- Print this page
- Share this page
A PDF of this guide is available for download
Guidelines for the provision of relevant services have been published
SIRA has published the Guidelines for the Provision of Relevant Services (Health and Related Services), which apply to relevant service providers providing services in the NSW workers compensation and CTP schemes. The following sections of the Guidelines apply to medical practitioners providing relevant services in the workers compensation scheme:
- Part 1: Code of conduct
- Part 2: Requirements for telehealth services
- Part 3:Administrative requirements for prescription of medication
- Part 5: Billing requirements for the provision of relevant services under the workers compensation legislation
- Part 6: Invoicing requirements for relevant services under the workers compensation legislation (excluding pharmaceutical services)
- Part 8: Application of the Guidelines by relevant service/provider
This webpage has been updated to include content from the Guidelines and the associated legislation.

Introduction
The worker and you
Under the workers compensation system, your patient is referred to as a worker. A worker with a work related injury or illness is encouraged to choose their own doctor. This is often their usual general practitioner or family doctor.
The doctor’s role is defined by workers compensation legislation and, as such, there are certain obligations you must meet. Your primary objective is to support the worker to optimise their recovery. This is generally achieved through a recovery at work plan involving a combination of clinical intervention and injury management.
This guide also explains the roles of others in the worker’s support team. The support team will include you, the employer and insurer, along with any approved workplace rehabilitation providers and/or allied health practitioners involved in treatment.
Advice and direction in this guide is based on a strong body of research about the health benefits of good work, and how returning to and, where possible, recovering at work after an injury, can promote healing and facilitate recovery.
This guide will help you to work with the support team to determine what the worker can do, rather than what they can’t.
Your role in assessing the worker’s capacity will help the worker and employer identify suitable tasks to enable recovery at work. This interaction is critical in preventing long term disability and bringing about the best possible outcome for the worker.
Most injured workers take little or no time off work. For those that do, the vast majority (more than 80 per cent) return to and recover at work within the first 13 weeks.
Health benefits of good work
There is good evidence that:
- work is therapeutic and promotes recovery1
- safe work is good for you physically, socially, and financially2, 3
- time off work is often not medically necessary, and can delay recovery3
- the longer a worker is off work the less likely they are to ever return to work.4
Workers compensation in NSW
The State Insurance Regulatory Authority (SIRA) is the government organisation responsible for regulating the NSW workers compensation system.
There are three types of insurers in the NSW workers compensation system:
The Nominal Insurer is a statutory legal entity constituted by section 154A of the Workers Compensation Act 1987 (the Act). Under the Act, the Nominal Insurer is taken to be a licensed insurer and is responsible for managing the operation of the Workers Compensation Insurance Fund.
icare (Insurance and Care NSW) is a NSW Government agency that acts for the Nominal Insurer and provides services for authorities that provide insurance and compensation schemes in NSW. Those authorities are the:
- Workers Compensation (Dust Diseases) Authority
- Lifetime Care and Support Authority of New South Wales
- Sporting Injuries Compensation Authority
- NSW Self Insurance Corporation (SICorp).
The Nominal Insurer contracts scheme agents to manage policies and claims on its behalf. The three approved scheme agents are:
- Allianz Australia Worker’s Compensation (NSW) Limited
- Employers Mutual NSW Limited
- GIO General Limited.
Self-insurers are employers approved by SIRA to manage their own workers compensation claims.
Specialised insurers – hold a restricted licence to provide workers compensation insurance for a specific industry or class of business or employers.
Regardless of which type of insurer is involved, they all have an obligation to support employers, and workers in their recovery at/return to work, and manage claims to ensure they receive their entitlements.
NSW workers compensation certificate of capacity
This is the primary communication tool for the nominated treating doctor. It provides complete and accurate information to ensure the worker and their support team have a clear understanding of the worker’s recovery needs.
Your recommendations on the SIRA certificate of capacity help the employer and worker to identify suitable work options. The more detailed information you provide, the easier it is for the employer to identify and offer work that is a good match for the worker and their recovery.
There is comprehensive information on our website to help you complete the certificate.
Your role as the nominated treating doctor
While your usual role as a doctor involves assessing, diagnosing, treating and certifying patients, your role as a doctor in the workers compensation system also involves the following two responsibilities:
- to support the worker to return to, and where possible to recover at work, through appropriate clinical intervention and management
- to contribute to return to work and recover at work planning, in collaboration with the worker and other members of the support team.
Medical management
Assessment
In addition to your usual physical and/or psychological assessment, screening for psychosocial risk factors that may delay or present a barrier to recovery, forms an important part of the assessment of a worker presenting with a work related injury or illness.
Using acceptable medical terminology assists an insurance agent to make better decisions about a worker’s compensation claim. If diagnosis is unclear, provide a provisional diagnosis.
Treatment
You may identify medical and treatment related services likely to contribute to the worker’s successful recovery. These may include specialist treatment or workplace rehabilitation services as described in 'The worker's support team' section of this guide.
Prior approval is required from the insurer before recommended treatment can commence. There are some specific exemptions to this outlined in the 'Essential information for medical practitioners' section of this guide.
- must be directly related to the work related injury or illness and should be discussed with the worker to establish clear, realistic expectations about what treatment is likely to achieve
- should be included on the NSW workers compensation certificate of capacity so the insurer knows what services are required and what invoices to expect.
