Foreword
A fundamental objective of the State Insurance Regulatory Authority (SIRA) is to ensure that people who make claims in workers compensation and compulsory third party (CTP) schemes achieve good outcomes from the healthcare they receive - every dollar spent should deliver quality, value, and optimise recovery.
The Implementation plan for value-based healthcare in NSW WC and CTP schemes will drive improved health outcomes across the sector. SIRA will work collaboratively with all key participants of the workers compensation and CTP schemes to achieve this.
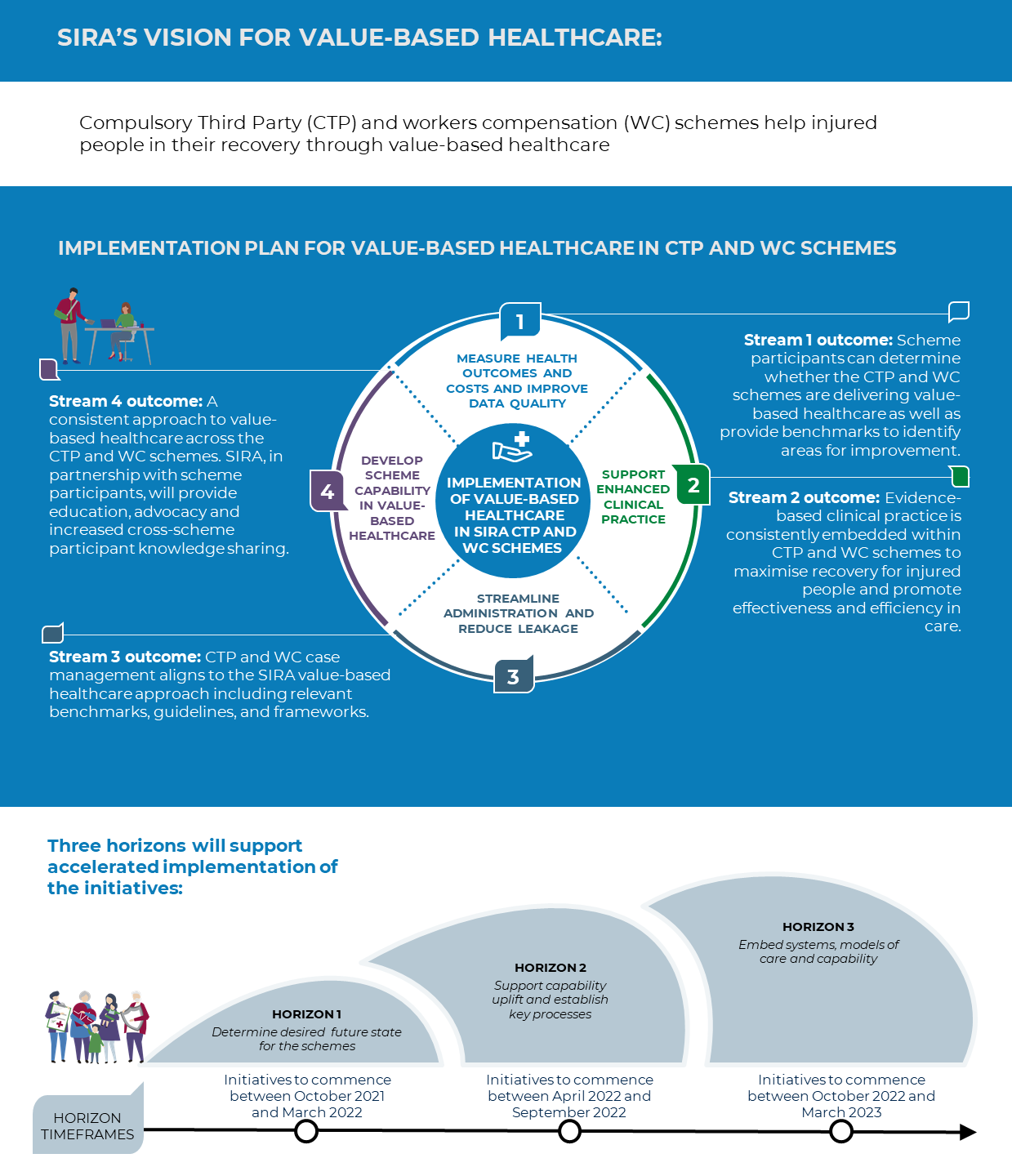
In 2020, SIRA committed to the vision
Compulsory Third Party (CTP) and workers compensation (WC) schemes help injured people in their recovery through value-based healthcare.
Achieving this will require innovation and collaboration. This is an ambitious plan, and as far as we know, the first time a value-based healthcare approach has been introduced in a compensable context. We have consulted with people with lived experience of the schemes and those who work in the schemes, who have advised us on how best to achieve this vision of getting the best possible health outcomes and experiences for people who are injured.
We know that there is room for improvement in WC and CTP schemes in the timeliness and way decisions are made about injured people’s care, how resources are used, and how we determine we are getting the best value in terms of outcomes.
We will continue to involve all scheme participants in developing and implementing all 21 initiatives in this plan. Some of the most significant initiatives in the plan include:
- designing how data on the health outcomes of injured people in the WC and CTP schemes will start to be collected
- developing best practice models of treatment and healthcare for key injuries seen in WC and CTP
- re-imagining administrative processes involving clinicians, insurers and injured people to reduce delays and duplication of effort
- identification and implementation of measures to empower injured people through improved health literacy.
I would like to acknowledge and thank all the scheme participants who have come together to guide the development of this plan - the people with lived experience of the schemes, representatives of insurers, road users, employers, unions, health practitioners and their peak organisations.
Adam Dent
Chief Executive
December 2021
| Term | Definition |
|---|
| Allied health practitioners | Covers a broad range of health professionals who are not doctors, dentists, nurses or midwives. They include practitioners such as physiotherapists, psychologists, exercise physiologists, amongst others. |
| Clinicians | Medical practitioners, treating specialists and/or allied health practitioners operating in the CTP and WC schemes. |
| CTP | NSW Compulsory Third Party scheme |
| GPs | General practitioners – often the nominated treating doctor for an injured person. |
