withdrawn. |
| Class 4 | Severe impairment: Never leaves place of residence. Tolerates the company of family member or close friend, but will go to a different room or garden when others come to visit family or flat mate. |
| Class 5 | Totally impaired: Cannot tolerate living with anybody, extremely uncomfortable when visited by close family member. |
| Class 1 | No deficit, or minor deficit attributable to the normal variation in the general population: Can travel to new environments without supervision. |
|---|---|
| Class 2 | Mild impairment: Can travel without support person, but only in a familiar area such as local shops, visiting a neighbour. |
| Class 3 | Moderate impairment: Cannot travel away from own residence without support person. Problems may e due to excessive anxiety or cognitive impairment. |
| Class 4 | Severe impairment: Finds it extremely uncomfortable to leave own residence even with trusted person. |
| Class 5 | Totally impaired: May require two or more persons to supervise when travelling. |
| Class 1 | No deficit, or minor deficit attributable to the normal variation in the general population: No difficulty in forming and sustaining relationships (eg a partner, close friendships lasting years). |
|---|---|
| Class 2 | Mild impairment: Existing relationships strained. Tension and arguments with partner or close family member, loss of some friendships. |
| Class 3 | Moderate impairment: Previously established relationships severely strained, evidenced by periods of separation or domestic violence. Spouse, relatives or community services looking after children. |
| Class 4 | Severe impairment: Unable to form or sustain long term relationships. Pre-existing relationships ended (eg lost partner, close friends). Unable to care for dependants (eg own children, elderly parent). |
| Class 5 | Totally impaired: Unable to function within society. Living away from populated areas, actively avoiding social contact. |
| Class 1 | No deficit, or minor deficit attributable to the normal variation in the general population. Able to pass a TAFE or university course within normal time frame. |
|---|---|
| Class 2 | Mild impairment: Can undertake a basic retraining course, or a standard course at a slower pace. Can focus on intellectually demanding tasks for periods of up to 30 minutes, then feels fatigued or develops headache. |
| Class 3 | Moderate impairment: Unable to read more than newspaper articles. Finds it difficult to follow complex instructions (eg operating manuals, building plans), make significant repairs to motor vehicle, type long documents, follow a pattern for making clothes, tapestry or knitting. |
| Class 4 | Severe impairment: Can only read a few lines before losing concentration. Difficulties following simple instructions. Concentration deficits obvious even during brief concentration. Unable to live alone, or needs regular assistance from relatives or community services. |
| Class 5 | Totally impaired: Needs constant supervision and assistance within institutional setting. |
| Class 1 | No deficit, or minor deficit attributable to the normal variation in the general population. Able to work full time. Duties and performance are consistent with the injured worker's education and training. The person is able to cope with the normal demands of the job. |
|---|---|
| Class 2 | Mild impairment: Able to work full time but in a different environment from that of the pre-injury job. The duties require comparable skill and intellect as those of the pre-injury job. Can work in the same position, but no more than 20 hours per week (eg no longer happy to work with specific persons, or work in a specific location due to travel required). |
| Class 3 | Moderate impairment: Cannot work at all in same position. Can perform less than 20 hours per week in a different position, which requires less skill or is qualitatively different (eg less stressful). |
| Class 4 | Severe impairment: Cannot work more than one or two days at a time, less than 20 hours per fortnight. Pace is reduced, attendance is erratic. |
| Class 5 | Totally impaired: Cannot work at all. |
Using the PIRS to measure impairment
11.13 Rating psychiatric impairment using the PIRS is a two-step procedure:
- Determine the median class score.
- Calculate the aggregate score.
Determining the median class score
11.14 Each area of function described in the PIRS is given an impairment rating which ranges from Class 1 to 5. The six scores are arranged in ascending order, using the standard form. The median is then calculated by averaging the two middle scores eg:
- Example A: 1, 2, 3, 3, 4, 5 Median Class = 3
- Example B: 1, 2, 2, 3, 3, 4 Median Class = 2.5 = 3*
- Example C: 1, 2, 3, 5, 5, 5 Median Class = 4
*If a score falls between two classes, it is rounded up to the next class. A median class score of 2.5 thus becomes 3.
11.15 The median class score method was chosen as it is not influenced by extremes. Each area of function is assessed separately. While impairment in one area is neither equivalent nor interchangeable with impairment in other areas, the median seems the fairest way to translate different impairments onto a linear scale.
Median class score and percentage impairment
11.16 Each median class score represents a range of impairment, as shown below:
- Class 1 = 0–3%
- Class 2 = 4–10%
- Class 3 = 11–30%
- Class 4 = 31–60%
- Class 5 = 61–100%
Calculation of the aggregate score
11.17 The aggregate score is used to determine an exact percentage of impairment within a particular median class range. The six class scores are added to give the aggregate score. Use of the conversion table to arrive at percentage impairment
11.18 The aggregate score is converted to a percentage score using the conversion Table 11.7, below.
11.19 The conversion table was developed to calculate the percentage impairment based on the aggregate and median scores.
11.20 The scores within the conversion table are spread in such a way to ensure that the final percentage rating is consistent with the measurement of permanent impairment percentages for other body systems.
Table 11.7 Conversion table
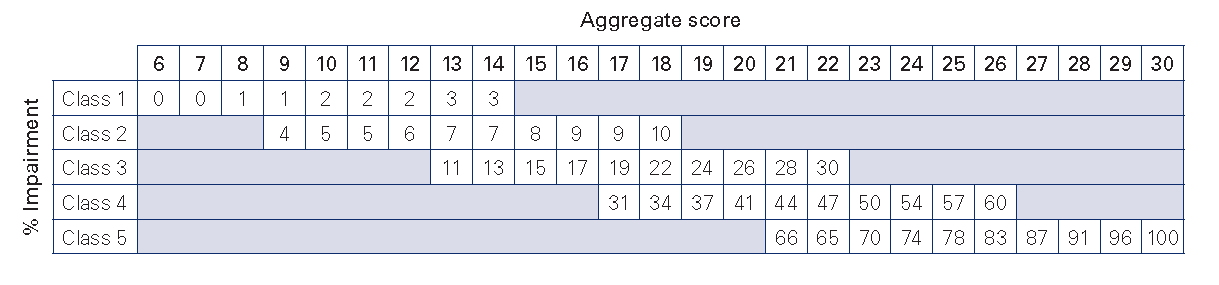
Conversion table — explanatory notes
- The lowest aggregate score that can be obtained is: 1+1+1+1+1+1=6.