- experimental or not evidence-based
- not ‘reasonably necessary’ to support the worker to recover and stay at work
- not contributing to an objective improvement for the worker (particularly in relation to improving the worker’s capacity to work)
- provided by a person who is not appropriately registered, qualified or authorised.
Before approving or paying for a medical, hospital or rehabilitation treatment or service, an insurer must determine, based on the facts of each case, that the treatment or service:
- is reasonably necessary, and
- is required as a result of the work related injury or illness.
When considering the facts of the case, the insurer should understand that:
- what is determined as reasonably necessary for one worker may not be reasonably necessary for another work with a similar injury
- reasonably necessary does not mean absolutely necessary
- although evidence may show that a similar outcome could be achieved by an alternative treatment, it does not mean that the treatment recommended is not reasonably necessary.
In most cases, the above points should be sufficient for an insurer to determine what is reasonably necessary. Where the insurer remains unclear on whether a treatment is reasonably necessary, then the following factors may be considered:
- the appropriateness of the particular treatment
- the availability of alternative treatment
- the cost of treatment
- the actual or potential effectiveness of the treatment
- the acceptance of the treatments by medical experts.
Reviewing treatment effectiveness
Your role includes regularly reviewing the effectiveness of treatment with the worker and facilitating an evidence-based treatment approach. In particular this includes:
- ensuring timely progression of treatment to an active, self-management approach
- recommending cessation of treatment where there is no resulting objective improvement in function or work capacity within the expected time frame.
Certification
The SIRA certificate of capacity is the primary tool for you to communicate with all parties involved in the recover at work process. The certificate places emphasis on what the worker can do rather than what they cannot do.
A thoroughly completed certificate minimises the likelihood that an insurer will need to contact you to obtain additional information or clarification.
The certificate must include a clear diagnosis and treatment plan, as well as any factors that may have an impact on recovery. When stating the worker has capacity for work, you must complete the hours and days, as well as the ‘capacity’ section. If the worker has no capacity, you must provide an estimated time frame in which you think the worker will have some capacity.
The certificate should not cover a period of more than 28 days, unless clinical reasoning supporting a longer timeframe is provided. For example, in the case of a serious injury or where there is surgery planned and recovery is known to be prolonged.
The insurer will use the certificate as one source of information when making decisions regarding the worker’s work capacity. Further information on completing the certificate is available on our website.
Frequently asked questions about medical management
When an insurer reviews any request for treatment, they consider all medical evidence. If the medical evidence indicates the recommended treatment is not reasonably necessary, it may be refused.
This evidence may be obtained from a number of sources, such as a treating specialist, independent allied health practitioner or an independent medical examiner.
If the worker wants to dispute this decision, they should contact the insurer in the first instance. If the worker is unable to resolve the matter directly with the insurer they can contact the Independent Review Office (IRO). IRO can advise the worker (or their representative) about how to get advice from a lawyer approved under the Independent Legal Assistance and Review Service (ILARS). The lawyer will review the workers case and may make an application to IRO to see if funding is available to have the dispute resolved by the Personal Injury Commission.
Yes, if the worker agrees and the specialist is willing to be available to communicate effectively with all parties, for example taking phone calls or participating in case conferences. If they cannot commit to being available for this, it is better for a local GP to be the nominated treating doctor.
Not usually, but if information is not available within a reasonable period of time, the worker can be sent for an independent medical examination. For further information on independent medical examiners, refer to 'The worker's support team' section or our website.
If you identify barriers to recovery that are not directly related or attributable to the work related injury or illness (for example a pre-existing psychological condition) ensure the worker receives the necessary treatment and/or medication using the appropriate mechanisms for example Medicare or private health fund. You should discuss the impact of the interaction between work and non‑work related factors with the worker.
If you feel it is appropriate to talk to the insurer about any non-work related issue, you should seek consent from the worker to do so. It may not be necessary to disclose all details but rather flag the existence of a barrier and advise that management will occur concurrently with the work related injury or illness.
Recover at work
You can contribute to a worker’s successful recovery at work in a number of ways:
Talk to the employer
Ask the employer about their plan to support the recover at work process. This can include:
- the nature of suitable work options
- hours of available work
- equipment or changes to the working environment.
Talk to the worker about their job
Ask the worker about:
- their work tasks and associated work demands
- the work environment (physical environment and support mechanisms)
- what they think they could do at work while recovering from their injury
- what activities they are doing at home
- any support they think they may require to recover at work.
Correcting misconceptions and discussing the health benefits of good work
Workers have their own beliefs and expectations about health and work. These don’t always align with available evidence and may be unhelpful for their long term health.
There is evidence that the long term consequences of time off work may be greater than the consequences of the original health problem.5 This provides a platform to discuss the health benefits of good work. As the worker is likely to be receptive to your opinion, simple messages delivered in a clinical environment can assist workers to develop an evidence-based view of the relationship between health and work.
Worker misconceptions and evidence based responses6
The information below describes common misconceptions and provides supporting evidence to the contrary, with some messages to assist in your discussions with the worker about the health benefits of good work.
- there is often little or no underlying disease or permanent damage, and even if there is, incapacity is not inevitable
- clinical symptoms do not reliably correlate with findings on investigative imaging.
- treatment is beneficial when it is tailored to your work tasks
- clinical management is often about managing symptoms to allow you to continue or resume your usual activities at home and at work.
- staying active (including safe work) promotes recovery
- for most people with a work related injury, time off work is not medically necessary
- common health problems can often be accommodated at work with the necessary adjustments and support
- the longer a worker is off work, the less likely they are to ever return*.