| Health outcomes framework | SIRA’s Value-Based Healthcare Outcomes Framework |
| Health providers | Any health service provider operating in the CTP and WC schemes. This includes individual practitioners and organisations that provide healthcare, such as hospitals. |
| Injured people | Any injured person accessing the CTP or WC schemes. |
| Lived experience | Injured people who have experience of healthcare provided through the CTP and WC schemes. |
| Multi-disciplinary teams | A team of health professionals, from one or more clinical backgrounds, working together to deliver comprehensive patient care. |
| Scheme participants | Persons and organisations that engage in the CTP and WC schemes including injured people, insurers, clinicians and health providers. |
| SIRA | State Insurance Regulatory Authority. |
| Value-based healthcare | An approach to healthcare that centres the needs of the injured person through directing resources to areas where they will achieve the greatest health outcomes. |
| WC | NSW workers compensation scheme. |
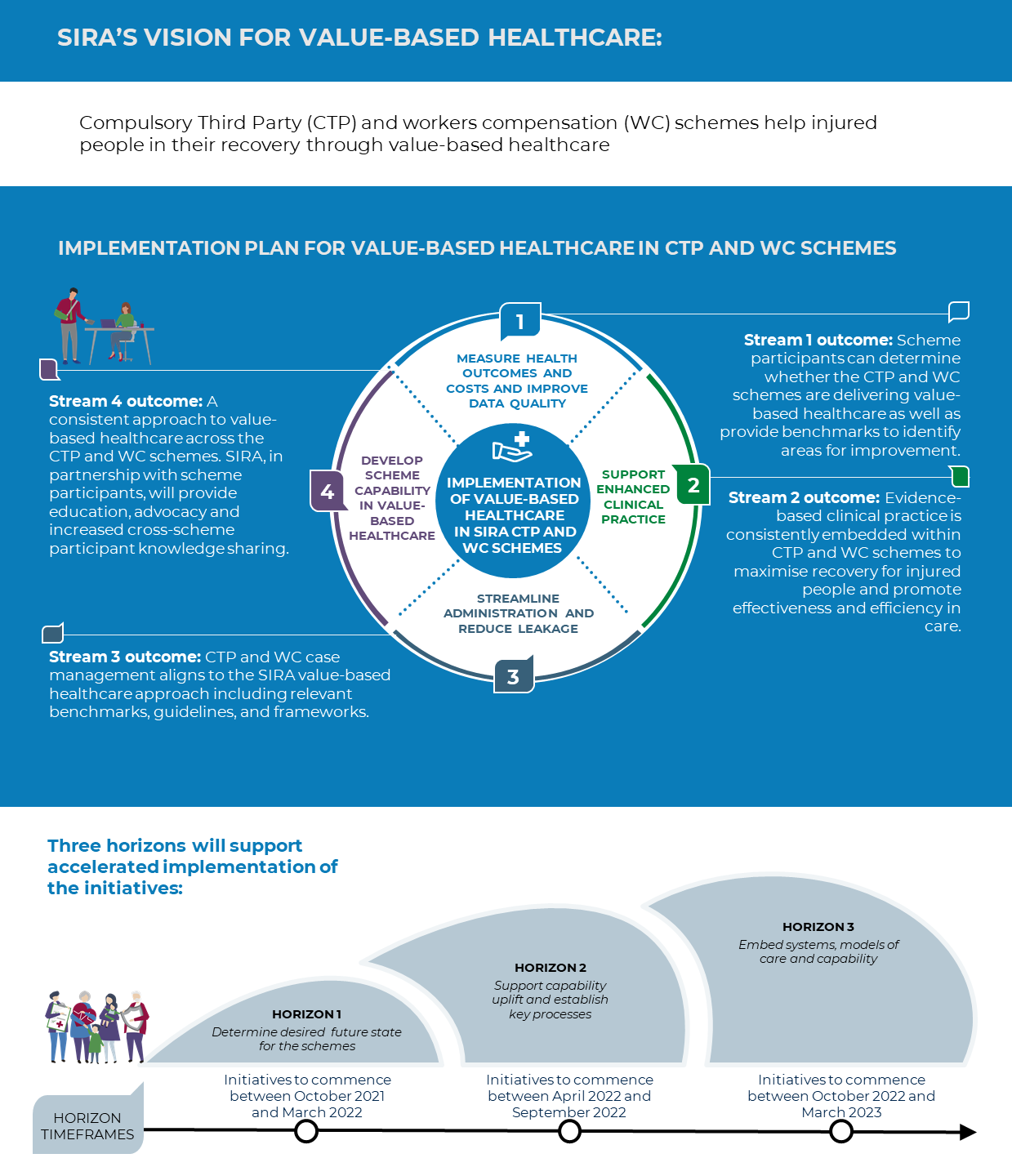
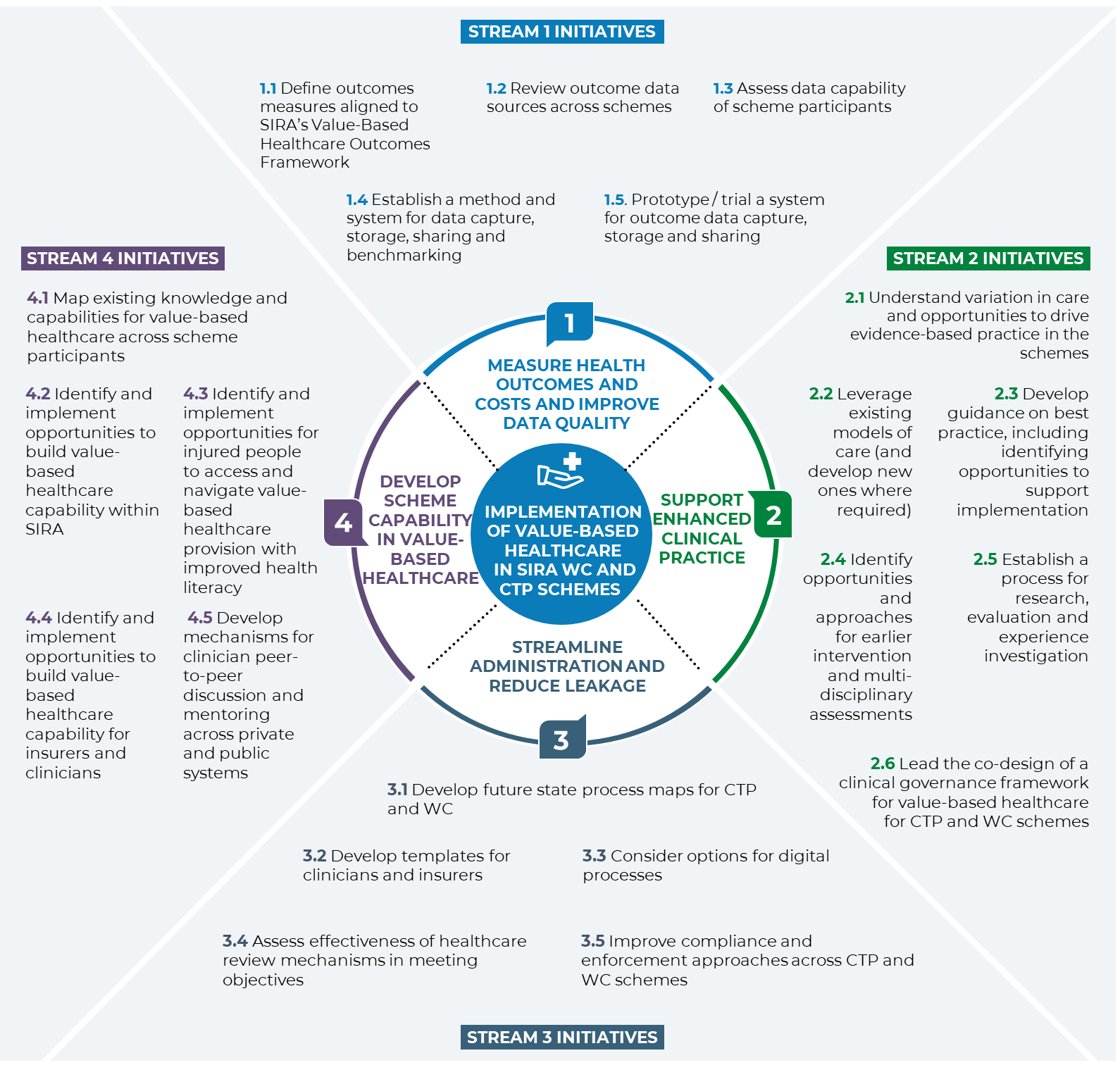
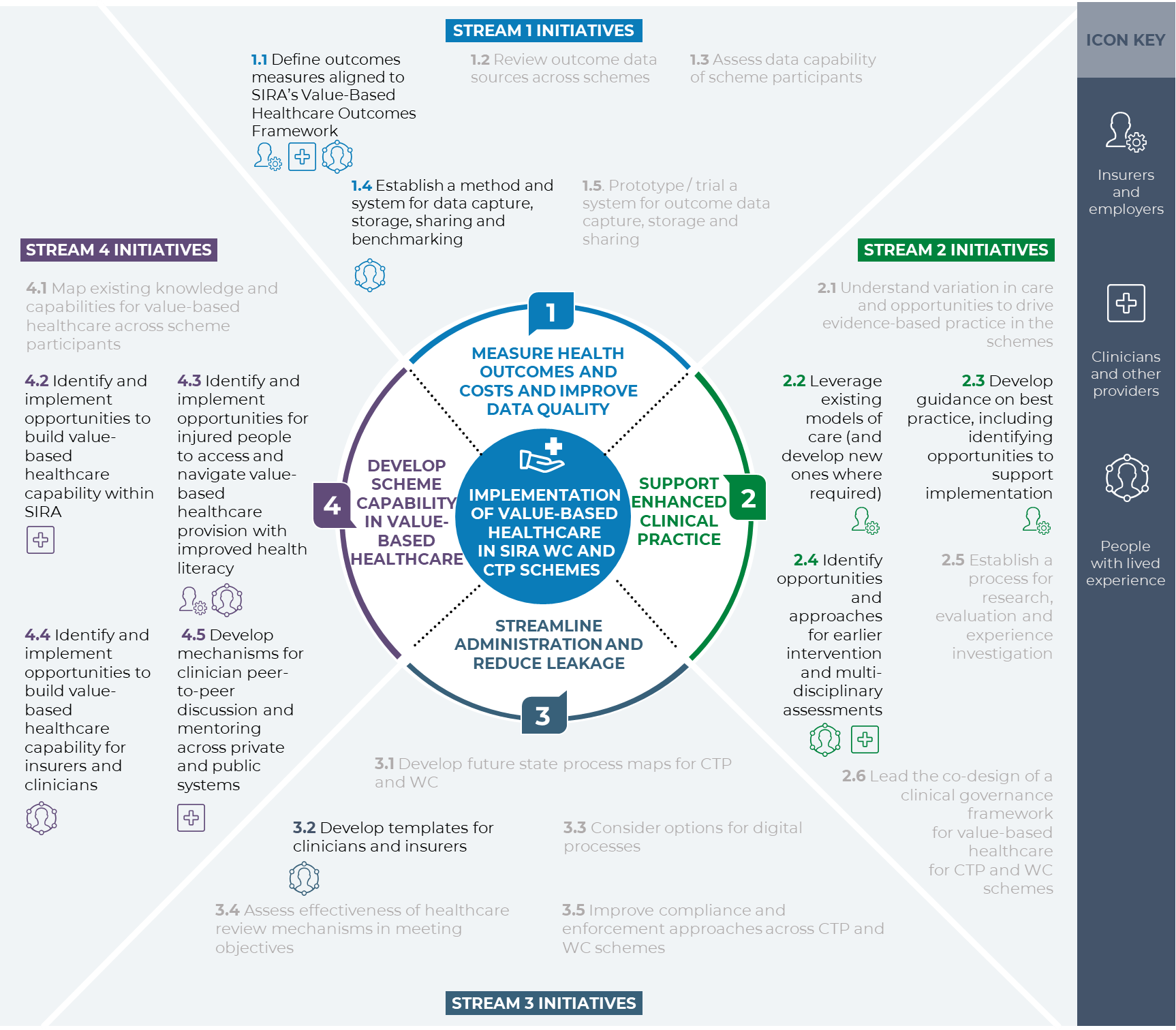
Figure 1: Implementation Plan for value-based healthcare in CTP and WC schemes.
1. Executive summary
The State Insurance Regulatory Authority (SIRA)’s vision for healthcare is that “Compulsory Third Party and workers compensation schemes help injured people in their recovery through value-based healthcare”. Value-based healthcare is defined as achieving measurable improvements in a patient’s meaningful health outcomes relative to the resources utilised in achieving those improvements. With a value-based healthcare approach, SIRA will support recovery and improve return to activity, return to work and quality of life outcomes for people injured at work and on the road.
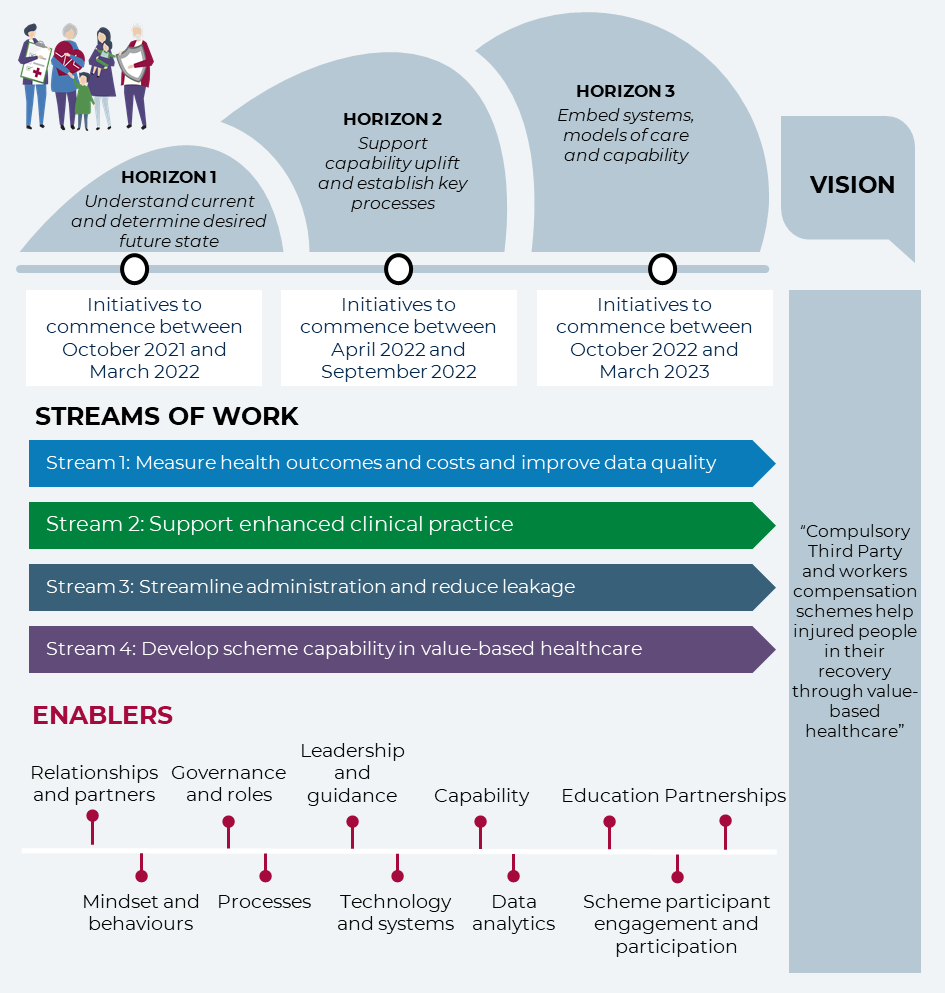
SIRA is implementing 21 initiatives across four streams of work that will drive the uptake of value-based healthcare. These initiatives are outlined in the following implementation plan (this document). This implementation plan was developed through a co-design process with stakeholders including people with lived experience, clinicians, employers, unions, and insurers – and their representatives.
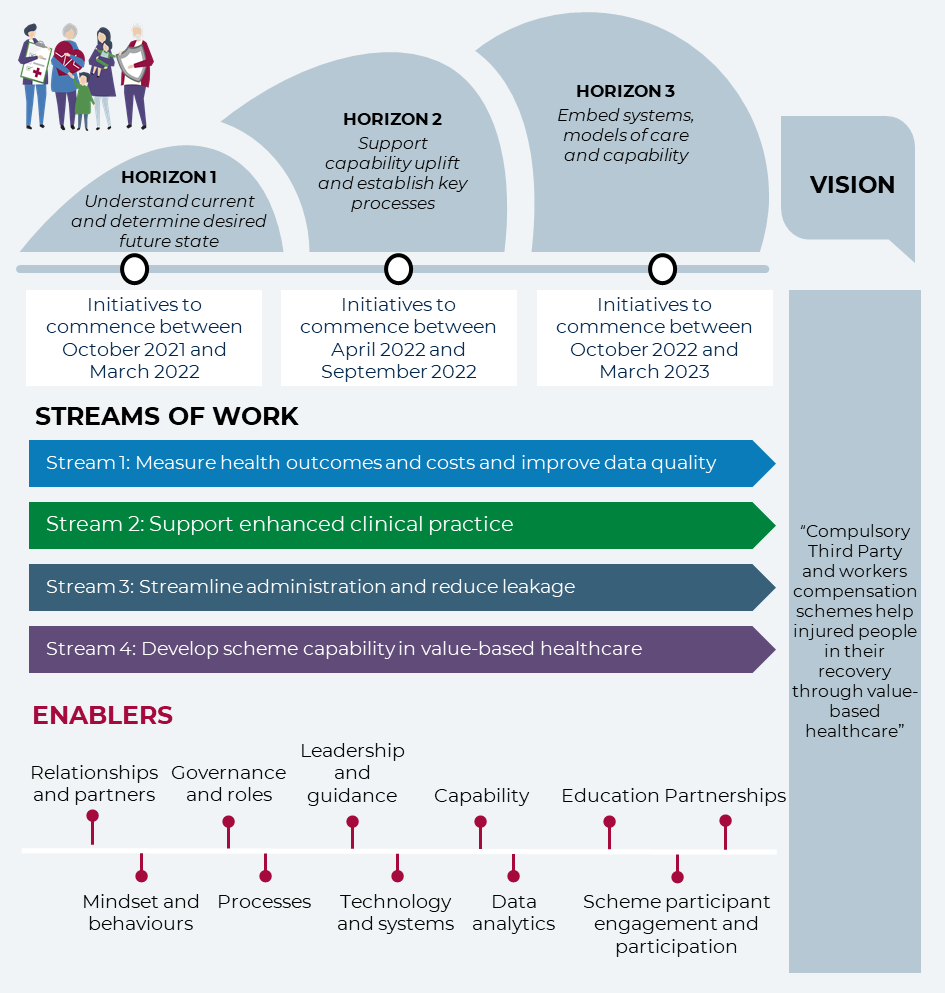
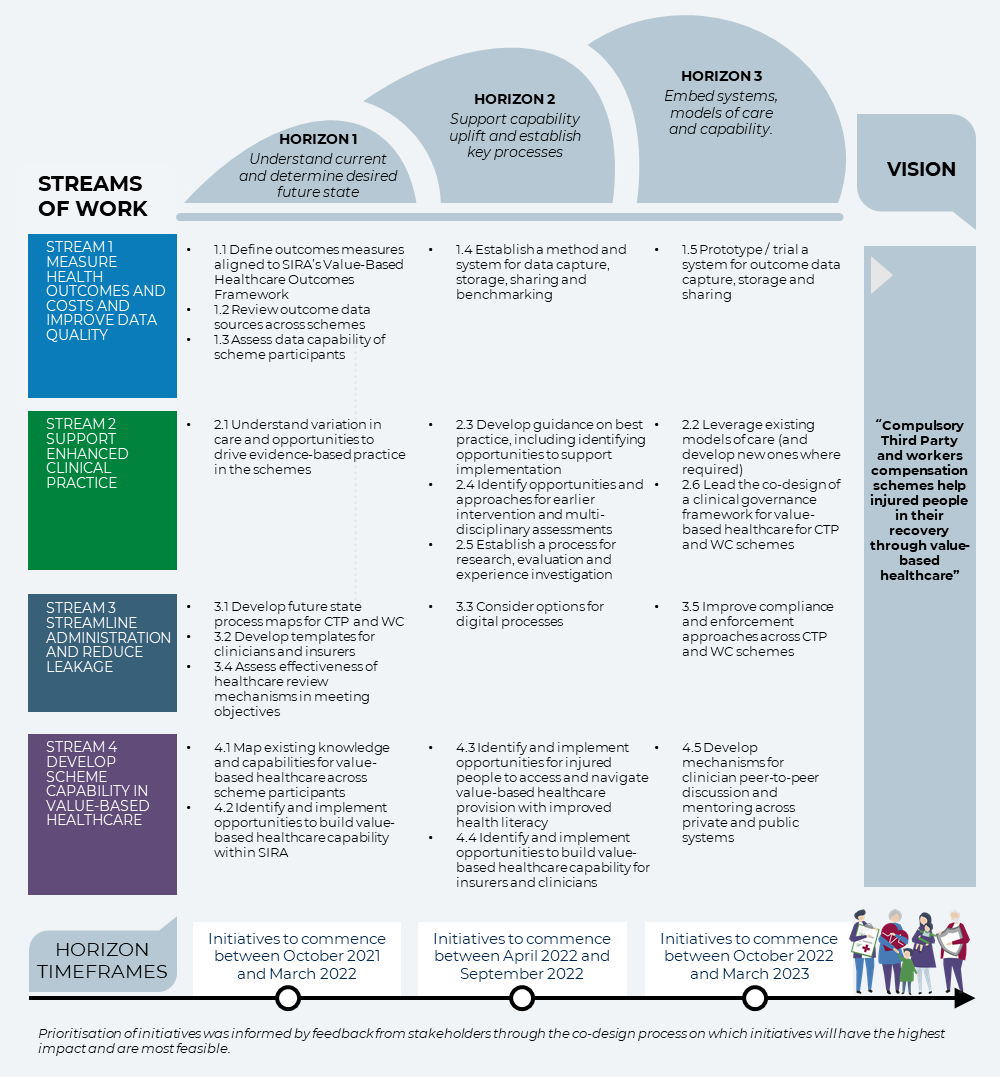
Figure 2 SIRA’s approach to implementation
Implementation will occur across three time horizons commencing between October 2021 and March 2023. SIRA has already started work on understanding the current state and the desired future state before it moves to supporting capability uplift and establishing key processes. Finally, SIRA will focus on embedding systems, models of care and capability. Through the implementation of this ambitious implementation plan (this document), SIRA will be world leading in its application of value-based healthcare to compensation schemes. The horizons for implementation are outlined in Figure 2, above.