- The highest aggregate score is 5+5+5+5+5+5= 30.
- The table therefore has aggregate scores ranging from six to 30.
- Each median class score has an impairment range, and a range of possible aggregate scores (eg class 3 = 11-30 per cent).
- The lowest aggregate score for class 3 is 13 (1 + 1 + 2 + 3 + 3 + 3 = 13).
- The highest aggregate score for class 3 is 22 (3 + 3 + 3 + 3 + 5 + 5 = 22).
- The conversion table distributes the impairment percentages across aggregate scores.
- The conversion table shows that the same aggregate score leads to different percentages of impairment in different median classes.
- For example, an aggregate score of 18 is equivalent to an impairment rating of
- 10% in Class 2,
- 22% in Class 3,
- 34% in Class 4.
- This is due to the fact that an injured worker whose impairment is in median class 2 is likely to have a lower score across most areas of function. They may be significantly impaired in one aspect of their life, such as travel, yet have low impairment in social function, self-care or concentration.
- Someone whose impairment reaches median class 4 will experience significant impairment across most aspects of his or her life.
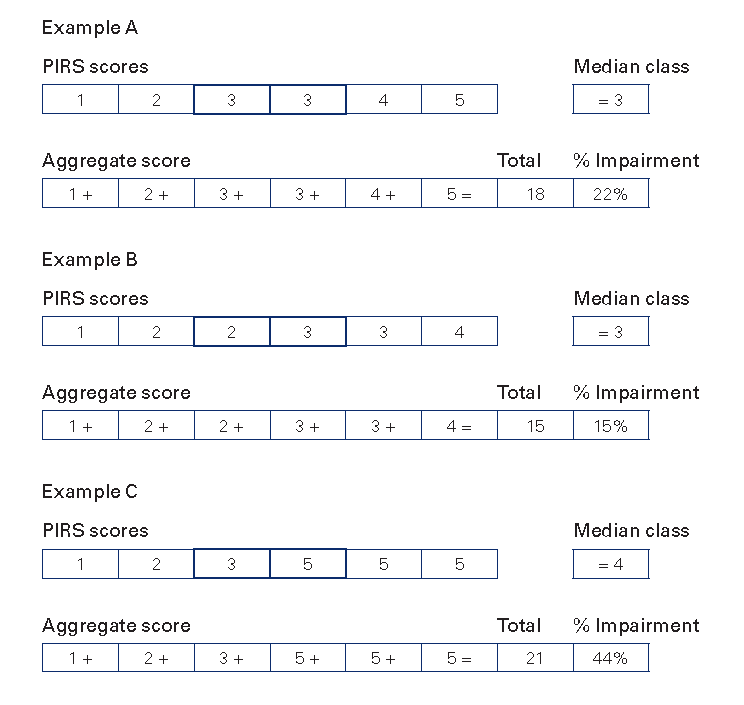
Table 11.8: PIRS rating form
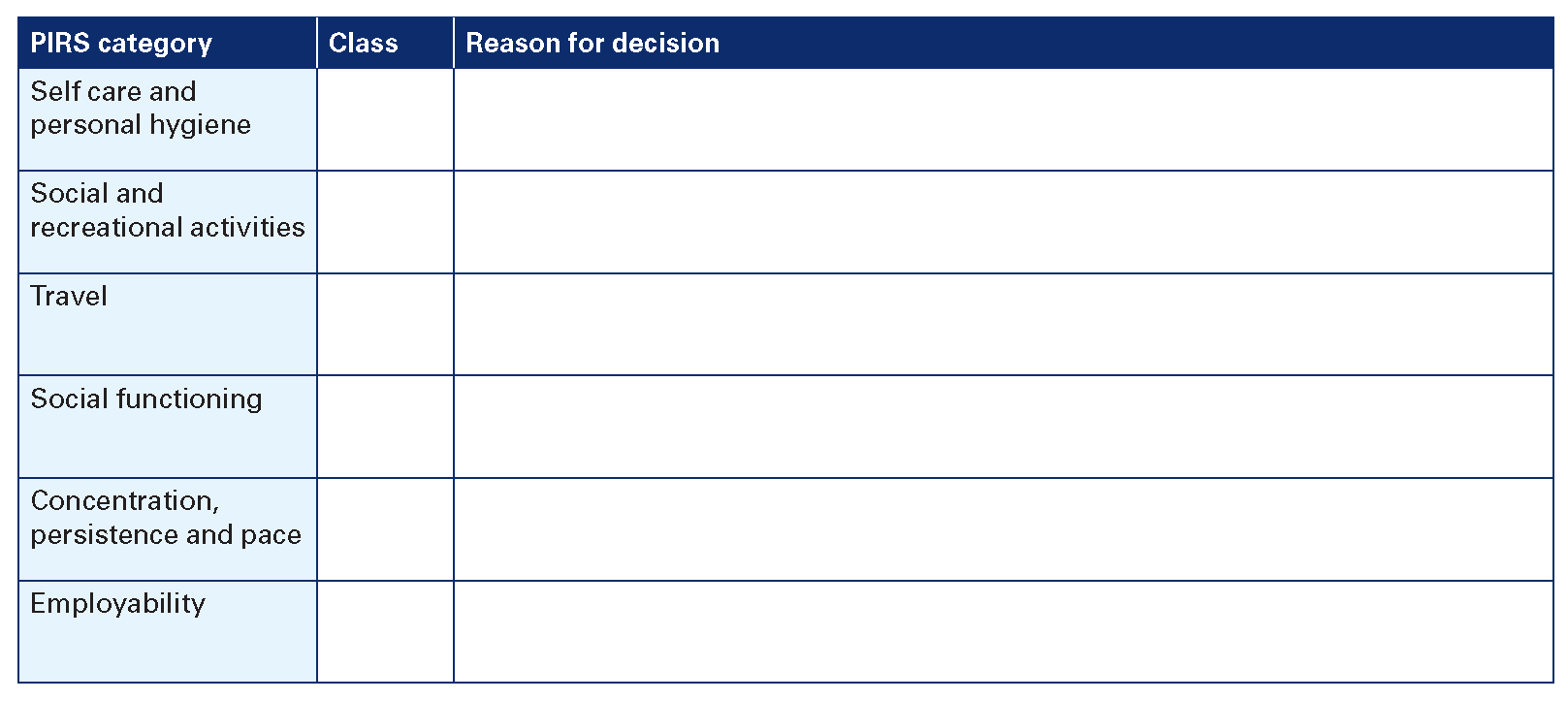
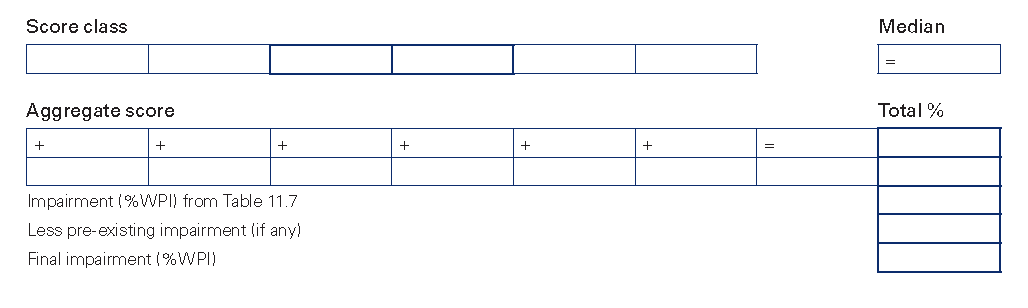
AMA5 Chapter 9 (p 191) applies to the assessment of permanent impairment of the haematopoietic system, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
12.1 AMA5 Chapter 9 (pp 191–210) provides guidelines on the method of assessing permanent impairment of the haematopoietic system. Overall, that chapter should be followed when conducting the assessment, with variations indicated below.