*Johnson D, Fry T. Factors Affecting Return to Work after Injury: A study for the Victorian SIRA Authority. Melbourne: Melbourne Institute of Applied Economic and Social Research; 2002.
- employers must not dismiss a worker because of a work related injury within six months* from when they first become unfit as a result of the injury
- however, the worker must make reasonable efforts to return to suitable employment** with their pre-injury employer and, if this is not possible, with a different employer (see information on our vocational rehabilitation programs for a worker who cannot return to their pre-injury employment below).
* Section 248 of the Workers Compensation Act 1987
** Section 48(1) of the Workplace Injury Management and Workers Compensation Act 1998
Providing recommendations about work
On the certificate of capacity you must provide a recommendation about the worker’s capacity for work. You should consider the following when formulating your recommendation.
Determine what the worker can do
The SIRA certificate of capacity asks you to provide an opinion about what the worker can do in relation to specific tasks such as lifting, carrying, pushing, pulling, driving, standing or other considerations (for example psychological or cognitive) as relevant. You should focus on what the worker can do as opposed to what they cannot do. It may be helpful to ask the worker what activities they are performing at home that could transfer readily to their work environment.
If the worker is receiving treatment from an allied health practitioner they will be able to provide you with information regarding the worker's capacity. This will help you complete the certificate of capacity.
A worker may not be able to return to their usual work or usual hours immediately after their injury. Their employer is obliged to support the worker to recover at work. The information provided on the certificate of capacity can help the employer to find suitable work options.
- parts of the worker’s usual job
- the same job with reduced hours
- different tasks altogether
- work at a different site
- training opportunities
- a combination of some or all of the above.
Other forms of support, including provision of equipment, workplace modifications or changes in work practices to reduce work demands, may also be necessary to assist a worker to recover at work. You should note any support recommendations on the certificate of capacity.
Support the worker to recover at work
Given the health risks associated with long periods out of work, advice to stay off work should be viewed as a significant clinical intervention with potentially serious long term consequences.7 Accordingly, when assessing the worker's capacity consider if time off work is medically necessary or whether the worker could recover at work in some capacity with the right support.
If you feel further assessment may be helpful to inform your recommendations about work capacity, you may request a workplace or functional assessment. This involves the worker performing tasks which are assessed by an approved workplace rehabilitation provider.
The worker's support team
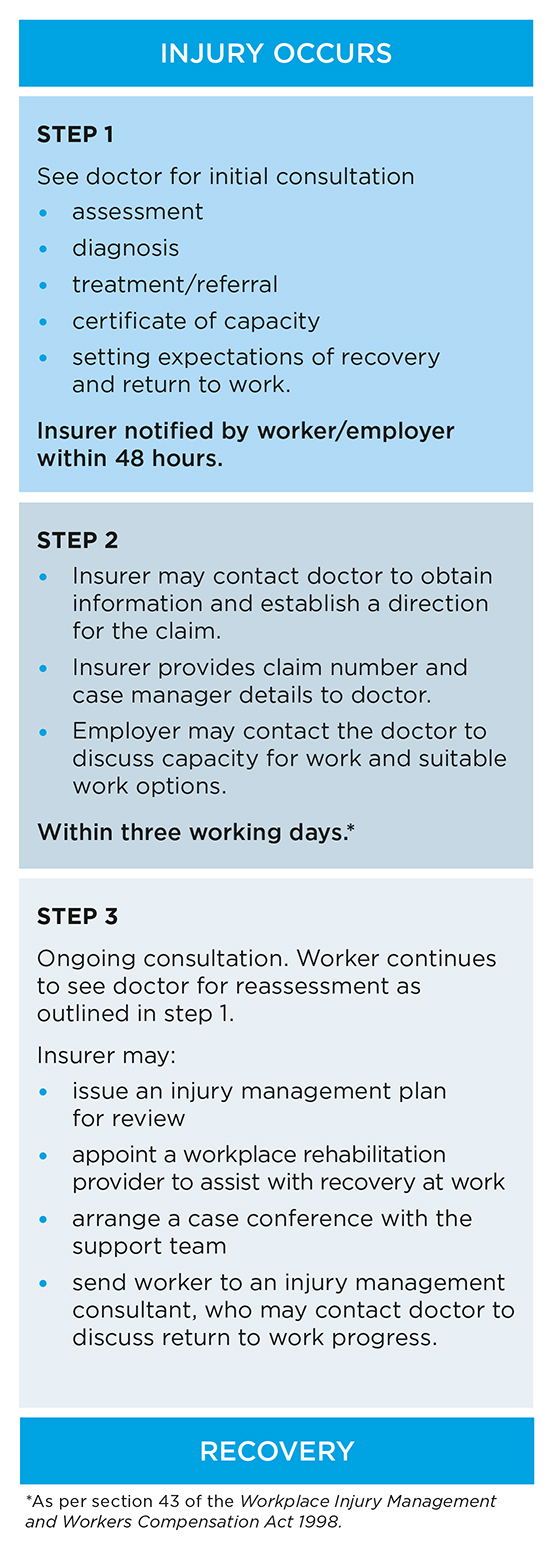
Success depends on the integration of sound clinical, workplace and insurance claims management, as well as agreement about the worker's goals and progress. That's why it is important you understand the role of others in the worker's support team.
