Model of care for the management of low back pain
The Model of care for the management of low back pain - summary (the Summary Model) champions best practice and is a guide for health practitioners and insurers managing claims under the motor accidents (CTP) and workers compensation (WC) schemes in NSW.
The Summary Model is an up to date, evidence-informed guide for primary care clinicians on best practice management of back pain. It encourages self-management, return to work and usual activity, empowering the person in their recovery journey.
The Summary Model promotes a holistic and person-centered approach through standardised risk evaluation of all injured people with lower back pain.
The Summary Model recommends that people use work as part of their recovery, and by talking to their doctor and employer about what they can do at work to help them stay active and recover.
How was the Summary Model developed?
The State Insurance Regulatory Authority (SIRA) developed the Summary Model in partnership with the NSW Agency for Clinical Innovation (ACI) as a value-based healthcare initiative to support enhanced clinical practice across the CTP and WC schemes. The Summary Model is based on the existing ACI Management of people with acute low back pain model of care.
SIRA brought together its Back Injury Clinical Advisory Group, the ACI and its expert groups to review the existing model and create the Model of care for the management of low back pain - Summary (the Summary Model). The revision includes current evidence and promotes consistency of care and prevention of low-value care for all people experiencing back pain, whether their back pain is compensable or not.
Members of the Clinical Advisory Group and the representatives are listed below.
Members of the Back Injury Clinical Advisory Group
Organisation | Member |
|---|---|
Australian Medical Association | Dr Rodney Allen |
Australian Orthopaedic Association | Dr Nathan Hartin |
Specialist Musculoskeletal Physiotherapist | Dr Michael Ryan |
Institute for Musculoskeletal Health, Sydney School of Public Health, Faculty of Medicine and Health The University of Sydney | Professor Chris Maher |
Ingham Institute | Professor Ian Harris |
The University of Sydney, Pain Management Research Institute Faculty of Medicine and Health | Professor Michael Nicholas |
Neurosurgical Society Australia | Dr Mitchell Hansen |
The Royal Australasian College of Surgeons NSW Branch | Dr Gemma Olsson |
Faculty of Pain Medicine, Australian and New Zealand College of Anaesthetists | Dr Renata Bazina |
Surgery Advisory Panel, WorkSafe Victoria | Dr Susan Liew |
Agency for Clinical Innovation (ACI) | Ms Jenni Johnson |
Transport Accident Commission | Dr Hugh Seward |
The Royal Australian College of General Practitioners | Dr Steve Peterson |
The Summary Model will support people to receive value-based healthcare through the early assessment, management, review and appropriate referral of people with back injury in the NSW personal injury schemes.
Watch the video below for more information about the initiative.
Why is SIRA introducing this model of care?
People with low back pain have been identified as a priority group in SIRA’s implementation of value-based healthcare.
Recent SIRA funded research found suboptimal outcomes for people with low back pain in the WC scheme who receive surgery, including:
- High cost of surgery with an average cost for a surgical episode of $46,000 for spinal fusion and $20,000 for spinal decompression.
- High rates of additional surgery with 1 in 5 people receiving at least one reoperation within 2 years.
- Low return to work rates with only 19% of spinal fusions and 39% of spinal decompression patients returning to work in full capacity within 2 years.
Standardised outcome measures for back pain
SIRA has published a set of standardised outcome measures for healthcare providers to screen an injured person’s health status, and to support evidence-based decision-making and care planning.
- The Örebro Musculoskeletal Pain Screening Questionnaire (short-form) is a ‘yellow flag’ screening tool that predicts long-term disability and failure to return to work.
- The Keele STarT Back screening tool helps primary care match patients to treatment appropriate for them.