12.2 Impairment of end organ function due to haematopoietic disorder should be assessed separately, using the relevant chapter of the Guidelines. The percentage whole person impairment (WPI) due to end organ impairment should be combined with any percentage WPI due to haematopoietic disorder, using the combined values table in AMA5 (pp 604–06).
Anaemia
12.3 Table 12.1 (below) replaces AMA5 Table 9-2 (p 193).
| Class 1: 0-10% WPI | Class 2: 11-30% WPI | Class 3: 31-70% WPI | Class 4: 71-100% WPI |
|---|---|---|---|
No symptoms and haemoglobin 100-120g/L and no transfusion required | Minimal symptoms and haemoglobin 80-100g/L and no transfusion required | Moderate to marked symptoms and haemoglobin 50-80g/L before transfusion and transfusion of 2 to 3 units required, every 4 to 6 weeks | Moderate to marked symptoms and haemoglobin 50-80g/L before transfusion and transfusion of 2 to 3 units required, every 2 weeks |
12.4 The assessor should exercise clinical judgement in determining WPI, using the criteria in Table 12.1. For example, if comorbidities exist which preclude transfusion, the assessor may assign class 3 or class 4, on the understanding that transfusion would under other circumstances be indicated. Similarly, there may be some claimants with class 2 impairment who, because of comorbidity, may undergo transfusion.
12.5 Pre-transfusion haemoglobin levels in Table 12.1 are to be used as indications only. It is acknowledged that for some claimants, it would not be medically advisable to permit the claimant’s haemoglobin levels to be as low as indicated in the criteria of Table 12.1.
12.6 The assessor should indicate a percentage WPI, as well as the class.
Polycythaemia and myelofibrosis
12.7 The level of symptoms (as in Table 12.1) should be used as a guide for the assessor in cases where non-anaemic tissue iron deficiency results from venesection.
White blood cell diseases
12.8 In cases of functional asplenia, the assessor should assign 3% WPI. This should be combined with any other impairment rating, using the Combined Values Table in AMA5 (pp 604–06).
Haemorrhagic and platelet disorders
12.9 AMA5 Table 9-4 (p 203) is to be used as the basis for assessing haemorrhagic and platelet disorders.
12.10 For the purposes of the Guidelines, the criteria for inclusion in class 3 of AMA5 Table 9-4 (p 203) are:
- symptoms and signs of haemorrhagic and platelet abnormality
- requires continuous treatment
- interference with daily activities; requires occasional assistance.
12.11 For the purposes of the Guidelines, the criteria for inclusion in class 4 of AMA5 Table 9-4 (p 203) is:
- symptoms and signs of haemorrhagic and platelet abnormality
- requires continuous treatment
- difficulty performing daily activities; requires continuous care.
Thrombotic disorders
12.12 AMA5 Table 9-4 (p 203) is used as the basis for determining impairment due to thrombotic disorder.
AMA5 Chapter 10 (p 211) applies to the assessment of permanent impairment of the endocrine system, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
13.1 AMA5 Chapter 10 provides a useful summary of the methods for assessing permanent impairment arising from disorders of the endocrine system.
13.2 Refer to other chapters in AMA5 for related structural changes – the skin (eg pigmentation, in Chapter 8), the central and peripheral nervous system (eg memory, in Chapter 13), the urinary and reproductive system (eg infertility renal impairment, in Chapter 7), the digestive system (eg dyspepsia, in Chapter 6) and the cardiovascular system (in chapters 3 and 4) and visual system (Chapter 8 AMA4).
13.3 The clinical findings to support the impairment assessment are to be reported in the units recommended by the Royal College of Pathologists of Australia. (See Appendix 13.1).
13.4 Westergren erythrocyte sedimentation rate (WSR) is equivalent to ESR.
Adrenal cortex
13.5 AMA5 (p 222) first paragraph: disregard the last sentence, ‘They also affect inflammatory response, cell membrane permeability, and immunologic responses, and they play a role in the development and maintenance of secondary sexual characteristics’. Replace with: ‘Immunological and inflammatory responses are reduced by these hormones and they play a role in the development and maintenance of secondary sexual characteristics.’
13.6 AMA5 example 10-18 (pp 224–25): See reference to ESR (paragraph 13.4, above).
13.7 AMA5 example 10-20, regarding history (p 225): Instead of ‘hypnotic bladder’, read ‘hypotonic bladder’.
Diabetes mellitus
13.8 AMA5 (p 231): refer to the Australian Diabetes Association Guidelines with regard to levels of fasting glucose. (The position statement from the Australian Diabetes Society is reprinted in Appendix 13.2).
13.9 AMA5 (p 231): At the end of the second paragraph insert, ‘The goal of treatment is to maintain haemoglobin A1c within 1% of the normal range (4.0–6.3%)’.
Mammary glands
13.10 AMA5 example 10-45, regarding current symptoms (p 239): Disregard the last sentence, ‘Both bromocriptine and cabergoline cause nausea, precluding use of either drug’. Replace with: ‘Routine use of bromocriptine and cabergoline is normal in Australia. It is rare that nausea precludes their use’.