The team includes the employer, insurer case manager, allied health practitioner, a workplace rehabilitation provider (if required) and you. Each member has an important role to play in the worker's recovery and these are outlined below.
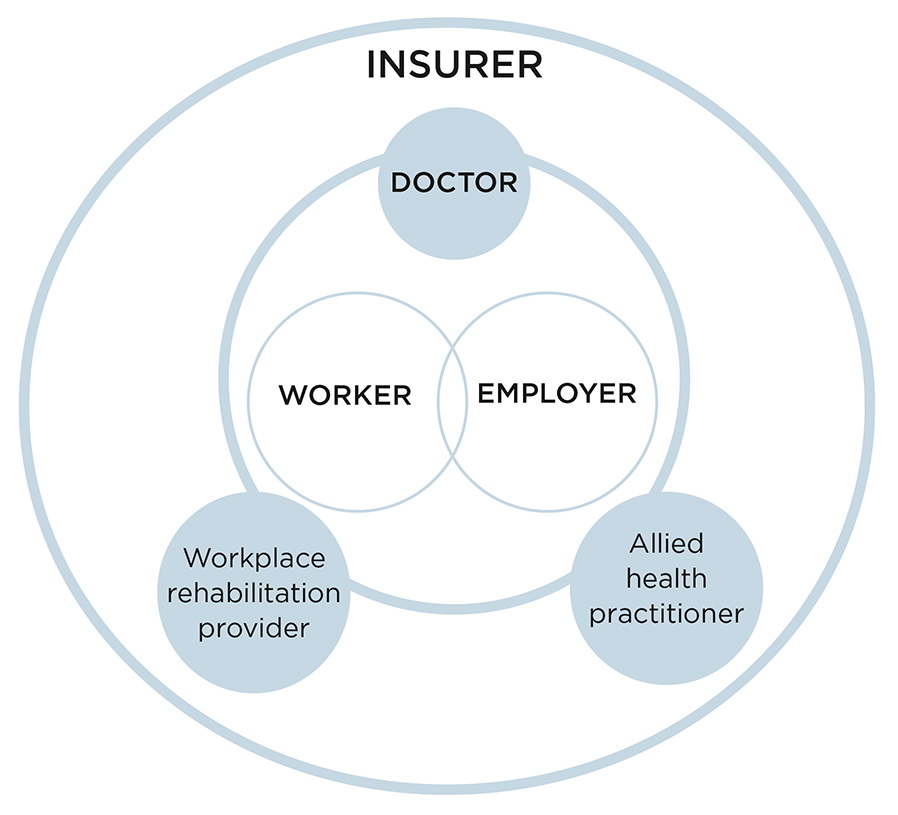
Evidence suggests that shared goals, communication and cooperation among the support team is critical in improving clinical and occupational outcomes for the worker.8
Worker
The worker’s primary role is to focus on returning to and recovering at work, in some capacity, as soon as possible. The worker’s responsibility is to ensure they receive the assistance they require, to remain focused and achieve their goals. This means:
- notifying their employer of their injury or illness as soon as possible
- consulting a doctor and obtaining a certificate of capacity and providing a copy to their employer and insurer
- attending reviews with their doctor and maintaining a current certificate of capacity
- actively participating in their treatment
- actively participating in their recover at work planning
- making reasonable efforts to return to their usual work or suitable work
- attending appointments and assessments arranged by the insurer case manager.
Employer
The employer is obliged to provide suitable work to support recovery at work.* The greater the employer’s ability to accommodate a worker while they recover, the less likely the worker will need time away from the workplace as a result of their injury. According to the legislation, this should be as far as possible, the same or equivalent work that was performed before the injury.**
The employer uses the recommendations you provide on the certificate of capacity to identify suitable work options in collaboration with the worker. The more information you provide, the easier it is for the employer to identify tasks that align with the worker’s current capacity for work.
You may find it helpful to contact the employer to discuss the worker’s needs or the employer may contact you.
The employer can assist you by:
- providing information about the workplace, the worker’s usual job and available short term suitable work options
- discussing any risks or barriers that may have an impact on the worker’s recovery
- developing a recover at work plan to ensure the worker’s recovery progresses as expected and they receive the support they need in the workplace.
Larger employers may have a return to work coordinator to assist them with their responsibilities. You may be dealing directly with the employer or their return to work coordinator.
* Section 49 of the Workplace Injury Management and Workers Compensation Act 1998
** Section 49(2) of the Workplace Injury Management and Workers Compensation Act 1998
Insurer case manager
The insurer case manager coordinates all aspects of a worker’s claim and is the primary contact for the worker and others involved in assisting the worker to return to and recover at work.
The insurer case manager:
- makes early contact with the worker, employer and you after receiving notification of a claim to determine the assistance the worker requires
- authorises and arranges payment for ‘reasonably necessary’ medical and related expenses (see the definition of reasonably necessary in the 'Your role as the nominated treating doctor' section)
- determines a worker’s entitlement to weekly compensation payments and commences payments
- assists the employer to meet their obligations to support the worker to recover at work
- may arrange assessments or services to help determine a worker’s capacity for work or identify suitable employment.
The information you provide on the SIRA certificate of capacity allows the insurance agent to promptly organise necessary support and services for the worker. You can contact the insurance agent at any stage to discuss specific needs, barriers or issues that may have an impact on the worker’s recovery at or return to work.