2. Introduction
2.1. Purpose of the implementation plan
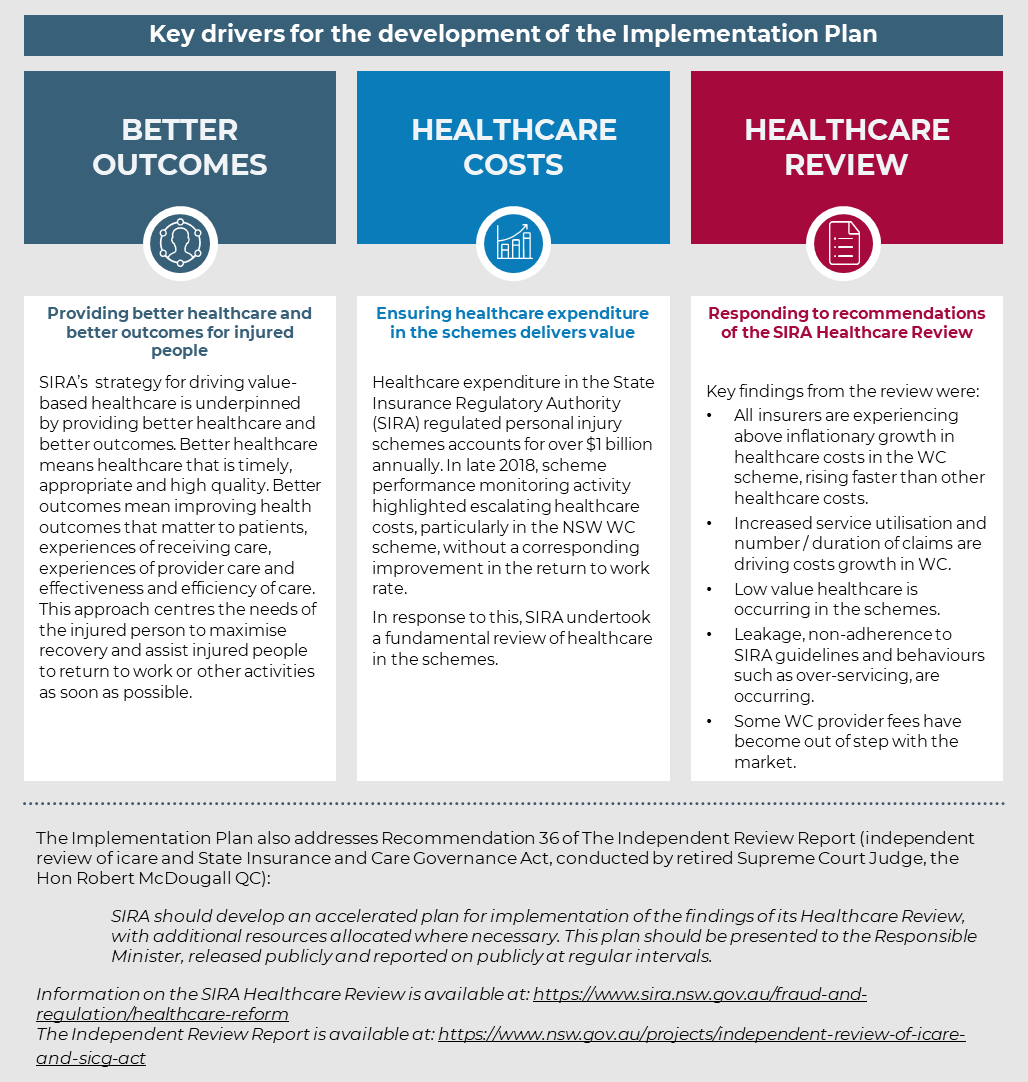
SIRA regulates the CTP and WC statutory insurance schemes in NSW and is committed to achieving value-based healthcare in these schemes. SIRA’s role is to ensure that the schemes that it regulates continue to be fair, effective, and affordable for policy holders, and for people who make a claim for compensation today or in the future.
The purpose of this implementation plan is to support SIRA to implement value-based healthcare in NSW CTP and WC schemes and respond to the findings of the SIRA Healthcare Review. Through the implementation of the initiatives, SIRA will be a world leader in the application of value-based healthcare to compensation schemes. The key drivers for the development of the implementation plan are outlined in Figure 3, below.
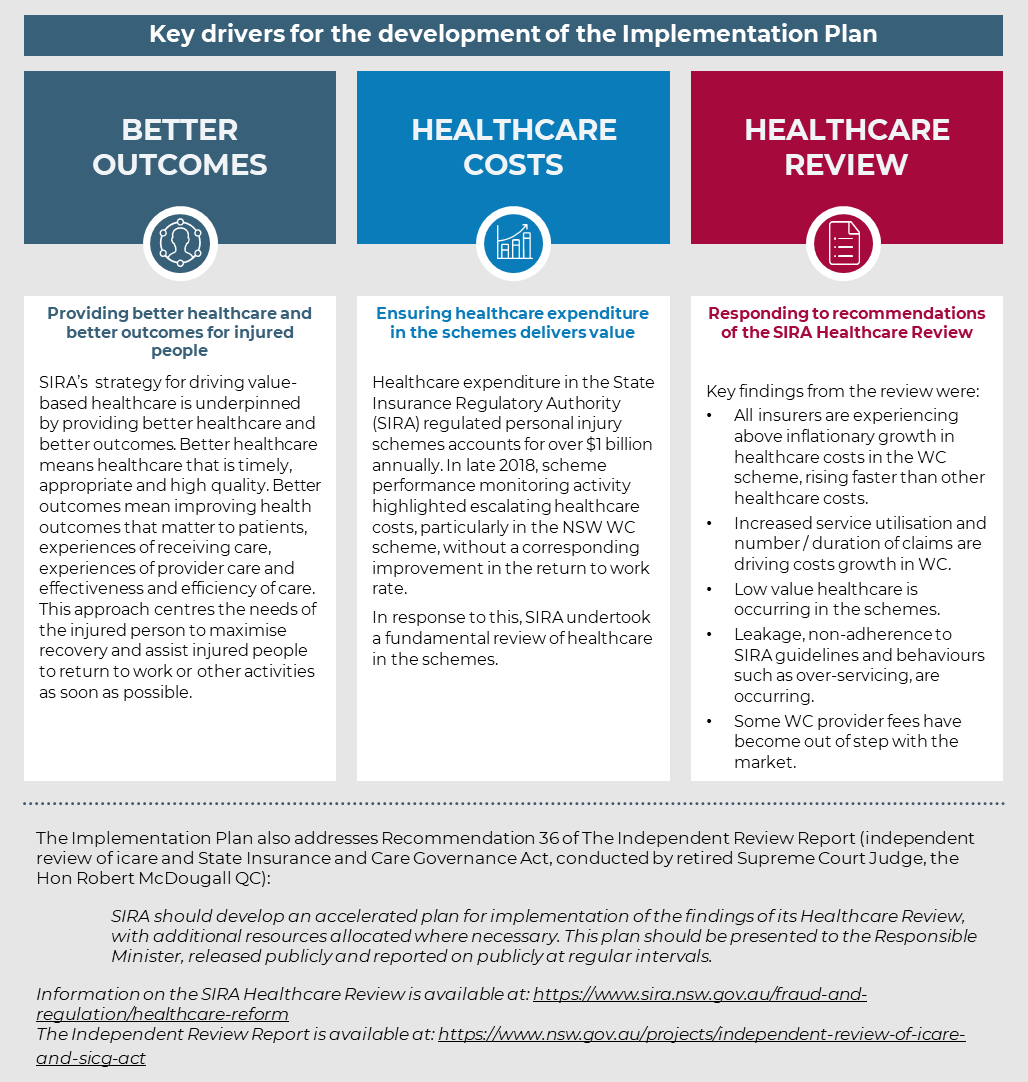
Figure 3 Key drivers for the development of the implementation plan
2.2. Value-based healthcare and SIRA
SIRA has adopted the quadruple aim that continually strives to deliver care that improves:
- health outcomes that matter to patients
- experiences of receiving care
- experiences of provider care
- effectiveness and efficiency of care
Value-based healthcare in CTP and WC schemes will allow SIRA to deliver on the quadruple aim. This will help to support recovery and improve return to activity, return to work and quality of life outcomes for people injured at work and on the road by providing the right care, at the right time, in the right setting.
As shown in Figure 4 below, value is measured by looking at the health outcomes of injured people in the schemes relative to the resources used. Value-based healthcare effectively directs resources to areas where they will achieve the greatest health outcomes.

Figure 4: Overview of value-based healthcare1
Since the concept originated around 15 years ago, value-based healthcare has been increasingly recognised as essential to delivering sustainable healthcare. Governments and organisations across NSW, Australia and the world are working towards value-based healthcare arrangements. With most health systems set up to focus on delivery and costs, moving health systems towards value-based healthcare necessitates significant reforms.
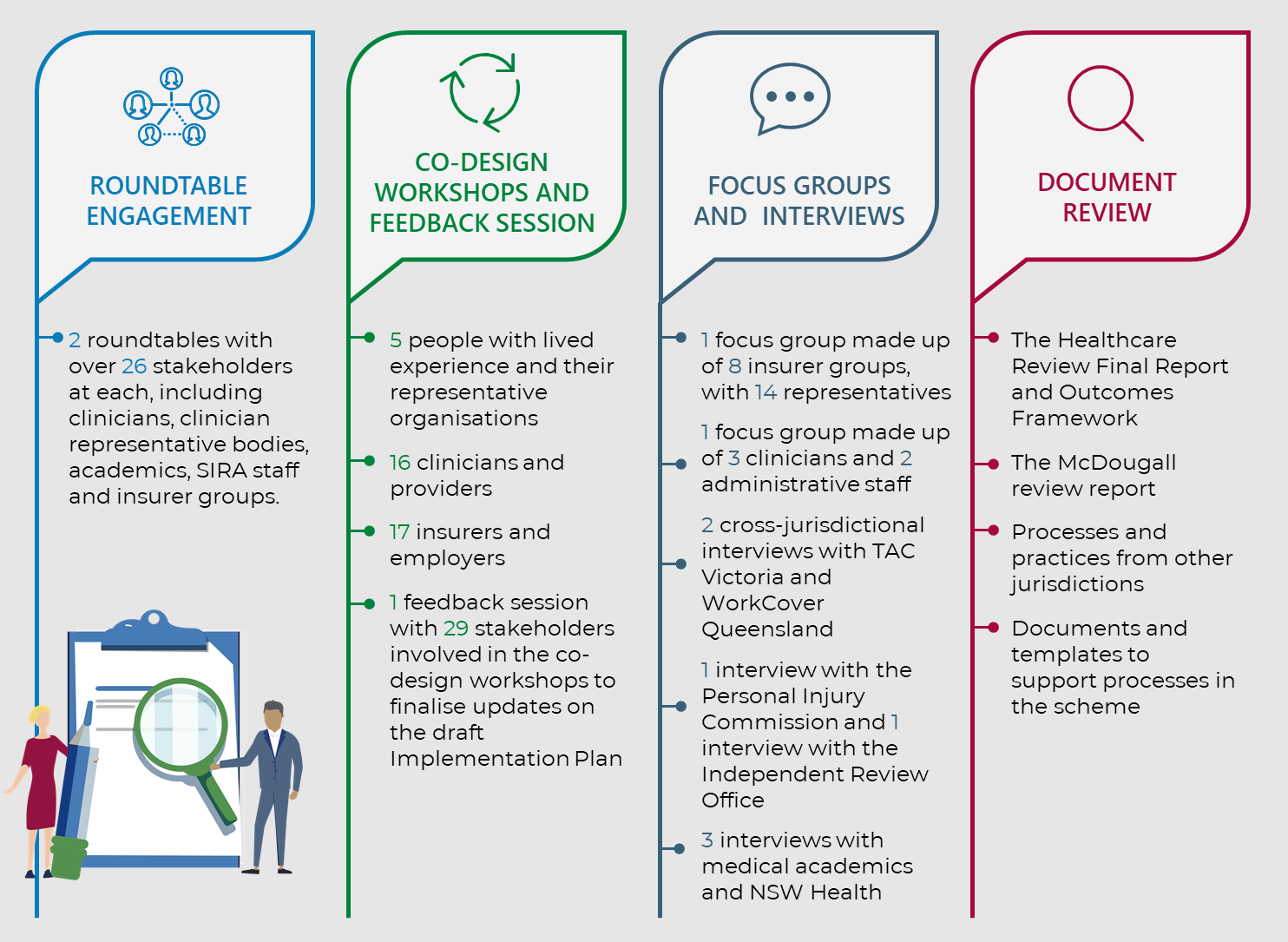
2.3. How we developed our implementation plan
SIRA, with the support of Nous Group (Nous), undertook several activities to ensure that the methodology to develop the implementation plan included co-design with stakeholders, considered existing knowledge and data, and communicated with staff and stakeholders throughout the process. This means that over 80 key stakeholders were involved in shaping the implementation plan, including participating in a prioritisation process to identify which initiatives will have the highest impact and are most feasible. A list of those organisations and people involved can be found in Appendix C.