Criteria for rating permanent impairment due to metabolic bone disease
13.11 AMA5 (p 240): Impairment due to a metabolic bone disease itself is unlikely to be associated with a work injury and would usually represent a pre-existing condition.
13.12 Impairment from fracture, spinal collapse or other complications may arise as a result of a work injury associated with these underlying conditions (as noted in AMA5 Section 10.10c) and would be assessed using the other chapters indicated, with the exception of Chapter 18, on pain, which is excluded from the Guidelines.
Appendix 13.1: Interpretation of pathology tests
From the Manual of use and interpretation of pathology tests, 3rd edition. Reprinted with kind permission of the Royal College of Pathologists of Australasia.
| Alanine aminotransferase (ALT) | (adult) | <35 U/L |
| Albumin | (adult) | 32-45 g/L |
| Alkaline phosphatase (ALP) | (adult, non-pregnant) | 25-100 U/L |
| Alpha fetoprotein | (adult, non-pregnant) | <10 g/L |
| Alpha-1-antitrypsin | 1.7-3.4 g/L | |
| Anion gap | 8-16 mmol/L | |
| Aspartate aminotransferase (AST) | <40 U/L | |
| Bicarbonate (total CO2) | 22-32 mmol/L | |
| Bilirubin (total) | (adult) | <20 μmol/L |
| Calcium | (total) | 2.10-2.60 mmol/L |
| (ionised) | 1.17-1.30 mmol/L | |
| Chloride | 95-110 mmol/L | |
| Cholesterol (HDL) | (male) | 0.9-2.0 mmol/L |
| (female) | 1.0-2.2 mmol?L | |
| Cholesterol (total) (National Heart Foundation (Australia) recommendation) | <5.5 mmol/L | |
| Copper | 13-22 μmol/L | |
| Creatine kinase (CK) | (male) | 60-220 U/L |
| (female) | 30-180 U/L | |
| Creatinine | (adult male) | 0.06-0.12 mmol/L |
| (adult female) | 0.05-0.11 mmol/L | |
| Gamma glutamyl transferase (GGT) | (male) | <50 U/L |
| (female) | <30 U/L | |
| Globulin | adult | 25-35 g/L |
| Glucose | (venous plasma) - (fasting) (venous plasma) - (random) | 3.0-5.4 mmol/L 3.0-7.7 mmol/L |
| Lactate dehydrogenase (LD) | (adult) | 110-230 U/L |
| Magnesium | (adult) | 0.8-1.5 mmol/L |
| Osmolality | (adult) | 280-300 m.osmoll/kg water |
| pCO2 | (arterial blood) | 4.6-6.0 kPa (35-45 mmHg) |
| pH | (arterial blood) | 7.36-7.44 (36-44 nmol/L) |
| Phosphate | 0.8-1.5 mmol/L | |
| pO2 | (arterial blood) | 11.0-13.5 kPa (80-100 mmhg) |
| Potassium | (plasma) | 3.4-4.5 mmol/L |
| (serum) | 3.8-4.9 mmol/L | |
| Prolactin | (male) | 150-500 m U/L |
| (female) | 0-750 m U/L | |
| Protein, total | (adult) | 62-80 g/L |
| Sodium | 135-145 mmol/L | |
| Testosterone and related androgens | See Table A below | |
| Male | Female | |||
|---|---|---|---|---|
| Pre-pubertal | Adult (age related) | Pre-pubertal | Adult (age related) | |
| Free testosterone (pmol/L) | 170-510 | <4.0 | ||
| Total testosterone (nmol/L) | <0.5 | 8-35 | <0.5 | <4.0 |
| SHBG (nmol/L) | 55-100 | 10-50 | 55-100 | 30-90 (250-500 in the third trimester) |
| Dihydrotestosterone (nmol/L) | 1-2.5 | |||
| Haemoglobin (Hb) | (adult male) (adult female) | 130-180 g/L 115-165 g/L |
| Red cell count (RCC) | (adult male) (adult female) | 4.5-6.5 x 1012/L 3.8-5.8 x 1012/L |
| Packed cell volume (PCV) | (adult male) (adult female) | 0.40-0.54 0.37-0.47 |
| Mean cell volume (MCV) | 80-100 fL | |
| Mean cell haemoglobin (MCH) | 27-32 pg | |
| Mean cell haemoglobin concentration (McHC) | 300-350 g/L | |
| Leucocyte (white cell) count (WCC) | 4.0-11.0 x 109/L | |
Leucocyte differential count
Platelet count | 2.0-7.5 x 109/L 0.04-0.4 x 109/L <0.1 x 109/L 0.2-0.8 x 109/L 1.5-4.0 x 109/L 150-400 x 109/L | |
| Erythrocyte sedimentation rate (ESR) | male 17-50 yrs male >50 yrs female 17-50 yrs female >50 yrs | 1-10 mm/hour 2-14 mm/hour 3-12 mm/hour 5-20 mm/hour |
| Reticulocyte count | 10-100 x 109/L (0.2-2.0%) |
| Iron | (adult) | 10-30 μmol/L |
| Iron (total) binding capacity (TIBC) | 45-80 μmol/L | |
| Transferrin | 1.7-3.0 g/L | |
| Transferrin saturation | 0.15-0.45 (15-45%) | |
| Ferritin | (male) (female) | 30-300 μg/L 15-200 μg/L |
| Vitamin B12 | 120-1400 nmol/L | |
| Folate | (red cell) (serum) | 360-1400 nmol/L 7-45 nmol/L |
Activated partial thromboplastin time (APTT)
| 25-35 seconds 1.5-2.5 x baseline |
| Prothrombin time (PT) | 11-15 seconds |
International normalised ration (INR)
| 1.0-4.5 |
| Fibrinogen | 1.5-4.0 g/L |
| Rheumatoid factor (nephelometry) | <30 IU/L |
| C3 | 0.9-1.8 g/L |
| C4 | 0.16-0.50 g/L |
| C-reative protein | <5.0 mg/L |
Immunoglobin:
| 6.5-16.0 g/L 0.6-4.0 g/L 0.5-3.0 g/L |
| Adult | |
|---|---|
| Total lymphocytes | 1.5-4.0 |
| CD3 | 0.6-2.4 |
| CD4 (T4) | 0.5-1.4 |
| CD8 (T8) | 0.2-0.7 |
| CD19 | 0.04-0.5 |
| CD16 | 0.2-0.4 |
| CD4/CD8 ratio | 1.0-3.2 |
Appendix 13.2: New classification and criteria for diagnosis of diabetes mellitus
AMA5 Chapter 8 (p 173) applies to the assessment of permanent impairment of the skin, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
14.1 AMA5 Chapter 8 (pp 173–90) refers to skin diseases generally rather than work related skin diseases alone. This chapter has been adopted for measuring impairment of the skin system, with the following variations.