Other health practitioners
Other treatment practitioners may be involved in the management of the worker's injury/condition and may assist you to facilitate their recovery by:
- conducting a detailed assessment of the worker and providing information to inform and/or confirm diagnosis and the treatment strategy
- providing treatment to improve the worker’s capacity for work
- providing information about the worker’s progress to inform recommendations about capacity for work
- educating all parties about the health benefits of work.
SIRA approved workplace rehabilitation providers deliver specialised services to help employers meet their return to work obligations and assist workers to return to and recover at work.
The approved workplace rehabilitation provider assists you by:
- conducting a workplace or functional assessment to provide detailed information about the worker’s capacity for work, their pre-injury work and available suitable work options
- providing advice about reducing work demands through changes to a work environment or work practices
- collaborating with other members of the support team to identify and develop strategies to address barriers to recovery and develop a tailored recover at work plan. Our recover at work planning tool will assist you
- educating the worker and employer about their obligations and/or the health benefits of work
- conducting a vocational assessment to identify suitable employment options with a new employer (where appropriate)
- preparing and/or assisting the worker to obtain suitable employment with a new employer (where appropriate).
Referral to an approved workplace rehabilitation provider
You may consider recommending a referral on the NSW workers compensation certificate of capacity where:
- significant psychosocial barriers have an impact on recovery at work
- a worker’s injury is complex and/or recovery may be difficult or lengthy
- recovery is not progressing as expected
- there are communication issues, relationship breakdowns or conflict in the workplace
- suitable employment has not been offered and/or is not available
- additional information about the worker’s capacity for work, work options or work environment is required.
The insurer will discuss the referral with the worker, and engage an approved workplace rehabilitation provider.
Other medical practitioners
The independent medical examiner is a registered medical practitioner who provides an impartial medical assessment when requested by the worker, their legal representative or the insurer. A referral for an independent medical examination occurs when medical information is unavailable, inadequate, inconsistent and/or where these issues are not able to be resolved by other means.
The independent medical examiner may provide advice about accepting a claim, ongoing liability, the worker’s capacity for employment and/or ongoing treatment.
They may also recommend additional or alternative treatments if they believe it is in the interest of the worker. The independent medical examiner report goes to the person who requested the assessment.
See our page on medical practitioners for further information.
Methods of communicating with the support team
The Guidelines for the Provision of Relevant Services (Health and Related Services) make it a requirement for medical practitioners to work collaboratively and communicate in an effective and timely manner with members of the injured person’s support team about the injured person's injury, treatment, and recovery.
Regular communication with the support team will help facilitate a positive outcome for your patient. You may wish to make your preferences about communication known to the team, for example, preferred times and how you would like to be contacted. The table below outlines the key communication tools that you will encounter in your role as the nominated treating doctor.
The certificate of capacity is the primary communication tool for the nominated treating doctor to provide complete and accurate information to ensure everyone involved has a clear understanding of the worker’s needs.
In practice:
- Part A can be completed by the worker or doctor.
- Part B to be completed by the doctor.
- Part C is a declaration that the worker completes.
- The certificate is available on our website and in most medical software. For hard copies, call our publications hotline on 1300 799 003.
- Our website has detailed information about completing the certificate.
The injury management plan outlines the agreed support and plan for the worker in terms of treatment, rehabilitation and recovery at work. The insurer case manager, in consultation with the worker and others, completes this plan in the first four weeks post injury.
In practice:
- The insurer will include in the plan information on the certificate of capacity, and may contact the nominated treating doctor if clarification is required.
- You may receive copies of the plan and any updated plans throughout the recovery process.
The recover at work plan outlines the suitable work offered by the employer, other agreed workplace support, and stages or steps proposed to gradually progress the worker towards their usual work. It is completed by the employer and approved workplace rehabilitation provider (if involved).
In practice:
- The plan is developed by the employer and potentially an approved workplace rehabilitation provider in consultation with the worker.
- Input or endorsement may be required from you to ensure the plan meets the worker’s needs, and aligns with anticipated time frames for recovery.
- The worker may also bring a copy of the plan to their appointment with you to discuss progress and goals.
- A recover at work planning tool is available on our website.
A case conference is a face-to-face meeting, video conference or teleconference with any or all of the support team for the purpose of recover at work planning. Any member of the support team can instigate and manage a case conference.
In practice:
- A case conference should be booked in advance at a mutually convenient time, separate from the workers medical consultation unless you and the worker agree otherwise.
- The person initiating the case conference should provide an agenda with key points to be discussed.
- All parties involved should contribute openly and honestly when addressing the issues that led to the case conference being arranged.
- You must document the discussion, including those spoken to, key points discussed, agreed outcomes, and duration (for invoicing purposes) in your patient’s case notes.
- Case conferences may be billed in addition to the consultation using the appropriate payment classification code, see the Workers Compensation (Medical Practitioner Fees) Order for details, noting that treatment planning discussions between you and other treating practitioners are considered a normal interaction and are not chargeable.
Reports and information can be requested by the insurer case manager, legal provider, approved workplace rehabilitation provider or injury management consultant.
In practice:
- Requests from a worker’s legal representative for information that you have already provided to the insurer should be redirected to the insurer case manager.
- Information should be provided as soon as possible and within 10 working days to reduce delays for the worker.
- If you are unable to provide the information within a reasonable time frame, you should advise the requesting party as it may be possible to negotiate an extension, or they may choose to withdraw the request.