The implementation plan has been informed by the activities outlined in Figure 5.
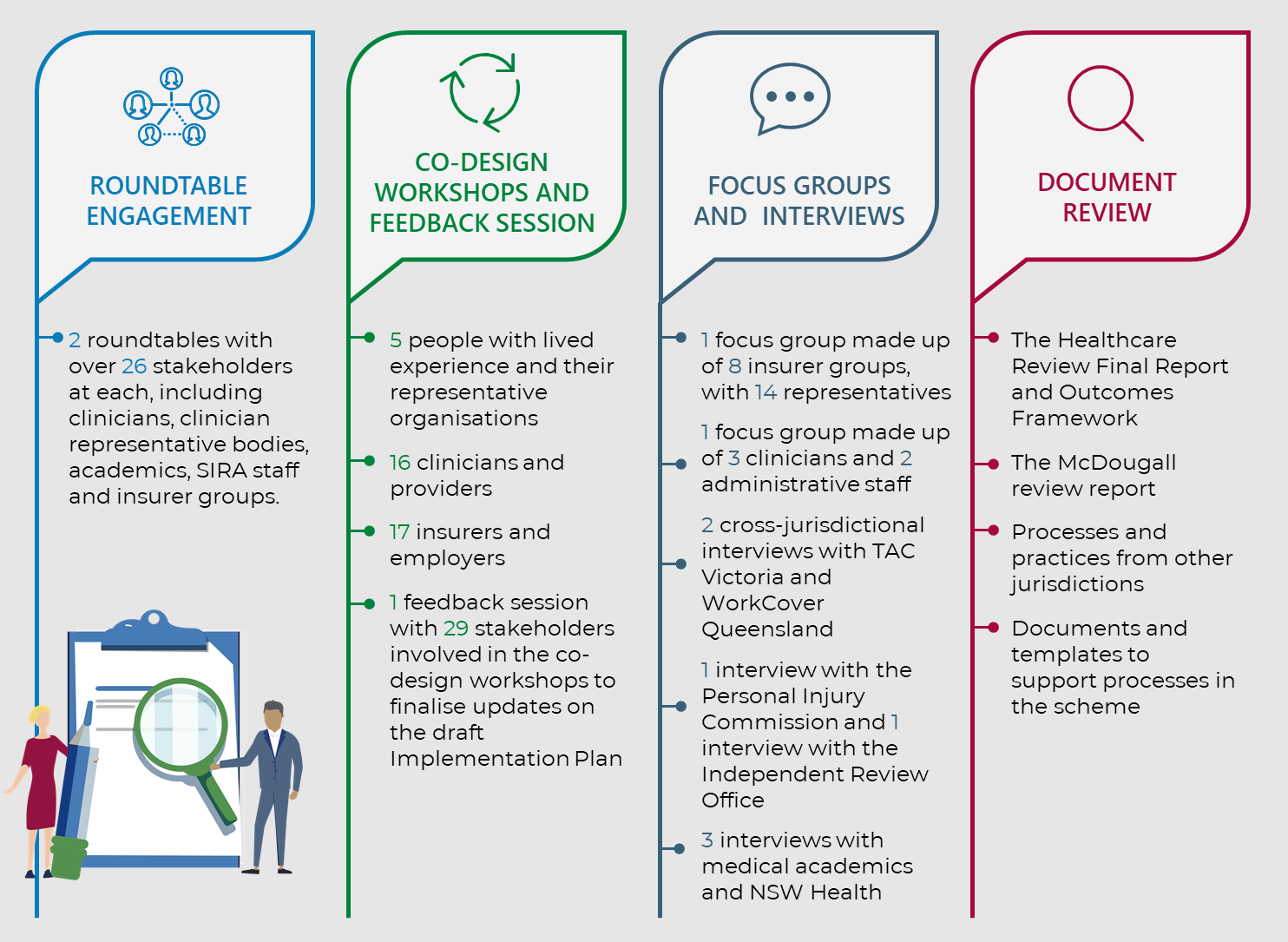
Figure 5: Development of the implementation plan
3. Streams of work
This section outlines four streams of work for the implementation plan. There are five to six initiatives per stream. Each initiative includes:
- a rationale based on outcomes SIRA is looking to deliver for the CTP and WC schemes
- actions listed sequentially to support implementation of the initiatives.
Additional information on implementation is outlined in Section 5. A summary of the four streams of work and the related initiatives is provided in Figure 6, below.
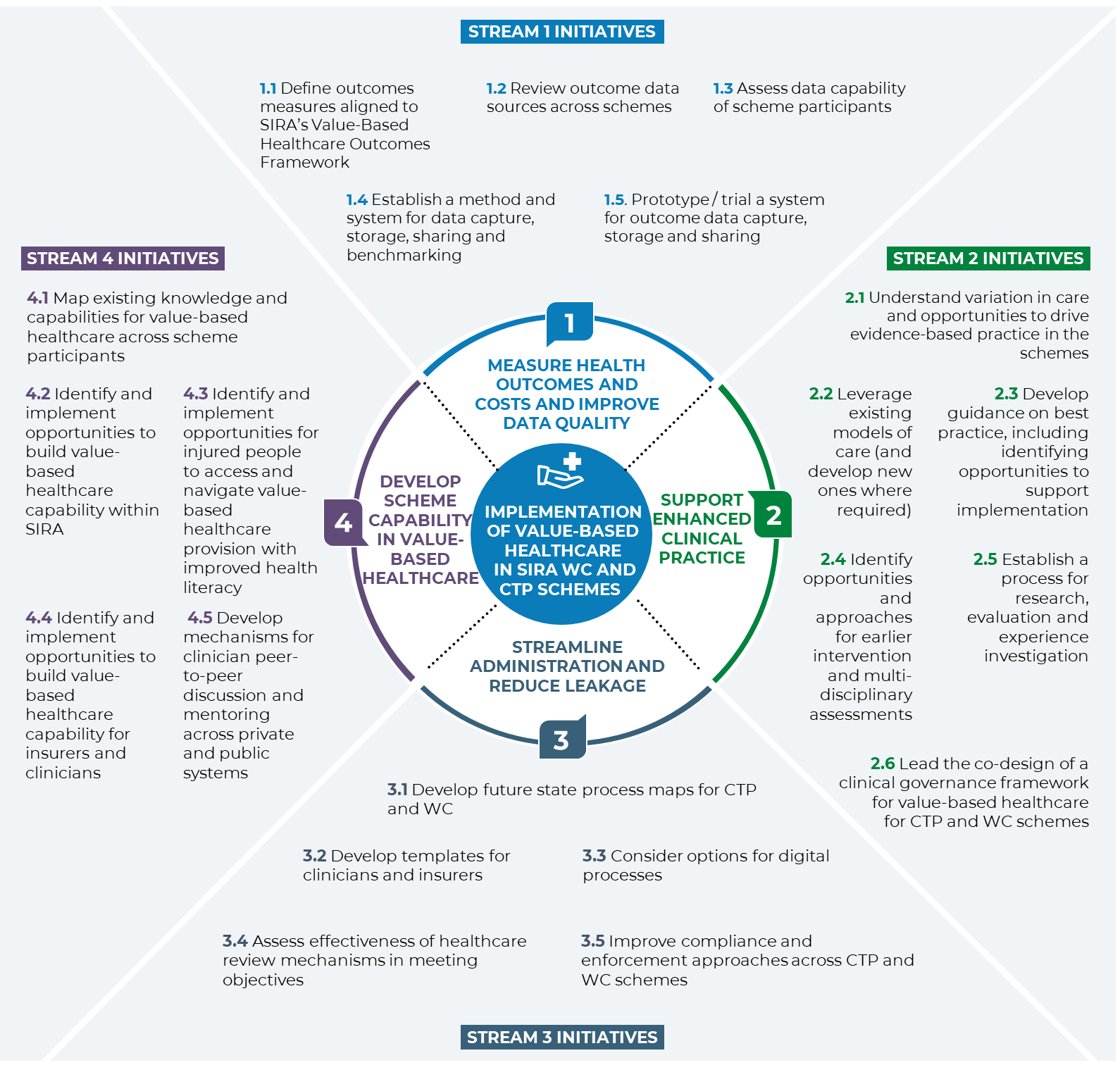
Figure 6: Summary of streams of work
Stream 1: Measure health outcomes and costs and improve data quality
Stream 1 will ensure SIRA and scheme participants can determine whether the CTP and WC schemes are delivering value-based healthcare as well as provide benchmarks to identify areas for improvement. This stream will support the implementation of SIRA’s health outcomes framework through:
- Clearly defining outcome measures. This includes Patient-Reported Outcome Measures (PROMs) and Patient Reported Experience Measures (PREMs).
- Embedding consistent approaches to the measurement of health outcomes, including patient and clinician experience measures, data capture and sharing across scheme participants.
SIRA has commenced publishing a healthcare costs and outcomes data dashboard and is currently in the process of implementing broader data capability upgrades. This includes a strategy for a uniform method of data capture and governance across SIRA.
“The most important thing is ensuring the system is focussed on the injured person and they feel empowered by this information and not threatened by it”
– Person with lived experience
There are five initiatives that will enable outcomes costs and improve data quality across CTP and WC schemes. These are outlined in Table 1 below.
Table 1: Stream 1 initiatives
Initiative 1.1 Define outcome measures aligned to SIRA’s Value-Based Healthcare Outcomes Framework for clinical and patient reported measures, including clinician experience, for CTP and WC scheme participants.| Scheme outcomes | Actions |
|---|
- CTP and WC schemes have clearly defined outcome measures for clinical care, including psychosocial measures, return to work measures and patient reported measures, which are assessed and matched to the level of need (i.e. risk is stratified).
- SIRA and scheme participants understand whether injured people in the CTP and WC schemes are obtaining good health outcomes.
- SIRA and scheme participants understand whether clinicians in the CTP and WC schemes experience wellbeing, engagement, and satisfaction in the schemes.
- Scheme participants have clearly defined metrics across desired outcomes for data capture and sharing.
| - Work with scheme participants to develop high-level outcomes SIRA and scheme participants want to achieve through the introduction of outcome measures.
- Work with the appropriate clinical provider(s) to develop outcome measures across prioritised areas.
- Draft clinical and patient reported outcome measures to be prioritised for collection.
- Consult stakeholders to test and refine potential measures.
|
Initiative 1.2 Review outcome data sources across schemes including outcome capture and benchmarking by insurers, clinicians, and other service providers.2| Scheme outcomes | Actions |
|---|
- SIRA and scheme participants understand what and how outcome data is collected, stored, and shared in the CTP and WC schemes. This will include gaps in outcome capture and identification of additional data sources to support outcome capture.
- SIRA identifies opportunities to leverage existing data capture processes by external bodies relevant to the CTP and WC schemes.
| - Conduct an internal review of required outcomes captured by SIRA across insurers, clinicians, and other health providers. This should include a document review of current data capture policies and requirements.
Identify gaps and opportunities to improve outcome capture and benchmarking. - Consult with internal SIRA stakeholders to build on understanding of what is collected across CTP and WC schemes.
- Conduct an external review of outcome capture by health providers and scheme participants. This should include engaging clinical registries relevant to CTP and WC schemes, and NSW Health.
- Consult with external scheme participants to build on understanding of what is collected across CTP and WC schemes.
- Consolidate findings into a current state analysis that includes priority clinical outcomes and patient reported outcomes and the required data capabilities to support outcomes capture across CTP and WC schemes.
|
Initiative 1.3 Assess data capability of scheme participants to capture, onboard and manage data including barriers to sharing data across CTP and WC schemes.| Scheme outcomes | Actions |
|---|
- Scheme participants understand capabilities to capture, onboard and manage data, including identifying barriers to data sharing across CTP and WC schemes.
- Scheme participants understand where there is a need or opportunity to strengthen capability for high quality data capture.
| - Conduct an internal review of data capability to capture, onboard and manage data across insurers, clinicians, and other service providers.
Identify gaps and opportunities to build data capability within SIRA. - Consult with scheme participants to understand current data capability and identify gaps and opportunities across CTP and WC schemes.
- Review existing approaches across jurisdictions and/or internationally for outcomes capture and the associated data capability to support capture.
- Develop recommendations and high-level plan for addressing data capability gaps across scheme participants.
|
Initiative 1.4 Establish a method and system for data capture, storage, sharing and benchmarking for scheme participants that aligns to SIRA’s data governance framework.| Scheme outcomes | Actions |
|---|
- Scheme participants endorse SIRA systems to capture, store and share data and understand their roles and responsibilities in data capture, storage and sharing across CTP and WC schemes.