14.2 Disfigurement, scars and skin grafts may be assessed as causing significant permanent impairment when the skin condition causes limitation in the performance of activities of daily living (ADL).
14.3 For cases of facial disfigurement, refer to Table 6.1 in Chapter 6 of in the Guidelines.
14.4 AMA5 Table 8-2 (p 178) provides the method of classification of impairment due to skin disorders. Three components – signs and symptoms of skin disorders, limitations in ADL and requirements for treatment – define five classes of permanent impairment. The assessing specialist should derive a specific percentage impairment within the range for the class that best describes the clinical status of the claimant.
14.5 The skin is regarded as a single organ and all non-facial scarring is measured together as one overall impairment, rather than assessing individual scars separately and combining the results.
14.6 A scar may be present and rated as 0% WPI.
Note that uncomplicated scars for standard surgical procedures do not, of themselves, rate an impairment.
14.7 The table for the evaluation of minor skin impairment (TEMSKI) (see Table 14.1 below) is an extension of Table 8-2 in AMA5. The TEMSKI divides class 1 of permanent impairment (0–9%) due to skin disorders into five categories of impairment. The TEMSKI may be used by trained assessors (who are not trained in the skin body system), for determining impairment from 0–4% in the class 1 category, that has been caused by minor scarring following surgery. Impairment greater than 4% must be assessed by a specialist who has undertaken the requisite training in the assessment of the skin body system.
14.8 The TEMSKI is to be used in accordance with the principle of ‘best fit’. The assessor must be satisfied that the criteria within the chosen category of impairment best reflect the skin disorder being assessed. If the skin disorder does not meet all of the criteria within the impairment category, the assessor must provide detailed reasons as to why this category has been chosen over other categories.
14.9 Where there is a range of values in the TEMSKI categories, the assessor should use clinical judgement to determine the exact impairment value.
14.10 The case examples provided in AMA5 Chapter 8 do not, in most cases, relate to permanent impairment that results from a work-related injury. The following NSW examples are provided for information.
14.11 Work-related case study examples 14.1–14.6 are included below, in addition to AMA5 examples 8.1–8.22 (pp 178–87).
Table 14.1: Table for the evaluation of minor skin impairment (TEMSKI)
| Criteria | 0% WPI | 1% WPI | 2% WPI | 3-4% WPI | 5-9% WPI* |
|---|---|---|---|---|---|
Description of the scar(s) and/or skin conditions(s) | Claimant is not conscious or barely conscious of the scar(s) or skin condition. Good colour match with surrounding skin, and the scar(s) or skin condition is barely distinguishable. Claimant is unable to easily locate the scar(s) or skin condition. No trophic changes. | Claimant is conscious of the scar(s) or skin condition. Some parts of the scar(s) or skin condition colour contrast with the surrounding skin as a result of pigmentary or other changes. Claimant is able to locate the scar(s) or skin condition. Minimal trophic changes. Any staple or suture marks are visible. | Claimant is conscious of the scar(s) or skin condition. Noticeable colour contrast of scar(s) or skin condition with surrounding skin as a result of pigmentary or other changes. Claimant is able to easily locate the scar(s) or condition. Trophic changes evident to touch. Any staple or suture marks are clearly visible. | Claimant is conscious of the scar(s) or skin condition. Easily identifiable colour contrast of scar(s) or skin condition with surrounding skin as a result of pigmentary or other changes. Claimant is able to easily locate the scar(s) or skin condition. Trophic changes evident to touch. Any staple or suture marks are clearly visible. | Claimant is conscious of the scar(s) or skin condition. Distinct colour contrast of scar(s) or skin condition with surrounding skin as a result of pigmentary or other changes. Claimant is able to easily locate the scar(s) or skin condition. Trophic changes are visible. Any staple or suture marks are clearly visible. |
Location | Anatomic location of the scar(s) or skin condition not clearly visible with usual clothing/hairstyle. | Anatomic location of the scar(s) or skin condition not usually visible with usual clothing/hairstyle. | Anatomic location of the scar(s) or skin condition is usually visible with usual clothing/hairstyle. | Anatomic location of the scar(s) or skin condition is visible with usual clothing/hairstyle. | Anatomic location of the scar(s) or skin condition is usually and clearly visible with usual clothing/hairstyle. |
Contour | No contour defect. | Minor contour defect. | Contour defect visible. | Contour defect easily visible. | Contour defect easily visible. |
ADL/treatment | No effect on any ADL. No treatment, or intermittent treatment only, required. | Negligible effect on any ADL. No treatment, or intermittent treatment only, required. | Minor limitation in the performance of few ADL. No treatment, or intermittent treatment only, required. | Minor limitation in the performance of few ADL and exposure to chemical or physical agents (eg sunlight, heat, cold etc) may temporarily increase limitation. No treatment, or intermittent treatment only, required. | Limitation in the performance of few ADL (including restriction in grooming or dressing) and exposure to chemical or physical agents (eg sunlight, heat, cold etc) may temporarily increase limitation or restriction. No treatment, or intermittent treatment only, required. |
Adherence to underlying structures | No adherence. | No adherence. | No adherence. | Some adherence. | Some adherence. |
This table uses the principle of 'best fit'. You should assess the impairment to the whole skin system against each criteria and then determine which impairment category best fits (or describes) the impairment. Refer to 14.8 regarding application of this table.