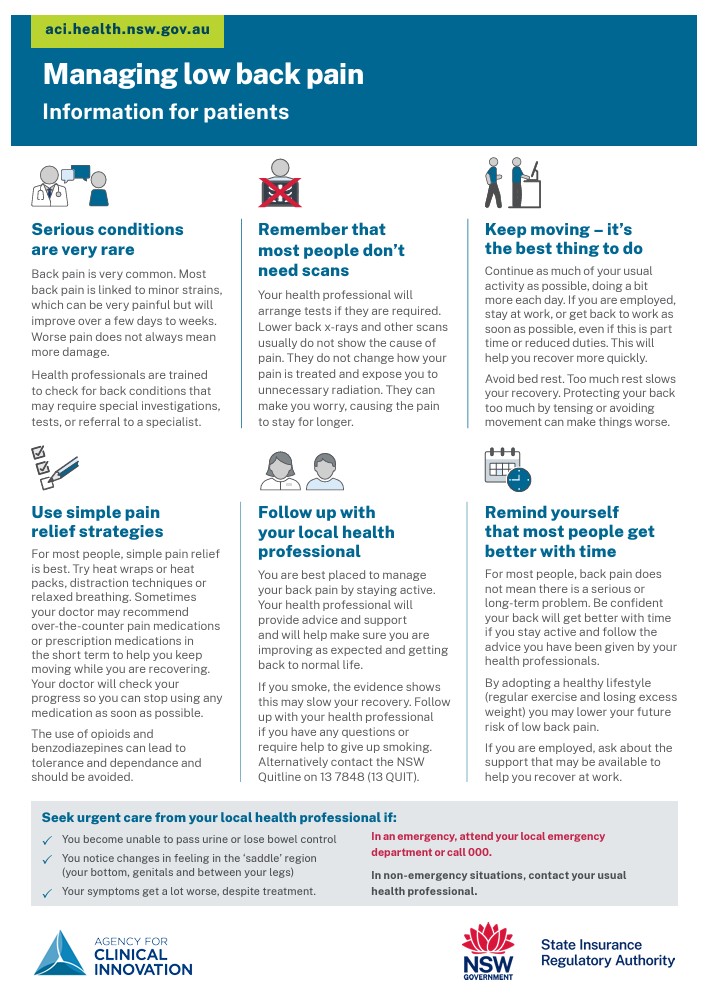
Managing low back pain - information for patients
Frequently asked questions
For answers to frequently asked questions about the model of care, please see the fact sheets available to download or specific questions below.
What is a model of care?
A 'model of care' broadly defines the way health services are delivered. It outlines best practice care and services for a person as they progress through the stages of a condition, injury or event.
Who is the model of care for the management of low back pain for?
The model is for:
- people with low back pain in NSW, and
- guiding health professionals to provide healthcare that helps people with low back pain to recover.
Why was the model developed?
People with low back pain have been identified as a priority group in SIRA’s implementation of value-based healthcare.
Recent SIRA funded research has found sub optimal outcomes for people with low back pain in WC scheme who receive surgery, including:
- low return to work rates
- high rates of additional surgery
- an ongoing need for pain medicine at two years post-surgery
- and high cost of treatment.
The model is a value-based healthcare initiative that will enable SIRA to support enhanced clinical practice across CTP and WC schemes.
Value-based healthcare is defined as achieving measurable improvements in a patient’s meaningful health outcomes relative to the resources utilised in achieving those improvements.
The model will support people to receive value-based healthcare through the early assessment, management, review and appropriate referral of people with back injury in the NSW personal injury schemes.
What are an employer's responsibilities?
Responsibilities of an employer include:
- providing workers with the Managing low back pain: Information for patients fact sheet,
- arranging a case conference for complex cases to set goals, ensure roles and responsibilities are understood and agree on timeframes to recover at or return to work,
- participation in the development and implementation of the worker’s injury management plan, written by the insurer,
- providing suitable work that is (as far as reasonably practicable) the same as or equivalent to the work being performed at the time of the injury.
More information is available in When a worker is injured: A workers compensation guide for employers.
What does this mean for insurers?
Insurers should expect that people in the CTP & WC schemes receive care according to these pathways, including:
- biopsychosocial risk screening at regular intervals to ensure a holistic and person-centred approach,
- primary care providers using the Standardised outcome measures to determine what pathway is relevant,
- people in pathway A or C who show no improvement by visit 3 (6 week) should be referred by their GP to a musculoskeletal specialist,
- people presenting to primary care with suspected conditions of concern identified in the pathways should have immediate referral to a tertiary hospital or other specialist care.
Does the model direct or limit the services people in the schemes are able to receive?
The model champions best practices and is a guide for practitioners caring for people with low back pain. The model uses 10 key principles to promote best practice for people with low back pain.
Insurers are not required to instruct or direct primary health care providers on how to treat an injured person, or direct a general practitioner to make a referral in accordance with the medical pathways. However, insurers can encourage general practitioners and primary healthcare practitioners to adopt the model.
The primary care practitioner is guided through the model so that people are triaged appropriately and referrals to musculoskeletal specialists or other specialist care is made in line with the model.
What are the benefits of recovering at work?
Being at work is often the best way to recover from your injury.
Research suggests five key benefits:
- Get better sooner - recovering at work with support from your employer means you’re likely to get better sooner.
- Keep up your connections - recovering at work helps you stay connected with colleagues and workplace friends.
- Get back to your usual activities - recovering at work also helps you return to the other things you enjoy.
- Boost your physical and mental health - recovering at work can boost your self esteem and wellbeing according to research.
- Reduce the chance of long-term effects - recovering at work helps you avoid other health complications following injury.
Additional resources
- SIRA standardised outcome measures
- SIRA implementation plan for value-based healthcare in the NSW WC and CTP schemes
- Agency for Clinical Innovation Management of people with acute low back pain (the full model of care)
- Summary model factsheet
Contact
Contact SIRA's Value Based Healthcare team by email at [email protected].