- SIRA has a plan for outcome data capture, storage, sharing and benchmarking that aligns to the SIRA data governance framework. This will include the capability to capture, share and report on clinical outcomes and PROMs and PREMs.
- SIRA has a process for monitoring and reporting outcome data that strengthens understanding of health outcomes across CTP and WC schemes.
| - SIRA to establish a working group with scheme participants to support the co-design of a method and system for data capture, storage, sharing and benchmarking.
- Test findings from the current state analysis developed in initiatives 1.2 and 1.3 with the data governance working group and explore desired future state of data sharing and outcome capture in the CTP and WC schemes.
- Draft a data governance plan. This should include an outline of roles, responsibilities and required system capabilities of scheme participants in outcome capture and data sharing.
- Identify method for capture, storage, sharing and benchmarking of desired future data sharing and outcome capture for 2-3 specific conditions.
|
Initiative 1.5 Prototype/trial a system for outcome data capture, storage and sharing for CTP and WC scheme data.| Scheme outcomes | Actions |
|---|
SIRA has a tested system for the outcome capture lifecycle (identify, capture, report, respond) for a small number of priority conditions, for example lower back pain management. | - Identify the system capabilities for outcome data capture, storage and sharing for CTP and WC schemes for 2-3 specific conditions.
- Engage stakeholders to identify potential systems that support outcome data capture, storage and sharing. This will include exploring opportunities for internal and/or external data storage.
- Test identified options with scheme participants. This could include establishing a working group to trial systems and identify strengths and weaknesses and preference for implementation.
|
Stream 2: Support enhanced clinical practice
Stream 2 will ensure evidence-based clinical practice is consistently embedded within CTP and WC schemes to maximise recovery for injured people and promote effectiveness and efficiency in care. This stream will support injured people to receive a holistic episode of care through the alignment of case managers, GPs and other treating doctors, and allied health practitioners across the claims journey.
SIRA has commenced work to support enhanced clinical practice. This includes:
- development of the mental health lived experience framework
- strengthening of WC guidelines for allied health practitioner approval
- publishing the medication management guide
- developing the CTP whiplash guidelines
- establishing the Back Injury Clinical Advisory Group. The advisory group has commenced work on a model of care for back injury, to be piloted in 2022.
“Involvement of senior clinicians and ongoing collaboration will be critical”
– Clinician
There are six initiatives that will enable SIRA to support enhanced clinical practice across CTP and WC schemes. These are outlined in Table 2 below.
Table 2: Stream 2 initiatives
Initiative 2.1: Understand variation in care and opportunities to drive evidence-based practice in the schemes.| Scheme outcomes | Actions |
|---|
- SIRA, insurers and healthcare providers understand variation of care across CTP and WC schemes and public and private systems.
- SIRA, in partnership with clinicians, identifies opportunities to develop new models of care to reduce low value care across CTP and WC schemes.
- SIRA establishes working relationships with healthcare providers to promote consistent clinical practice aligned to the value-based healthcare model.
| - Assess the extent of low value care across CTP and WC. This should draw on clinician input, findings from SIRA’s healthcare review, initiative 1.1 and existing best practice guidance for clinical practice.
- Consult clinicians working in the schemes, and the public and private systems to understand current practices around outcome measures, benchmarking, and best clinical practice in CTP and WC schemes.
- Develop case studies of the injured person’s journey across CTP and WC schemes to understand low value care, variations in care and future quality improvement activities. These case studies will also be used to support strengthening capability (see initiative 4.4).
- Work with clinicians to identify areas with variation in care across the schemes, and where possible across public and private systems. This will include developing an evidence base for defining low value care and opportunities to drive evidence-based practice.
|
Initiative 2.2: Leverage existing models of care (and develop new ones where required).| Scheme outcomes | Actions |
|---|
- Clinicians can access materials to support consistent evidence-based clinical practice when treating injured people across CTP and WC schemes.
- Injured people receive evidence-based treatment that maximises their recovery and drives better outcomes.
- Insurers and healthcare providers work together to allocate the right resources, at the right time when determining treatment plans for injured people.
| - Work with clinicians to identify an area or areas of priority for embedding existing models of care and/or developing new models of care. This should draw on findings from initiative 2.1.
- Establish a clinician-led working group for the identified area of clinical practice.
- Support clinicians through facilitating regular communications around working group progression.
- Consider how SIRA supports GPs and other healthcare providers to implement approved models of care.
|
Initiative 2.3: Develop guidance on best practice, including identifying opportunities to support implementation (and including leveraging existing guidelines).| Scheme outcomes | Actions |
|---|
- Clinicians deliver consistent best practice across claims management, clinical practice, and allied health treatment to maximise recovery for injured people.
- Injured people receive quality clinical care and case management that maximises recovery and drives better outcomes.
| - Continue work on developing a model of care for back pain with clinicians and the Agency for Clinical Innovation.
- Support clinicians to access and navigate information on treating injured people in compensation schemes.
- Review existing guidance on best practice and assess effectiveness of existing implementation across schemes with clinicians. This should include identifying opportunities to improve implementation.
- Use findings from initiatives 2.1 to 2.5 to identify priority areas that require supporting guidance to implement best practice within CTP and WC schemes.
- Use working groups established in initiative 2.2 to develop guidance on best practice that is suitable to case managers and healthcare providers across CTP and WC schemes.
- Consult clinicians and other scheme participants to test and refine guidance materials to ensure they effectively meet the needs of scheme participants.
- Finalise guides and make them available to scheme participants.
- Develop supporting communications campaign to encourage uptake of materials and implementation of guides by case managers and other key scheme participants.
|
Initiative 2.4: Identify opportunities and approaches for earlier intervention and multi-disciplinary assessments3 including through leveraging existing screening tools.| Scheme outcomes | Actions |
|---|
- In Case managers and clinicians understand patient complexity and risk through early assessment of clinical and psychosocial outcomes and return to work indicators.
- Case managers and clinicians work together to develop treatment plans aligned to the injured person’s desired health outcomes and the relevant scheme outcomes, for example return to work objectives.
- Injured people receive the right treatment, at the right time aligned to their entire episode of care to maximise recovery and drive health outcomes.itiative 2.4:
- Identify opportunities and approaches for earlier intervention and multi-disciplinary assessments including through leveraging existing screening tools.
| - Consult healthcare providers, insurers, and other jurisdictions to understand the desired objectives of a screening tool in scheme case management.
- Review existing screening tools and identify strengths and weaknesses of each option, including alignment to the needs identified in stakeholder consultations.
- Engage with key clinicians and insurers to establish a working group to map the required processes that will enable early multi-disciplinary assessments for injured people across CTP and WC schemes.
|
Initiative 2.5: Establish a process for research, evaluation, and experience investigation.| Scheme outcomes | Actions |
|---|
- Clinicians have consistent processes for monitoring, research, evaluation, and experience investigation activities for health outcomes measurement.
- SIRA metrics reflect evidence-based practice and health outcomes that matter to injured people. nitiative 2.5: Establish a process for research, evaluation, and experience investigation.
| - Review existing research and evaluation and experience analysis processes across CTP and WC schemes and identify opportunities to document a consistent process for internal and external SIRA stakeholders.
- Consult internal and external SIRA stakeholders to identify opportunities to improve research, evaluation, and experience analysis.
- Develop a framework that outlines SIRA’s process for research, evaluation, and experience investigation. This should draw on findings from the review and stakeholder consultation.
|
Initiative 2.6: Lead the co-design of a clinical governance framework for value-based healthcare for CTP and WC schemes.| Scheme outcomes | Actions |
|---|
- CTP and WC have a clear clinical governance framework that drives consistent practice across schemes, including public and private systems.
- Scheme participants, SIRA and other regulators understand provider roles and responsibilities. This would include accountability processes to safeguard high standards of care and drive health outcomes across the CTP and WC schemes.
- SIRA has established ways of working with other regulators whose work intersects with SIRA’s.
| - Establish a working group (or leverage an existing working group) with key stakeholders to develop a clinical governance framework. This should include clinicians and other healthcare providers, medical representative bodies and other regulators involved in monitoring clinical practice.
- Consult scheme participants and other key regulators to understand and identify roles and responsibilities in driving health outcomes across CTP and WC schemes.
- Test and refine the clinical governance framework with key stakeholders required to endorse the clinical governance framework.
- Regularly update scheme participants on the development of the clinical governance framework.
Seek endorsement of the clinical governance framework. - Develop a communications campaign to support the implementation of the clinical governance framework.
|
Stream 3: Streamline administration and reduce leakage
Stream 3 will ensure CTP and WC case management aligns to the SIRA value-based healthcare approach including relevant benchmarks, guidelines, and frameworks. It will streamline the administration process to enable efficiencies in resource allocation and to better support recovery and health outcomes. A streamlined administration process will improve information sharing, reduce delays in care and drive better treatment outcomes and scheme experiences for injured people.
SIRA has commenced work to streamline administration and reduce leakage. This includes:
- a review of health expenditure leakage
- a review of the hearing loss claims process
- benchmarking of WC fees against comparator fees
- establishing a SIRA and insurers medical payment working group.
“It is about how the systems connect together and what it looks like on the ground [for the injured person]”
– Insurer
There are five initiatives that will enable SIRA to streamline administration and reduce leakage. These are outlined in Table 3 below.
Table 3: Stream 3 initiatives
Initiative 3.1: Develop future state process maps for CTP and WC per feedback on existing pain points and review of best practice.| Scheme outcomes | Actions |
|---|
- Scheme participants understand the desired future administrative process for CTP and WC. This will support scheme participants to streamline processes and reduce duplication. This includes:
- aligning future administrative processes for CTP and WC with best practice
- improving information sharing and reduce delays in care to drive better outcomes for injured people
- increasing efficiency in CTP and WC schemes.
- SIRA has strengthened its relationship with stakeholders and trust in the schemes through addressing feedback on administrative burden.
- Case managers have processes for improved case management across the claims journey for CTP and WC schemes.
| - Review best practice in CTP and WC case management and administrative processes including through consultation with other jurisdictions.
- Co-design future state process maps with stakeholders including clinicians, administrative staff, insurers, and injured people.
- Identify any regulatory changes required to enable future state (see optional actions below).
Finalise future state map. - Develop communications campaign for CTP and WC schemes emphasising the purpose and benefits for different stakeholder groups.
- Communicate changes to the schemes emphasising the benefits for different stakeholder groups.
- Develop best practice guides, templates, and tools to enable future state (see initiative 3.2).
- Engage stakeholders to regularly seek feedback and allow continuous improvement.
Optional actions if required: - Develop a business case to justify any change to regulations or guidelines required to streamline administrative processes. This will include benefits, costs, and risks.
- Seek SIRA board endorsement of the business case.
|
Initiative 3.2 Develop templates for clinicians and insurers to support streamlined administrative processes across CTP and WC schemes.| Scheme outcomes | Actions |
|---|
- Scheme participants have consistent requests for information and increased access to information throughout the claims journey.
- CTP and WC administrative processes have reduced duplication of information.
- Claims management is improved for injured people, maximises recovery and drives better outcomes.
| - Using the future state maps developed in initiative 3.1, identify key points where templates would support a streamlined administrative process across CTP and WC schemes.
- Consult key stakeholders to understand what information needs to be collected in the templates. This may include clinicians, insurers, and injured people.
- Identify opportunities to test and refine templates with key stakeholders.
- Update templates to reflect any key learnings during the user testing.
- Seek endorsement and approval of developed templates, to enable implementation across CTP and WC schemes.
|
Initiative 3.3 Consider options for digital processes.| Scheme outcomes | Actions |
|---|
- Improved information sharing and data capture, and reduced duplication across the claims journey.
| - Using the future state maps developed in initiative 3.1, identify key points where digitisation would support a streamlined administrative process across CTP and WC schemes.
- Review existing use of digital systems in other jurisdictions and/or similar schemes/systems that rely on claims management processes. The review should identify the strengths and weaknesses of each option, including any risks and desired outcomes.
- Consolidate findings and seek stakeholder feedback through a public consultation period to understand scheme participants’ buy-in and preference for digital options.
|
Initiative 3.4 Assess effectiveness of healthcare review mechanisms in meeting objectives. This may include the application of the medico-legal framework and peer review processes.| Scheme outcomes | Actions |
|---|
- Outcomes to be achieved to be determined as part of the project, but could include reduced treatment delays and disputes, improved quality of healthcare and improved health outcomes.
- Increased evidence-based practice, including through peer-to-peer knowledge transfer.
| - Identify key review mechanisms and their objectives across the schemes.
- Assess the operation of key review mechanisms to date to understand whether they are meeting required objectives.
- Use findings from the preliminary assessment to seek feedback on the effectiveness of review mechanisms from scheme participants. This may include providing key questions for stakeholders to respond to in order to receive targeted feedback on potential issues.
- Consider feedback on the operation of key review mechanisms, including identifying opportunities for improvement.
|
Initiative 3.5 Improve compliance and enforcement approaches across CTP and WC schemes to identify and address regulatory gaps.| Scheme outcomes | Actions |
|---|
- SIRA has improved compliance and enforcement across CTP and WC schemes, including identification of opportunities to strengthen regulatory gaps.
- Clinicians and insurers understand their compliance obligations across CTP and WC schemes.
| - Develop data analytic tools to support improved monitoring of insurer and healthcare provider compliance and enforcement across CTP and WC schemes.
- Identify potential areas for improvement in compliance and enforcement.