Examples
| Subject | 42-year-old man |
|---|---|
| History | Spray painter working on ships in dry dock. Not required to prepare surface but required to mix paints (including epoxy and polyurethane) with ‘thinners’ (solvents) and spray metal ships’ surface. At end of each session, required to clean equipment with solvent. Not supplied with gloves or other personal protective equipment until after onset of symptoms. Gradual increase in severity in spite of commencing to wear gloves. Off work two months leading to clearance, but frequent recurrence, especially if the subject attempted prolonged work wearing latex or PVC gloves or wet work without gloves. |
| Current | Returned to dry duties only at work. Mostly clear of dermatitis, but flares. |
| Physical examination | Varies between no abnormality detected to mild dermatitis of the dorsum of hands. |
| Investigations | Patch test standard + epoxy + isocyanates (polyurethanes) - no reactions |
| Impairment | 0% |
| Comment | No interference with ADL. |
| Subject | 30-year-old woman |
|---|---|
| History | Hairdresser 15 years, with six-month history of hand dermatitis, increasing despite beginning to wear latex gloves after onset. Dermatitis settled to very mild after four weeks off work, but not clear. As the condition flared whenever the subject returned to hairdressing, she ceased and is now a computer operator. |
| Current | Mild continuing dermatitis of the hands, which flares when doing wet work (without gloves) or when wearing latex or PVC gloves. Has three young children and impossible to avoid wet work. |
| Investigation | Patch test standard + hairdressing series - possible reaction to paraphenylene diamine. |
| Impairment | 5% |
| Comment | Able to carry out ADL with difficulty, therefore limited performance of some ADL. |
| Subject | 43-year-old man |
|---|---|
| History | Concreter since age 16. Eighteen-month history of increasing hand dermatitis, eventually on dorsal and palmar surface of hands and fingers. Off work, and treatment led to limited improvement only. |
| Physical examination | Fissured skin, hyperkeratotic chronic dermatitis. |
| Investigation | Patch test - positive reaction to dichromate. |
| Current | Intractable, chronic, fissured dermatitis. |
| Impairment | 12% |
| Comment | Unable to obtain any employment because has chronic dermatitis, and is on disability support pension. Difficulty gripping items, including steering wheel, hammer and other tools. Unable to do any wet work (eg painting). Former home handyman, now calls in tradesman to do any repairs and maintenance. Limited performance in some ADL. |
| Subject | 40-year-old female nurse |
|---|---|
| History | Six-month history of itchy hands minutes after applying latex gloves at work. Later swelling and redness associated with itchy hands and wrists, and subsequently widespread urticaria. One week off led to immediate clearance. On return to work wearing PVC gloves, developed anaphylaxis on first day back. |
| Physical examination | No abnormality detected or generalised urticaria/angioedema. |
| Investigation | Latex radioallergosorbent test, strong response. |
| Current | The subject experiences urticaria and mild anaphylaxis if she enters a hospital, some supermarkets or other stores (especially if latex items are stocked), at children’s parties, or in other situations where balloons are present, or on inadvertent contact with latex items, including sporting goods handles, some clothing and many shoes (latex-based glues). Also has restricted diet (must avoid bananas, avocados and kiwi fruit). |
| Impairment | 17% |
| Comment | Severe limitation in some ADL in spite of intermittent activity. |
| Subject | 53-year-old married man |
|---|---|
| History | Road worker since 17 years of age. Has had a basal cell carcinoma on the left forehead, squamous cell carcinoma on the right forehead (graft), basal cell carcinoma on the left ear (wedge resection) and squamous cell carcinoma on the lower lip (wedge resection) excised since 45 years of age. No history of loco-regional recurrences. Multiple actinic keratoses treated with cryotherapy or Efudix over 20 years (forearms, dorsum of hands, head and neck). |
| Current | New lesion right preauricular area. Concerned over appearance - 'I look a mess'. |
| Physical examination | Multiple actinic keratoses forearms, dorsum of hands, head and neck. Five millimetre diameter nodular basal cell carcinoma right preauricular area; hypertrophic red scar, 3cm length, left forehead; 2cm-diameter graft site (hypopigmented with 2mm contour deformity) right temple; non-hypertrophic scar left lower lip (vermilion) with slight step deformity; and non-hypertrophic pale wedge resection scar left pinna, leading to 30% reduction in size of the pinna. Graft sites taken from right post-auricular area. No regional lymphadenopathy. |
| Impairment rating | 6% |
| Comment | Refer to Table 6.1 (facial disfigurement) in Chapter 6. |
| Subject | 35-year-old single female professional surf life saver |
|---|---|
| History | Occupational outdoor exposure since 19 years of age. Basal cell carcinoma on tip of nose excised three years ago with full thickness graft following failed intralesional interferon treatment. |
| Current | Poor self-esteem because of cosmetic result of surgery. |
| Physical examination | One-centimetre diameter graft site on the tip of nose (hypopigmented with 2mm depth contour deformity, cartilage not involved). Graft site taken from right post-aricular area. |
| Impairment | 10% |
| Comment | Refer to Table 6.1 (facial disfigurement) in Chapter 6. |
AMA5 chapters 3 and 4 (pp 23 and 65) apply to the assessment of permanent impairment of the cardiovascular system, subject to the modifications set out below. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
15.1 The cardiovascular system is discussed in AMA5 chapters 3 (Heart and Aorta) and 4 (Systemic and Pulmonary Arteries) (pp 25–85). These chapters can be used to assess permanent impairment of the cardiovascular system with the following minor modifications.
15.2 It is noted that in these chapters there are wide ranges for the impairment values in each category. When conducting an assessment, assessors should use their clinical judgement to express a specific percentage within the range suggested.
Exercise stress testing
15.3 As with other investigations, it is not the role of an assessor to order exercise stress tests purely for the purpose of evaluating the extent of permanent impairment.
15.4 If exercise stress testing is available, then it is a useful piece of information in arriving at the overall percentage impairment.
15.5 If previous investigations are inadequate for a proper assessment to be made, the assessor should consider the value of proceeding with the evaluation of permanent impairment without adequate investigations and data (see Chapter 1 of the Guideline – ordering of additional investigations).
Permanent impairment – maximum medical improvement
15.6 As for all assessments, maximal medical improvement is considered to have occurred when the worker’s condition is well stabilised and unlikely to change substantially in the next year, with or without medical treatment.
Vascular diseases affecting the extremities
15.7 Note that in this section, AMA5 tables 4-4 and 4-5 (p 76) refer to percentage impairment of the upper or lower extremity. Therefore, an assessment of impairment concerning vascular impairment of the arm or leg requires that the percentages identified in these tables be converted to whole person impairment (WPI). The table for conversion of the upper extremity is AMA5 Table 16-3 (p 439), and the table for conversion of the lower extremity is AMA5 Table 17-3 (p 527).
Thoracic outlet syndrome
15.8 Impairment due to thoracic outlet syndrome is assessed according to AMA5 Chapter 16, relating to the upper extremities, and Chapter 2 of the Guidelines.
AMA5 Chapter 6 (p 117) applies to the management of permanent impairment of the digestive system. Before undertaking an impairment assessment, users of the Guidelines must be familiar with:
- the Introduction in the Guidelines
- chapters 1 and 2 of AMA5
- the appropriate chapter(s) of the Guidelines for the body system they are assessing.
- the appropriate chapter(s) of AMA5 for the body system they are assessing.