- Invoicing for reports that do not relate to the routine management of a worker’s injury, and are not required as part of a dispute or potential dispute, can be done as per the current fees order. If the report is requested as part of a current or potential dispute then the Workplace Injury Management and Workers Compensation (Medical Examinations and Reports) Order applies.
- Prepayment (in whole or part) cannot be made for reports.
SIRA requirements for medical practitioners
Code of conduct
Part 1 of the Guidelines for the Provision of Relevant Services (Health and Related Services) requires that medical practitioners:
- be appropriately registered, accredited, hold appropriate professional membership, and be qualified and experienced to provide the relevant service
- act in a professional, ethical, honest, and impartial way
- treat an injured worker with empathy, respect, and cultural safety
- comply with relevant provisions of the Guidelines for the Provision of Relevant Services (Health and Related Services), and relevant provisions of the workers compensation legislation and the regulations and guidelines made under that Act
- not engage in over servicing or engage in behaviour that leads to overbilling or delivering more services than necessary
- not provide, bill, or refer for relevant services, in a misleading or deceptive way intended to result in their financial or personal gain or another person or entity where the medical practitioner or the other person is not entitled to the financial or personal gain
- identify perceived, potential, and actual conflicts of interest and manage them to ensure services provided best meet the needs of the injured worker. Where there is an actual conflict, declare it to the injured person concerned, the referrer and the insurer concerned
- comply with the applicable laws in protecting injured person’s personal and health information
- work collaboratively and communicate in an effective and timely manner with members of the injured person’s support team (including the insurer) about the injured person's injury, treatment, and recovery
- respond to a request from SIRA for information relating to compliance with the Act, workers compensation legislation or motor accident legislation or the regulations or guidelines made under those Acts in the form, time and manner reasonably required and requested (including consistency with privacy legislation) by SIRA from time to time.
Telehealth requirements
Part 2 of the Guidelines for the Provision of Relevant Services (Health and Related Services) requires that medical practitioners must provide telehealth services:
- combination with in-person services unless the services are:
- psychiatric treatment services, or
- pre-approved by the insurer managing the injured person’s claim for delivery exclusively by telehealth.
- by videoconference unless it is unavailable. Email, SMS, or an app may only be used in conjunction with the delivery of telehealth via videoconference.
You must only provide telehealth services to an injured worker if:
- the injured worker requests or consents to participate in a telehealth service, and
- the practitioner determines that telehealth is appropriate for the injured worker concerned following consideration of the following factors:
- whether a physical assessment or treatment is required
- whether it will compromise worker outcomes
- availability of support at the injured worker’s location
- availability and access to a suitable device e.g., videoconferencing units/systems or a personal device capable of videoconferencing
- ability of the injured worker to participate, considering any physical, mental, social, and cognitive barriers
- ability to schedule telehealth session within the timeframes for a service
- the injured person's access to fast secure internet connection and sufficient internet or mobile data quota/allowance
- the injured person’s capability/capacity to access care this way.
Administrative requirements for prescriptions
Part 3 of the Guidelines for the Provision of Relevant Services (Health and Related Services) requires that medical practitioners prescribing or dispensing medication to an injured person must prescribe medications through the Pharmaceutical Benefits Scheme (PBS) where clinically appropriate and available.
You may provide a private prescription (not through the PBS) when:
- the medication is not available on the PBS, or
- the medication is available on the PBS, but the injured person does not meet the criteria for PBS prescribing, or
- the quantity of medication or number of repeats being prescribed for a medication available through the PBS is outside the PBS prescribing criteria, but can be clinically justified by the prescribing practitioner; or
- pre-approval has been obtained from the insurer to prescribe it privately (after the first month from the date of injury).
If you privately prescribe a high-risk medication (e.g., opioids, medication-assisted treatment of opioid dependency, injectable narcotics, benzodiazepines, Z-drugs, or medicinal cannabis) or drugs of addiction (Schedule 8), you must provide a written clinical rationale to the insurer that explains why:
- you are prescribing a medication that is not available through the PBS; or
- if it is available through the PBS, why you are prescribing it privately.
SIRA supervision of these requirements
SIRA recognises that the majority of medical practitioners providing services in the scheme are doing the right thing. However, SIRA may need to deal with practitioners with a pattern of poor practice who have not responded to opportunities provided by SIRA to correct those practices.
SIRA will ensure actions taken in response to non-compliance are appropriate, proportionate, and effective. Actions that could be taken in response to non-compliance may include:
- SIRA may contact the practitioner to discuss the matter, help identify the causes of non-compliance, and provide support and education to remedy any gaps in understanding.
- SIRA may write to the practitioner, informing them where they are not meeting requirements, how to comply with requirements, and that SIRA has the power to give a direction if requirements are not complied with.
Practitioners will be given the opportunity to make submissions about their behaviour and why further compliance activity is not warranted. It is expected that most matters will be remedied in discussion with the provider.
If non-compliance continues, SIRA may issue a direction under section 26D of the State Insurance and Care Governance Act 2015. A direction could include requiring the provider to take certain action or, if there is a risk of harm to injured workers or the scheme, suspend or exclude the practitioner from providing services in the CTP and WC schemes.
In general, SIRA will not investigate concerns about a medical practitioner’s clinical or professional conduct or intervene in individual clinical decision-making. If SIRA considers there is a potential risk to an injured worker’s health or welfare, SIRA may refer the matter to an appropriate body for investigation, such as the Health Care Complaints Commission, or the Health Professional Councils Authority.