- Implement proposed changes currently before the Parliament in the Motor Accidents and Workers Compensation Legislation Amendment Bill 2021, if passed.
|
Stream 4: Develop scheme capability in value-based healthcare
Stream 4 will enable a consistent approach to value-based healthcare across the CTP and WC schemes. SIRA, in partnership with scheme participants, will provide education, advocacy and increased cross-scheme participant knowledge sharing. This will embed consistent understanding and improved capability to ensure service provision aligns to value-based healthcare models and drives better outcomes.
SIRA has commenced value-based healthcare capability building through the co-design process that informed this implementation plan. This included stakeholder engagement with SIRA staff, insurers and employer representatives, medical and allied health practitioners, and people with lived experience of the schemes. These engagement activities included defining value-based healthcare and its relevance to the CTP and WC schemes. SIRA staff have also piloted an accredited value-based healthcare course in partnership with UNSW.
“Health literacy is important to support the injured worker push and pull information that meets their needs across the process
– Person with lived experience
There are five initiatives that will enable SIRA to develop scheme capability in value-based healthcare. These are outlined in Table 4 below.
Table 4: Stream 4 initiatives
Initiative 4.1: Map existing knowledge and capabilities for value-based healthcare across scheme participants| Scheme outcomes | Actions |
|---|
- SIRA understands scheme participants’ current knowledge and capability to implement value-based healthcare.
- SIRA has baseline measurements to track capability development and monitor the implementation of value-based healthcare knowledge and capability.
| - Identify desired capabilities across the schemes.
- Review existing materials and programs available to build knowledge and capability on value-based healthcare.
- Consult with scheme participants to identify and map their existing value-based healthcare knowledge. This could include developing a scheme-wide survey to track knowledge and capability progress.
- Collate findings and identify gaps in value-based healthcare knowledge and capability. These findings will inform the materials and programs for initiatives 4.2 to 4.4.
|
Initiative 4.2: Identify and implement opportunities to build value-based healthcare capability within SIRA.| Scheme outcomes | Actions |
|---|
- SIRA is better equipped to drive value-based healthcare in the CTP and WC schemes, including supporting scheme participants and injured people to build their value-based healthcare knowledge and capability.
| - Use findings from initiative 4.1 to inform and develop education materials and/or program options on value-based healthcare in CTP and WC schemes.
- Implement education materials and/or programs across SIRA. This could include facilitating access to existing accredited programs.
- Encourage uptake through an internal communications campaign.
|
Initiative 4.3: Identify and implement opportunities for injured people to access and navigate value-based healthcare provision with improved health literacy.| Scheme outcomes | Actions |
|---|
- Injured people have a clear understanding of value-based healthcare and feel empowered to ask the right questions and make informed decisions throughout their treatment and claims journey.
| - Use findings from initiative 4.1 to inform and develop education materials and/or program options on value-based healthcare in CTP and WC schemes. This should include the purpose of patient reported outcome measures to better inform treatment plans.
- Provide access to materials and programs across CTP and WC schemes. This could include creating an online repository of resources that providers can link to scheme participants.
- Develop external communications campaign to inform injured people that materials are available to support the CTP and WC claims journey and help improve outcomes.
- Ongoing review and update of materials to ensure alignment to best practice value-based healthcare models.
|
Initiative 4.4 Identify and implement opportunities to build value-based healthcare capability for insurers and clinicians.| Scheme outcomes | Actions |
|---|
- Insurers and clinicians consistently build value-based healthcare knowledge.
- Clinicians understand how to provide treatment that aligns to the value-based healthcare model, including the capability to meet their roles and responsibilities in outcome capture and measurement.
- Insurers and clinicians understand the different trajectories of injured people through the claims journey.
- Injured people receive quality clinical care that maximises recovery and drives better outcomes.
| - Use findings from initiative 4.1 and initiative 1.3 to inform and develop education materials and/or program options on value-based healthcare in CTP and WC schemes. This should include materials to address data capability gaps identified in stream 1.
- Engage people with lived experience to develop case studies that identify future quality improvement activities for insurers and clinicians across the claims management journey (see initiative 2.1 for more information).
- Provide access to materials and programs across CTP and WC schemes. This could include creating an online repository of resources that insurers and clinicians can access.
- Ongoing review and update of materials to ensure alignment to best practice value-based healthcare models.
|
Initiative 4.5 Develop mechanisms for clinician peer-to-peer discussion and mentoring across private and public systems.| Scheme outcomes | Actions |
|---|
- Clinicians across private and public systems provide consistent value-based healthcare.
- Injured people in CTP and WC schemes receive the same quality of care whether they are accessing private or public systems.
- CTP and WC schemes deliver improved outcomes for injured people.
| - SIRA will regularly engage clinicians working in WC and CTP and across the private and public system to understand models of care, best practice and outcomes captured within the schemes.
- SIRA will advocate for peer-to-peer discussions and mentoring opportunities across public and private systems to promote best practice in value-based healthcare in CTP and WC schemes.
|
4. Co-design process
4.1. Ongoing stakeholder engagement
The implementation plan was developed through a co-design process with a range of stakeholders (see Section 2.3). SIRA will continue to consult and co-design with stakeholders during the lifecycle of the implementation plan. Stakeholders have already noted through the co-design process that continuing to build trust with scheme participants will be a key enabler for the implementation plan. This will include:
- identifying key stakeholders to engage and opportunities for engagement e.g. working groups
- engaging people with lived experience and health consumer groups to inform co-design of value-based healthcare. This may include establishing a mechanism for regular input from people with lived experience.
- developing a communications plan to support transformation and undertake communications activities.
4.2. Key themes from the co-design process
SIRA invited a range of stakeholders to participate in a co-design process for the implementation plan. The initiatives identified most important by each stakeholder group are outlined in Figure 7, below. Key insights for implementation from each group of stakeholders consulted through the co-design process are outlined in Table 5.
Figure 7: Initiatives identified most important by each group of stakeholders
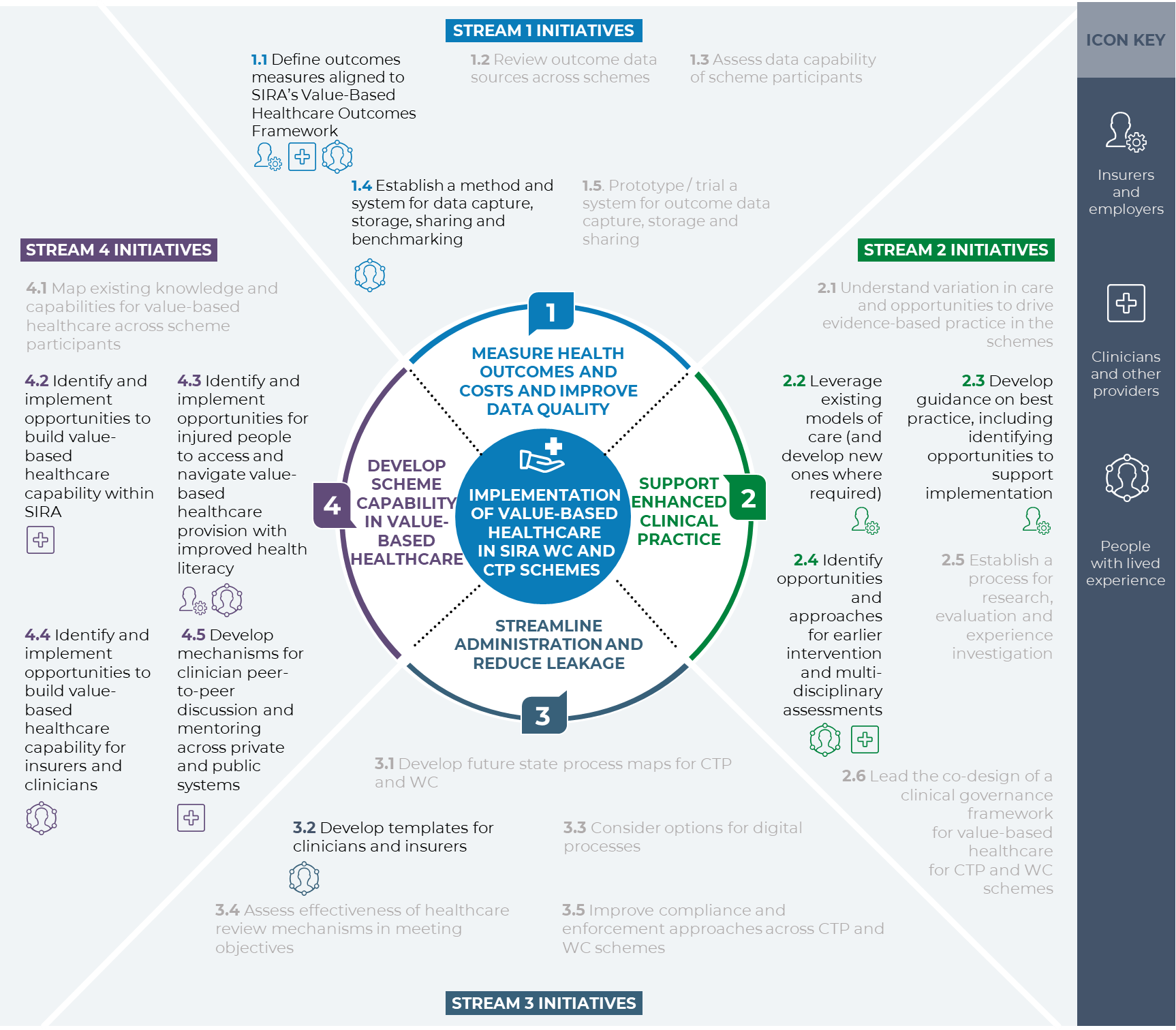
Figure 7: Initiatives identified most important by each group of stakeholders
Table 5: Feedback and insights from stakeholder groups on the implementation plan
| Stakeholder group | Key insights for implementation |
|---|
| Insurers and employers4 | - A lot of data is available for tracking outcomes, but it is not consolidated, hard to access and will be difficult to align.
- Enforcement penalties for providers should be considered to disincentivise low value care.
- Existing WC legislation, i.e. the "reasonably necessary" criteria, does not give insurers sufficient power to reject low value healthcare.
- It is important to understand the impact of changing workplace relationships on psychosocial outcomes.
- Reducing administration burden is key to improving the speed and cost of healthcare.
|
| People with lived experience | - Current processes can leave injured people feeling disempowered and contributes to a lack of trust in the schemes.
- Access and ownership over data and information sharing is critical for meaningful patient reported outcome measures.
- Building health literacy for injured people will be an enabler for information sharing and outcome measures.
- Through the implementation plan SIRA should consider which outcomes (including the return to work outcome) are best aligned to the intentions of the WC Acts.
|
| Clinicians and other providers | - Administrative burden across the claims journey as a challenge to quality care. This includes duplication of information and delays in care.
- Trust is a key enabler to the success of the implementation plan.
- Initiatives that are about improving clinical practice need to be clinician-led.
- Education materials need to be consistent and available to all.
- Real-time indicators on scheme performance will support clinicians to improve quality of care.
- Systems should share indicators on risk identification and stratification for clinicians.
|
5. Implementation approach
This section provides an implementation plan for the four streams of work. It is structured by stream and should be read in conjunction with Section 3.