The Guidelines take precedence over AMA5.
Introduction
16.1 The digestive system is discussed in AMA5 Chapter 6 (pp 117–42). This chapter can be used to assess permanent impairment of the digestive system.
16.2 AMA5 Section 6.6, ‘Hernias’ (p 136): Occasionally in regard to inguinal hernias, there is damage to the ilioinguinal nerve following surgical repair. Where there is loss of sensation in the distribution of the ilio-inguinal nerve involving the upper anterior medial aspect of the thigh, a 1% WPI should be assessed as per Table 5.1 in Chapter 5 of the Guidelines. This assessment should not be made unless the symptoms have persisted for 12 months.
16.3 Where, following repair, there is severe dysaesthesia in the distribution of the ilio inguinal nerve, a maximum of 5% whole person impairment (WPI) may be assessed as per Table 5.1 in Chapter 5 of the Guidelines. This assessment should not be made unless the symptoms have persisted for 12 months.
16.4 Where, following repair of a hernia of the abdominal wall, there is residual persistent excessive induration at the site, which is associated with significant discomfort, this should be assessed as a class 1 herniation (AMA5 Table 6-9, p 136). This assessment should not be made unless symptoms have persisted for 12 months.
16.5 Impairments due to nerve injury and induration cannot be combined. The higher impairment should be chosen.
16.6 A person who has suffered more than one work-related hernia recurrence at the same site and who now has limitation of activities of daily living should be assessed as herniation class 1 (AMA5 Table 6-9, p 136).
16.7 A diagnosis of a hernia should not be made on the findings of an ultrasound examination alone. For the diagnosis of a hernia to be made there must be a palpable defect in the supporting structures of the abdominal wall and either a palpable lump or a history of a lump when straining.
16.8 A divarication of the rectus abdominus muscles in the upper abdomen is not a hernia, although the supporting structures have been weakened, they are still intact.
16.9 Effects of analgesics on the digestive tract:
- AMA5 Table 6-3 (p 121) Class 1 is to be amended to read ‘there are symptoms and signs of digestive tract disease’.
- Nonsteroidal anti-inflammatory agents, including Aspirin, taken for prolonged periods can cause symptoms in the upper digestive tract. In the absence of clinical signs or other objective evidence of upper digestive tract disease, anatomic loss or alteration a 0% WPI is to be assessed.
- Effects of analgesics on the lower digestive tract:
- Constipation is a symptom, not a sign and is generally reversible. A WPI assessment of 0% applies to constipation.
- Irritable bowel syndrome without objective evidence of colon or rectal disease is to be assessed at 0% WPI.
- Assessment of colorectal disease and anal disorders requires the report of a treating doctor or family doctor, which includes a proper physical examination with rectal examination if appropriate, and/or a full endoscopy report.
- Failure to provide such reports may result in a 0% WPI.
16.10 Splenectomy: Post-traumatic splenectomy or functional asplenia following abdominal trauma should be assessed as 3% WPI.
16.11 Abdominal adhesions: Intra-abdominal adhesions following trauma requiring further laparotomy should be assessed according to AMA5 Table 6-3 (p 121).
(exclude AMA5 Chapter 18)
17.1 The International Association for the Study of Pain (IASP) has defined pain as:
‘An unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage’.
17.2 For chronic pain assessment using AMA5 and the Guidelines, exclude AMA5 Chapter 18, on pain (p 565–91).
17.3 The reasons for excluding chronic pain, as a separate condition from the Guidelines are:
- It is a subjective experience and is, therefore, open to exaggeration or fabrication in the compensation setting. Assessment depends on the credibility of the subject being assessed. In order to provide reliability, applicants undergoing pain assessments require more than one examiner at different times, concordance with the established conditions, consistency over time, anatomical and physiological consistency, agreement between the examiners and exclusion of inappropriate illness behaviour.
- Pain cannot be measured and no objective assessment can be made.
- Tools to measure pain are based on self-reports and may be inherently unreliable.
- Some impairment ratings take symptoms into account and some of the ranges of impairment – eg whole person impairment (WPI) of the spine, may reflect the effect of the injury and pain on activities of daily living (ADL). This is not so for impairment assessment of the upper and lower limb, which is based on range of movement and diagnosis-based estimates, other than for peripheral nerve injury.
17.4 Where there is a peripheral nerve injury and there is sensory loss, some of the sensory nerve impairment categories permit pain to be included (AMA5 Table 16-10, categories 1-5, p 482).
17.5 AMA5 Section 17.2m, ‘Causalgia and complex regional pain syndrome (reflex sympathetic dystrophy)’ (p 553), should not be used. AMA5 Table 16-16 (p 496) has been replaced by Table 17.1 (below) in the Guidelines. Table 17.1 is used to determine if complex regional pain syndrome (CRPS) is a rateable diagnosis. It is important to exclude diagnoses that may mimic CRPS, such as disuse atrophy, unrecognised general medical problems, somatoform disorders and factitious disorder. Once the diagnosis is established, assess impairment as in AMA5.
For Complex Regional Pain Syndrome Type 1 (CRPS1) to be present for the purposes of assessment:
- the diagnosis is to be confirmed by criteria in Table 17.1 (below)
- the diagnosis has been present for at least one year (to ensure accuracy of the diagnosis and to permit adequate time to achieve maximum medical improvement)
- the diagnosis has been verified by more than one examining physician
- other possible diagnoses have been excluded.
- CRPS1 is to be assessed as follows:
- Apply the diagnostic criteria for complex regional pain syndrome type 1 (Table 17.1).
Table 17.1: Diagnostic criteria for Complex Regional Pain Syndrome types 1 and 2
1. Continuing pain, which is disproportionate to any casual event. |
2. Must report at least one symptom in each of the following four categories:
|
3. Must display at least one sign* at time of evaluation in all of the following four categories:
|
4. There i no other diagnosis that better explains the signs and symptoms. *A sign is included only if it is observed and documented at time of the impairment evaluation. |
Then consider the following in assessing CRPS1:
- If the criteria in each of the sections 1, 2, 3 and 4 in Table 17.1, above, are satisfied, the diagnosis of CRPS1 may be made.
- Rate the extremity impairment resulting from loss of motion of each individual joint involved.
- Rate the extremity impairment resulting from sensory deficits and pain, according to the grade that best fits the degree or amount of interference with ADL, as described in AMA5 Table 16.10a (p 482). Use clinical judgement to select the appropriate severity grade and the appropriate percentage from within the range shown in each grade. The maximum value is not automatically applied. The value selected represents the extremity impairment. A nerve value multiplier is not used.