Essential information for medical practitioners
Confidentiality of information
Medical practitioners should provide information relevant to the worker’s injury or illness to other relevant parties as part of the workers compensation process.
The worker provides consent on the certificate of capacity for you to communicate with parties involved in the management of their injury and claim. This generally includes the employer, other treating practitioners, insurer and workplace rehabilitation provider. It can also include an injury management consultant or the Personal Injury Commission (or an approved medical specialist).
If you receive a request for information and are concerned about the right of that party to obtain confidential information about the worker, you should establish that the request has been made with the worker’s consent. A copy of a signed and dated consent to disclose relevant confidential information to the party concerned is considered sufficient for the release of information.*
*Section 243 (1)(a) of the Workplace Injury Management and Workers Compensation Act 1998
You may provide medical notes relevant to the injury, however you are not obliged to, unless requested under direction (from the Personal Injury Commission), subpoena or other legal process that remains unchallenged.
It would not usually be necessary for an insurer to request an entire medical record, unless the record relates solely to the injury giving rise to the claim.
Where a worker is claiming a psychological injury or injury in the nature of a disease contracted by a gradual process, more extensive records may be required than would be necessary for a single event injury.
If you provide medical notes to the insurer, you can redact information that is not related to the workers compensation claim.
We suggest insurers pose specific questions to the medical practitioner allowing provision of information that is succinct and relevant to the purpose of the request.
If you receive requests from the insurer for information you have already provided, remind the insurer when the information was provided and confirm that it can be located on file.
Similarly, if you receive a request for what you believe to be an excessive amount of information, contact the insurer to discuss the issue.
If you are unsure about the information request or if you want advice on handling excessive requests for information contact our Doctors Helpline on 1800 661 111.
As per the Workers Compensation (Medical Practitioner Fees) Order the report will contain:
- the patient’s diagnosis and present condition
- the patient’s likely capacity for pre-injury work or suitable employment
- the need for treatment or additional rehabilitation
- medical co-morbidities that are likely to impact on the management of the worker’s condition (in accordance with privacy considerations).
An insurer may refer a worker to an injury management consultant when there are barriers to a worker’s recovery at or return to work. When you agree to be the nominated treating doctor to a worker, you are obliged to communicate with all relevant parties involved in their return to work.
No, an employer cannot insist that they or their representative is present during a consultation. However, if an employer (or their representative) accompanies the worker to the consultation, you can invite them in at the conclusion, to update them and work together in recover at work planning. The employer’s representative can be invited to attend a case conference provided the worker consents.
Yes, you can redact information that is not related to the workers compensation claim.
Payments and services for workers
The insurer is responsible for approval and payment of these services.
Medical and treatment services
There are a range of medical and treatment services you may recommend.
These may include:
- medical treatment, ambulance services
- allied health treatment
- workplace rehabilitation.
The insurer is responsible for coordinating and paying for services that are reasonably necessary.
Weekly payments
If a worker is unable to return to their usual work or work hours, they may be eligible to receive weekly compensation payments.
For most workers, this weekly payment is based on a percentage of their pre-injury average weekly earnings.
After 13 weeks, a worker's weekly payment amount may reduce depending on the worker's capacity for work and how many hours they are actually working.
Entitlement to long term payment support (after a maximum of 130 weeks) is only available if certain requirements are met.
SIRA vocational programs
SIRA funds programs to help workers who need additional assistance to recover at work. The insurer or SIRA approves these programs which can include:
- work experience/work trial with a host employer
- equipment and workplace modifications
- training to develop new skills and qualifications to keep their job or get a new job
- funds to address an immediate barrier preventing a worker from accepting an offer of suitable employment with a new employer (for example access to transport or suitable clothing)
- incentives to encourage employers to employ workers with a work related injury or illness.
Learn more about SIRA vocational programs.
Fees and payments for medical practitioners
Fees for medical practitioners in the workers compensation system can be found on our current health-related fees page.
The fees are based on the Australian Medical Association (AMA) List of Medical Services and Fees. Other SIRA-specific fees have been agreed with the relevant medical association. The fee levels reflect the expectation that you will support recovery at/return to work and provide optimal services in this pursuit.
The fees set by SIRA are the maximum amount that can be paid for a service. This amount is legally binding and cannot be billed at higher rates.
Under Part 5 of the Guidelines for the Provision of Relevant Services (Health and Related Services) medical practitioners must not:
- request pre-payment of fees for reports and services from the insurer
- directly bill relevant services to an injured worker who has already lodged a claim
- bill an amount that is above the maximum amount fixed in the SIRA fees order
- charge the injured person any additional or gap fee
- charge a fee for cancellation or non-attendance by an injured worker for treatment services.
For payment of medical consultations and services, the AMA item codes must be used. Additionally, there are codes for SIRA-specific services that are not found in the AMA List. These are available on our current health related fees page.
Invoicing
Part 6 of the Guidelines for the Provision of Relevant Services (Health and Related Services) requires that medical practitioners must provide itemised invoices before payment can be made by the insurer; and that invoices must be submitted within 30 calendar days and include the following:
- the injured worker’s first and last name, and claim number
- payee name, address, telephone number and email address
- payee Australian Business Number (ABN)
- name of the relevant service provider who delivered the relevant service
- in the case of medical practitioner services, the provider’s:
- Australian Health Practitioner Regulation Agency (AHPRA) number, and
- Medicare provider number (unless not registered with Medicare).