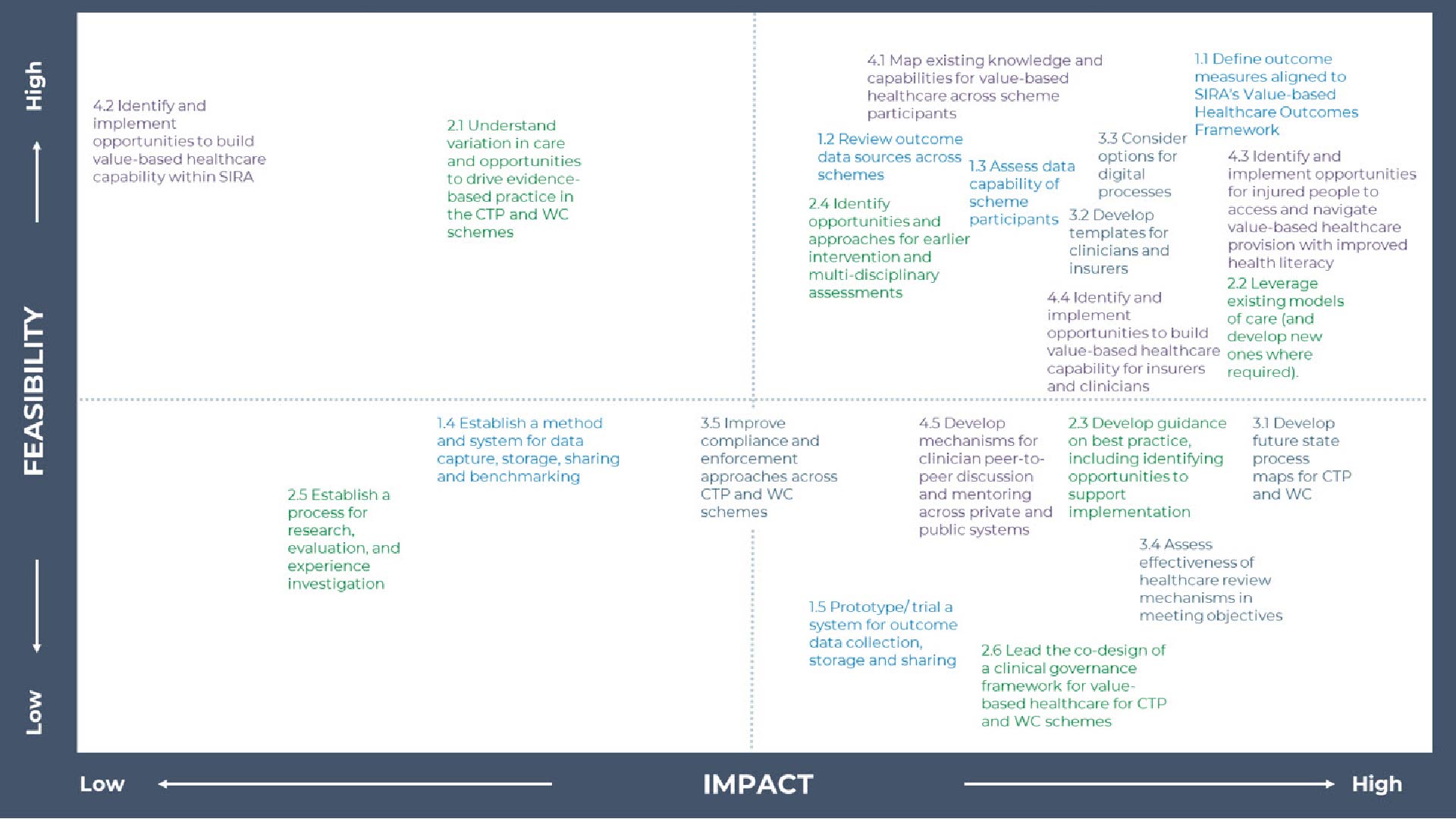
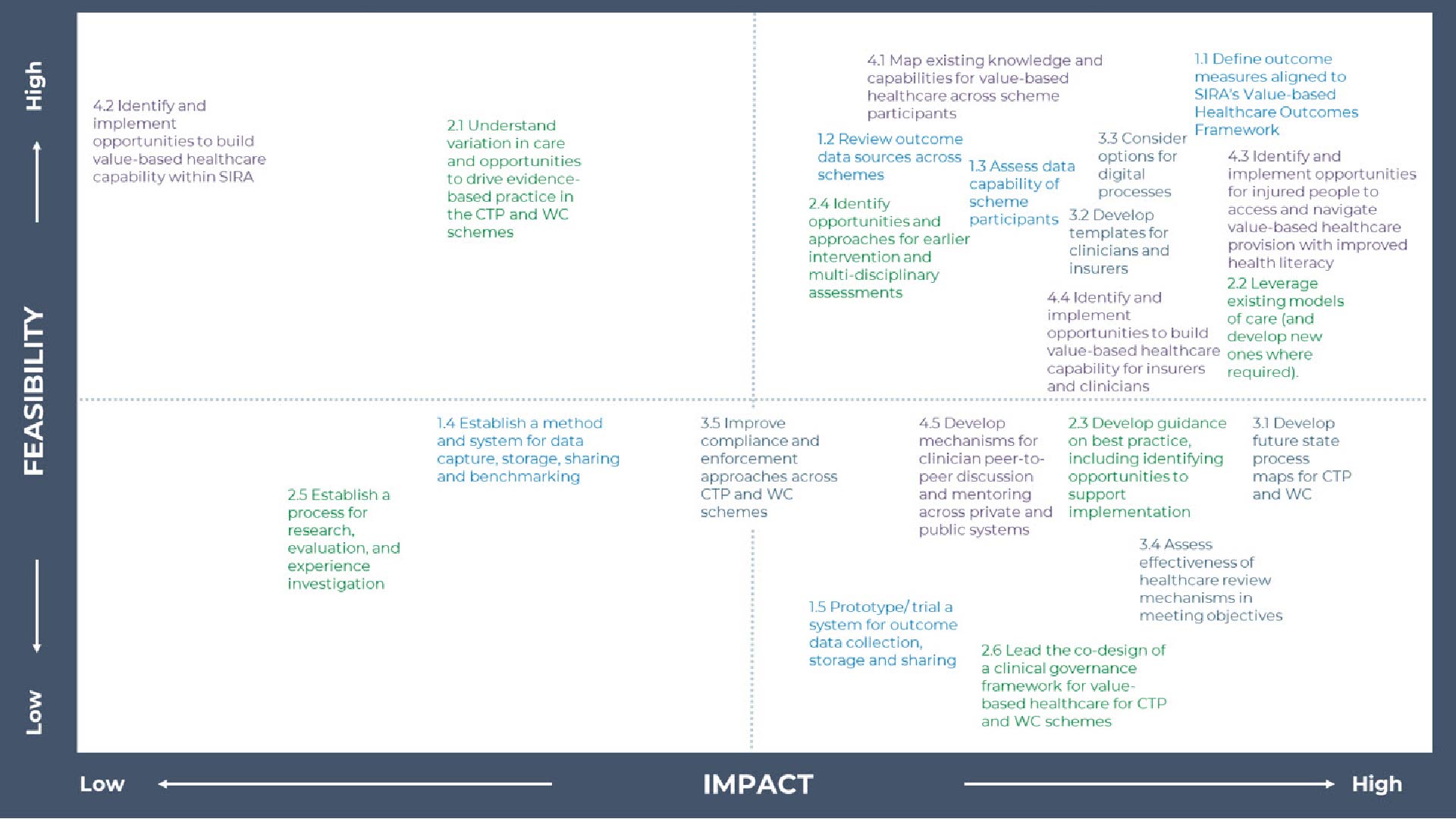
SIRA undertook a prioritisation process with stakeholders during the co-design work to assist in the development of the approach to implementing the plan, which included identifying which initiatives will have the highest impact and are most feasible.
The timeline for commencement of the initiatives is outlined in Figure 8, below. Table 6, overleaf, outlines the scheme participants with responsibility in delivering each stream or initiative. It also provides additional detail on the timeline for implementation.
Figure 8: Implementation horizons for the initiatives
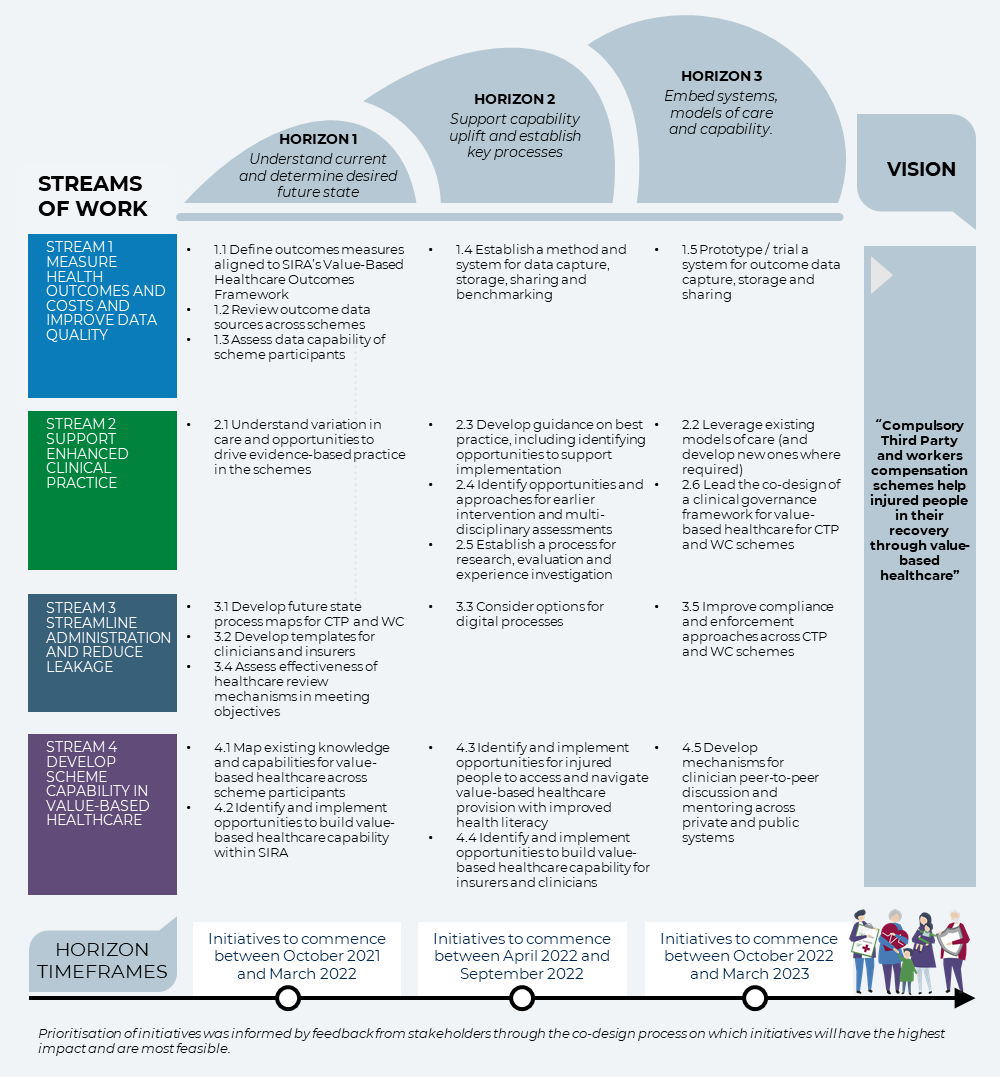
Figure 8: Implementation horizons for the initiatives
Table 6: Implementation responsibility and timing for streams of work
| Implementation activity | Responsible | Timeline |
|---|
| Stream 1: Measure health outcomes and costs and improve data quality |
|---|
| Define outcome measures aligned to SIRA Value-based Healthcare Outcomes Framework | SIRA in collaboration with scheme participants | Horizon 1: October 2021 – March 2022 |
| Review outcome data sources across schemes | Horizon 1: October 2021 – March 2022 |
| Assess data capability of scheme participants | Horizon 1: October 2021 – March 2022 |
| Establish a method and system for data capture, storage, sharing and benchmarking | Horizon 2: April 2022 – September 2022 |
| Prototype / trial a system for outcome data capture, storage and sharing | Horizon 2: April 2022 – September 2022 |
| Stream 2: Support enhanced clinical practice |
|---|
| Understand variation in care and opportunities to drive evidence-based practice in the schemes | SIRA in collaboration with scheme participants | Horizon 1: October 2021 – March 2022 |
| Leverage existing models of care (and develop new ones where required) | Scheme clinicians | Horizon 3: October 2022 – March 2023 |
| Develop guidance on best practice, including identifying opportunities to support implementation | SIRA in collaboration with scheme participants | Horizon 2: April 2022 – September 2022 |
| Identify opportunities and approaches for earlier intervention and multi-disciplinary assessments | SIRA in collaboration with scheme participants | Horizon 2: April 2022 – September 2022 |