- Combine the extremity impairment for loss of joint motion with the impairment for pain or sensory deficit using the Combined Values Chart (AMA5, p 604) to obtain the final extremity impairment.
- Convert the final extremity impairment to WPI using AMA5 Table 16.3, (p 439) for the upper extremity and AMA5 Table 17.3 (p 527) for the lower extremity.
For Complex Regional Pain Syndrome Type 2 (CRPS2), the mechanism is an injury to a specific nerve. The methodology in AMA5 (pp 496–97) is to be followed:
- If the criteria in each of sections 1, 2, 3 and 4 in Table 17.1, above, are satisfied and there is objective evidence of an injury to a specific nerve, the diagnosis of CRPS2 may be made.
- Rate the extremity impairment due to loss of motion of each individual joint involved.
- Rate the extremity impairment resulting from sensory deficits and pain of the injured nerves according to the determination methods described in AMA5 Chapter 16, Section 16.5b and Table 16-10a. Use clinical judgement to select the appropriate severity grade and the appropriate percentage from within each range shown in the grade.
- Rate the extremity impairment resulting from motor deficits and the loss of power of the injured nerve according to the determination method in AMA5 Chapter 16, Section 16.5b and Table 16-11a.
- Combine the extremity impairment percentages for loss of range of motion of the joints involved, pain or sensory deficits, and motor deficits, if present, to determine the final extremity impairment, using the Combined Values Chart in AMA5 (p 604).
- Convert the final extremity impairment to WPI using AMA5 Table 16.3 (p 439) for the upper extremity and AMA5 Table 17.3 (p 527) for the lower extremity.
| Term | Definition |
|---|---|
AMA5 | The 5th edition of the American Medical Association’s (AMA) Guides to the evaluation of permanent impairment and any published errata. |
AMA4 | The 4th edition of the American Medical Association’s (AMA) Guides to the evaluation of permanent impairment. |
Medical Assessor | For the purposes of the Workplace Injury Management and Workers Compensation Act 1998, medical assessors are decision-makers appointed by the President of the Personal Injury Commission under the PIC Act1. |
Assessor | An assessor will be a registered medical practitioner recognised as a medical specialist.
The assessor will have qualifications, training and experience relevant to the body system being assessed. The assessor will have successfully completed requisite training in using the Guidelines for each body system they intend on assessing. They will be listed as a trained assessor of permanent impairment for each relevant body system(s) on the State Insurance Regulatory Authority website. |
Degree of impairment | The degree of permanent impairment as assessed according to section 65 of the Workers Compensation Act 1987. |
Injury | A personal injury arising out of or in the course of employment and includes a disease injury. |
Maximum medical improvement (MMI) | This is considered to occur when the worker’s condition is well stabilised and is unlikely to change substantially in the next year, with or without medical treatment. |
The Guidelines | The NSW workers compensation guidelines for the evaluation of permanent impairment. |
Secondary injury | Means an injury to the extent that it arises as a consequence of, or secondary to, another injury. |
The Legislation | The Workers Compensation Act 1987 The Workplace Injury Management and Workers Compensation Act 1998 and the regulations made under those Acts. |
1. Consequent to the enactment of the PIC Act the WIMWC Act is amended to omit references to ‘approved medical specialist’ and instead insert ‘medical assessor’.
Permanent impairment coordinating committees
| Name | Position |
|---|---|
| Mr Gary Jeffery | Chair |
| Mr Kim Garling | WorkCover Independent Review Officer |
| Ms Alisha Wilde/ Mr Shay Degaura | Unions NSW |
| Dr Mark Burns | Australian Faculty of Occupational and Environmental Medicine |
| Associate Professor Michael Fearnside | Associate Professor of Neurosurgery, Neurosurgical Society of Australasia |
| Dr John Harrison | Orthopaedic Surgeon, Australian Orthopaedic Association, Australian Society of Orthopaedic Surgeons |
| Dr Yvonne Skinner | Psychiatrist, Royal Australian and New Zealand College of Psychiatrists |
| Prof Ian Cameron | Professor of Rehabilitation Medicine, Australasian Faculty of Rehabilitation Medicine |
| Dr Roger Pillemer | Workers Compensation Commission, Senior Approved Medical Specialist |
| Dr Michael Gliksman | Australian Medical Association |
| Dr Neil Berry | Royal Australasian College of Surgeons |
| Mr Kevin Gillingham | WorkCover WA |
| Mr David Caulfied/Mr Phil Waddas | WorkCover SA |
| Ms Meg Brighton | WorkSafe ACT |
| Name | Position |
|---|---|
| Mr Rob Thomson | Chair |
| Ms Mary Yaager | Unions NSW |
| Dr Ian Gardner | Workers Compensation and Workplace Occupational Health and Safety Council of NSW |
| Associate Professor Michael Fearnside | Associate Professor of Neurosurgery, Neurosurgical Society of Australasia |
| Dr John Harrison | Orthopaedic Surgeon, Australian Orthopaedic Association, Australian Society of Orthopaedic Surgeons |
| Dr Yvonne Skinner | Psychiatrist, Royal Australian and New Zealand College of Psychiatrists |
| Prof Roger Pillemer | Approved Medical Specialist |
| Dr Michael Gliksman | Australian Medical Association |
| Dr Neil Berry | Royal Australasian College of Surgeons |
| Name | Position |
|---|---|
| Dr Jim Stewart | Chair |
| Ms Kate McKenzie | WorkCover |
| Mr John Robertson | Labor Council of NSW |
| Ms Mary Yaager | Labor Council of NSW |
| Dr Ian Gardner | Medical Representative to Workers Compensation and Workplace Occupational Health and Safety Council of NSW |
| Dr Stephen Buckley | Rehabilitation Physician |
| Prof Michael Fearnside | Professor of Neurosurgery |
| Dr John Harrison | Orthopaedic Surgery |
| Dr Jonathan Phillips | Psychiatrist |
| Prof Bill Marsden | Professor of Orthopaedic Surgery |
| Dr Dwight Dowda | Occupational Physician |
| Associate Professor Ian Cameron | Associate Professor of Rehabilitation Medicine |
| Dr Robin Chase | Australian Medical Association |
| 2005 revisions | |
| Dr Roger Pillemer | Orthpaedic Surgeon |
| Dr John DIxon Hughes | General Surgeon |
| Dr Yvonne Skinner | Psychiatrist |
Working groups
Updated 21 January 2025