- in the case of invoices for surgery:
- a detailed operation report including a description of the initial injury and an outline of the mechanism of injury, time surgery commenced and finished, intra-operative findings and the procedures performed, including structures that were repaired (stating the anatomic location) and technique of repair.
- relevant SIRA payment classification code or Australian Medical Association (AMA) Fees List item number (where applicable)
- service cost for each SIRA payment classification code or AMA Fees List item number and service duration (if applicable)
- date of service
- date of invoice (must be on the day of or after last date of service listed on the invoice).
Payment complaints
Payments by insurers are to be made within a reasonable timeframe upon receipt of a correctly completed invoice where liability has been accepted.
If you have a complaint about the payment of your account, contact the insurer case manager responsible for payment. If you are unable to resolve the issue with the case manager, you should escalate the matter to their supervisor or the insurer's complaints department.
If after contacting the insurer you have not been able to resolve the matter, you should contact our Customer Service Centre on 13 74 72. We will ask you to provide evidence of your attempts to address the problem with the insurer.
Approval for services
In general, approval from the insurer is required prior to the provision of medical and treatment related services.
However, workers can access some services as a result of the work related injury without pre-approval from the insurer. Below is a list of those services relevant to medical practitioners. For a full list of reasonably necessary treatments and services that do not require pre-approval from the insurer, refer to page 13 of the workers compensation guidelines.
Any treatment within 48 hours of the injury happening.
Any consultation or case conferencing for the injury, apart from telehealth and home visits.
Any treatment during consultation for the injury, within one month of the date of the injury.
If referred by the nominated treating doctor, any consultation and treatment during consultations for the injury (apart from telehealth) within three months of the injury.
Prescription and over-the-counter pharmacy items prescribed by the nominated treating doctor or medical specialist for the injury and dispensed:
- within one month of the date of injury, or
- after one month of the date of injury if prescribed through the Pharmaceutical Benefits Scheme.
If referred by the nominated treating doctor for the injury:
- any plain x-rays within two weeks of the date of injury
- ultrasounds, CT scans or MRIs within three months of the date of injury, where the worker has been referred to a medical specialist for further injury management.
On referral by the medical specialist for the injury, any diagnostic investigations within three months of the date of injury.
Note: A general practitioner's MRI referral must meet Medicare Benefits Schedule criteria.
Any services provided in the emergency department for the injury.
Any services after receiving treatment at the emergency department for the injury, within one month of the date of injury.
The initial hearing needs assessment where:
- the hearing service provider is approved by SIRA, and
- the nominated treating doctor has referred the worker to a medical specialist who is an ear, nose and throat doctor, to assess if the hearing loss is work related and the percentage of binaural hearing loss.
Note: Hearing needs assessment includes obtaining a clinical history, hearing assessment as per Australian/New Zealand Standard 1269.4:2005, the determination of communication goals, recommendation of hearing aid and clinical rationale for hearing aid.
Further information
If you have any issues or queries regarding the worker's compensation claim:
- Contact the insurer. The insurer is the first point of contact for further information about the worker's claim and recovery at work.
- Contact our Customer Service Centre on 13 74 72 or visit our website for general information about work health and safety and workers compensation, or email contact@sira.nsw.gov.au.
If a worker is having issues with an insurer and they have been unable to resolve the matter directly, suggest they contact the Independent Review Office (IRO). IRO provides an independent complaints resolution service for worker and insurer disputes. Call 13 94 76 or visit their website for more information.
- The Australasian consensus statement on the health benefits of work and the role of GPs in realising the health benefits of work by the Australasian Faculty of Occupational and Environmental Medicine and the Royal Australasian College of Physicians.
- The Principles on the Role of General Practitioners in Supporting Work Participation assist GPs, other relevant professionals, and stakeholders to work better together to ensure no Australians are disadvantaged due to a health condition or disability that may impact their ability to work. There is a snapshot version and a full version.
- Talking about a return to work - conversation starters is a useful guide for general practitioners created by the Australasian Faculty of Occupational and Environmental Medicine and the Royal Australian College of General Practitioners.
- Returning to Work After an Injury provides guiding principles for General Practitioners completing the initial assessment early treatment phase of injury with a primary focus on the rehabilitation and return to work process.
References
- Cheng and Hung. Randomized Controlled Trial of Workplace- based Rehabilitation for Work-related Rotator Cuff Disorder. J Occup Rehab (2007) 17:487-503.
- Waddell G, Burton AK. Is work good for your health and wellbeing? London: The Stationery Office. 2006.
- Australian Consensus Statement on the Health Benefits of Work. A Position Statement. Australasian Faculty of Occupational and Environmental Medicine and The Royal Australasian College of Physicians. 2011.
- Johnson D, Fry T. Factors Affecting Return to Work after Injury: A study for the Victorian SIRA Authority. Melbourne: Melbourne Institute of Applied Economic and Social Research; 2002.
- Waddell G, Burton AK. Is work good for your health and wellbeing? London: The Stationery Office. 2006.
- Waddell G, Burton AK. Is work good for your health and wellbeing? London: The Stationery Office. 2006.
- Waddell G, Burton AK. Is work good for your health and wellbeing? London: The Stationery Office. 2006.
- Foreman P, Murphy G and Swerissen H. Barriers and facilitators to return to work: A Literature Review. Melbourne: Australian Institute for Primary Care, La Trobe University 2006.
Updated 21 July 2025