| Establish a process for research, evaluation, and experience investigation | SIRA | Horizon 2: April 2022 – September 2022 |
| Lead the co-design of a clinical governance framework for value-based healthcare for CTP and WC schemes | SIRA in collaboration with scheme participants, and other relevant regulators | Horizon 3: October 2022 – March 2023 |
| Stream 3: Streamline administration and reduce leakage |
|---|
| Develop future state process maps for CTP and WC | SIRA | Horizon 1: October 2021 – March 2022 |
| Develop templates for clinicians and insurers | SIRA in collaboration with scheme participants | Horizon 1: October 2021 – March 2022 |
| Consider options for digital processes | SIRA in collaboration with scheme participants | Horizon 2: April 2022 – September 2022 |
| Assess effectiveness of healthcare review mechanisms in meeting objectives | SIRA | Horizon 1: October 2021 – March 2022 |
| Improve compliance and enforcement approaches across CTP and WC schemes | SIRA | Horizon 3: October 2022 – March 2023 |
| Stream 4: Develop scheme capability in value-based healthcare |
|---|
| Map existing knowledge and capabilities for value-based healthcare across scheme participants | SIRA | Horizon 1: October 2021 – March 2022 |
| Identify and implement opportunities to build value-based healthcare capability within SIRA | SIRA | Horizon 1: October 2021 – March 2022 |
| Identify and implement opportunities for injured people to access and navigate value-based healthcare provision with improved health literacy | SIRA | Horizon 2: April 2022 – September 2022 |
| Identify and implement opportunities to build value-based healthcare capability for insurers and clinicians | SIRA | Horizon 2: April 2022 – September 2022 |
| Develop mechanisms for clinician peer-to-peer discussion and mentoring across private and public systems | SIRA in collaboration with clinicians | Horizon 3: October 2022 – March 2023 |
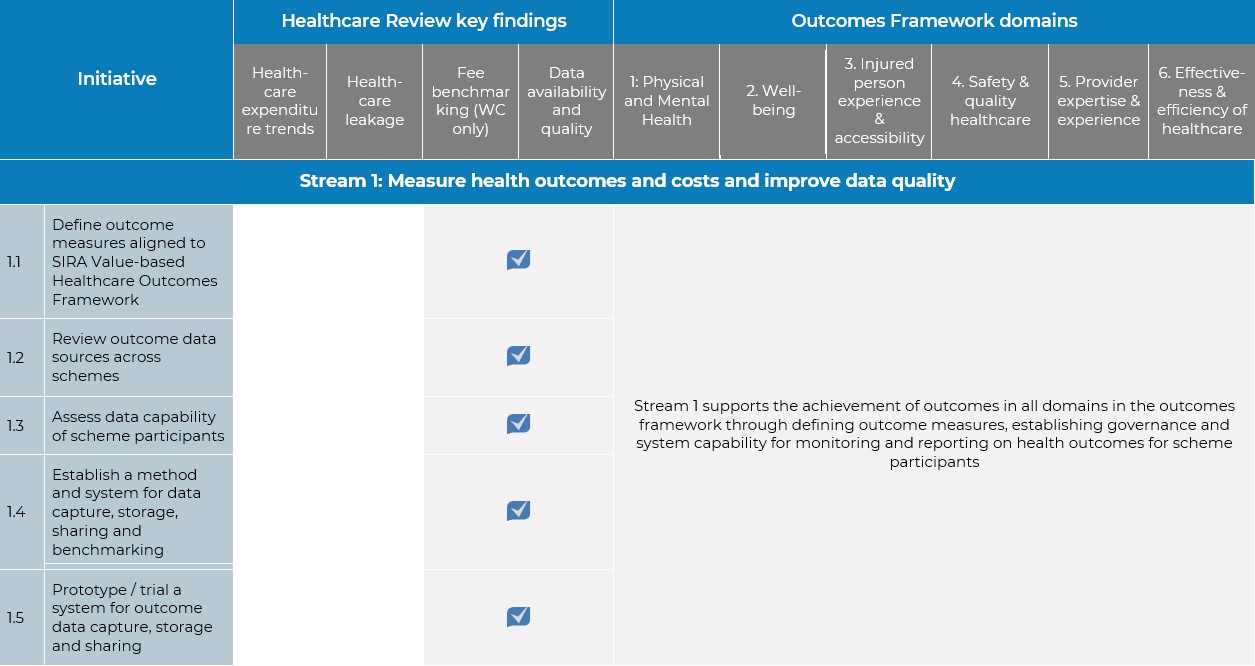
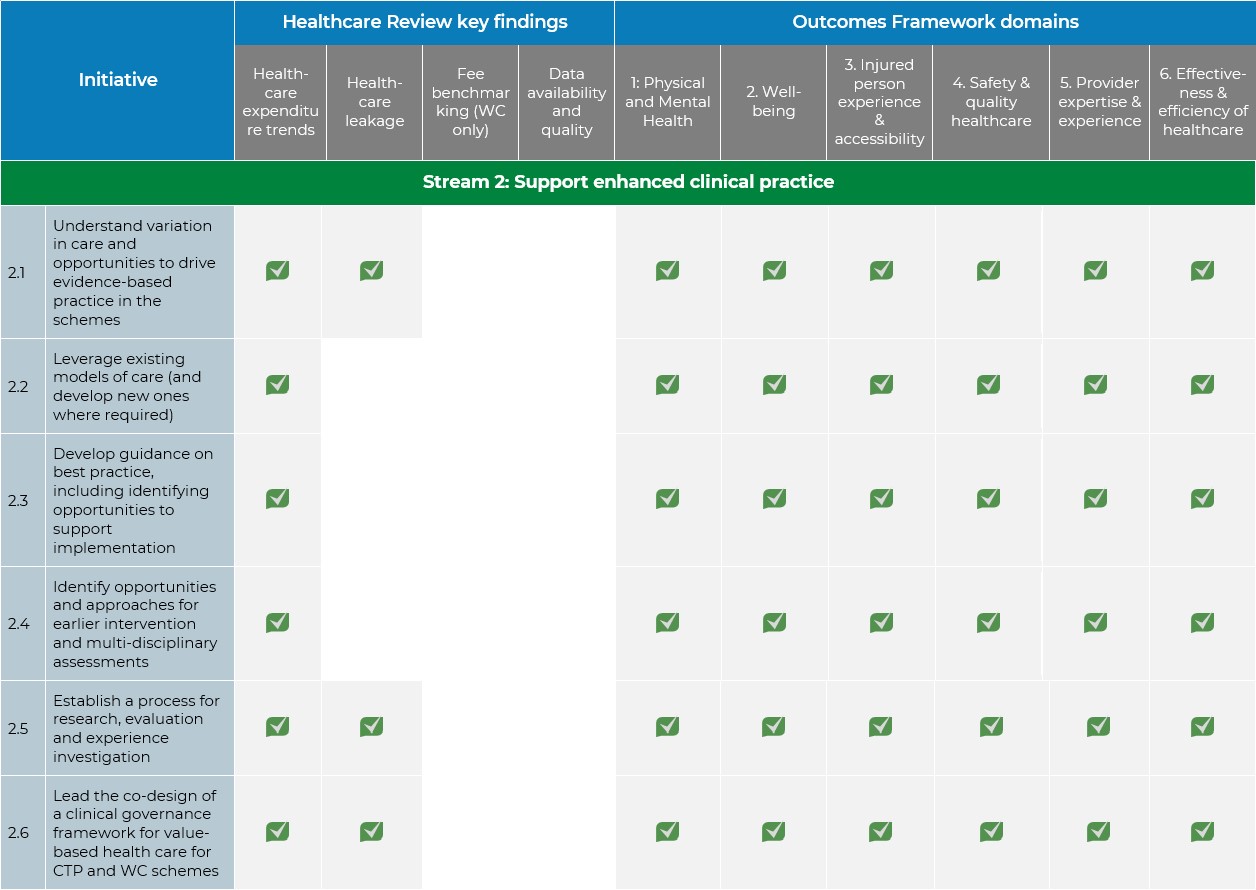
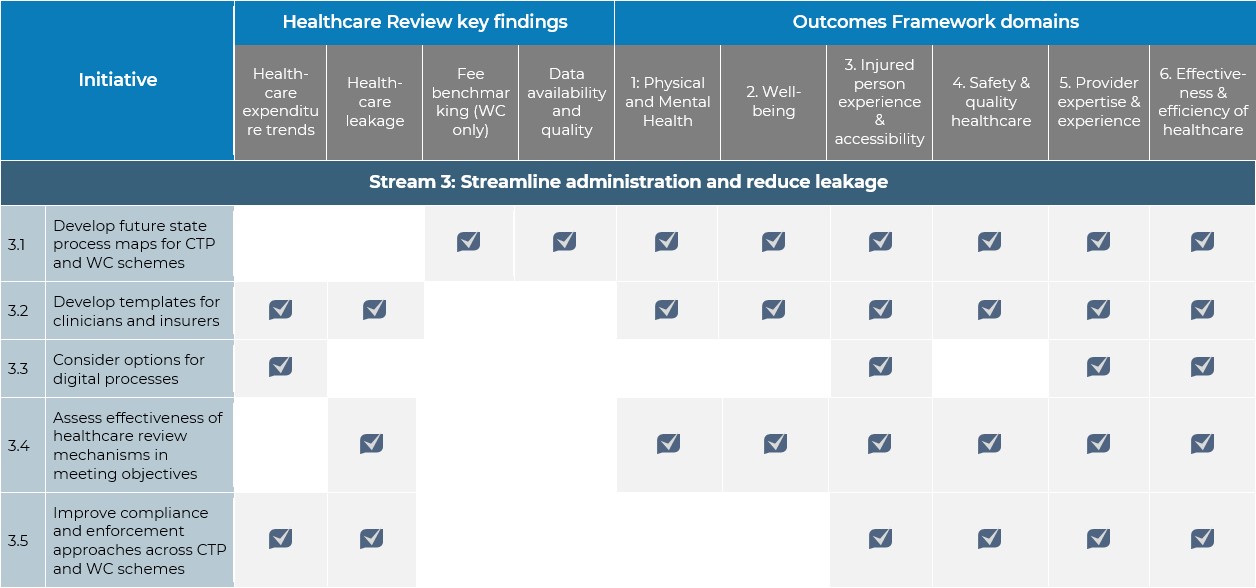
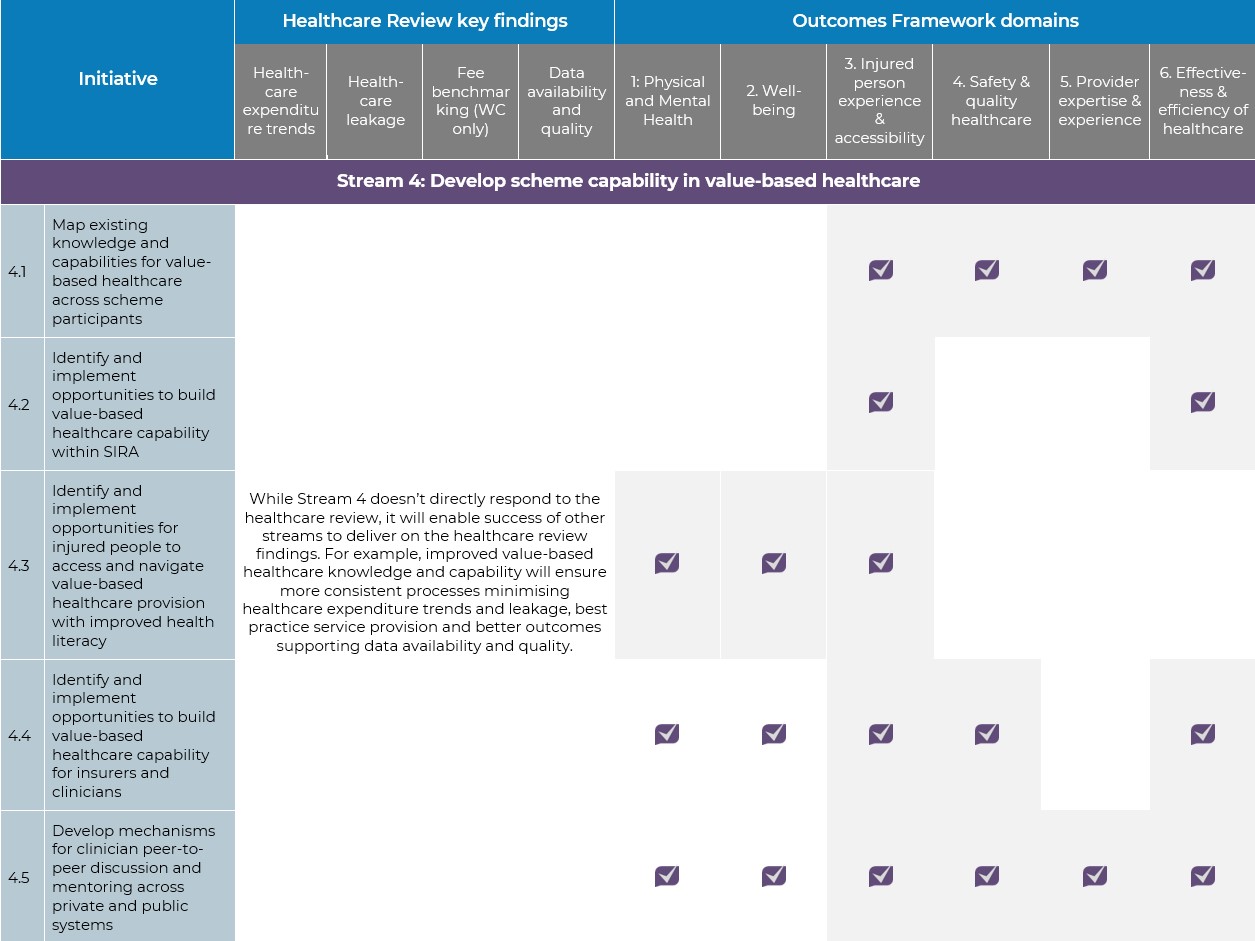
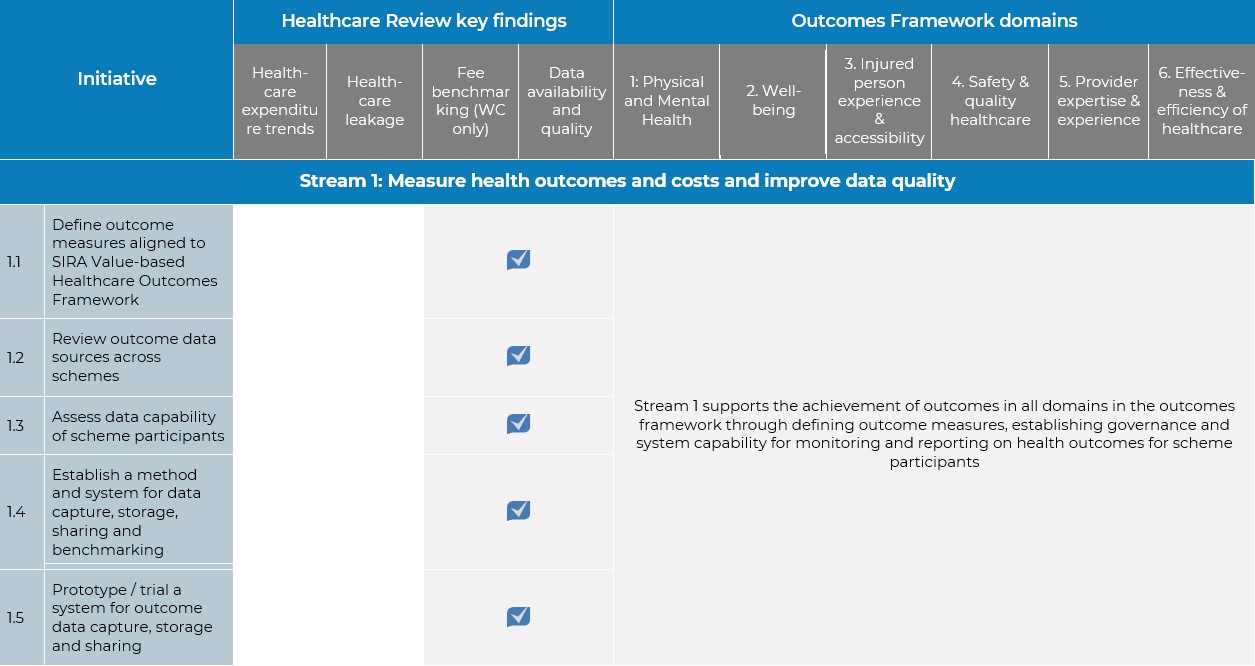
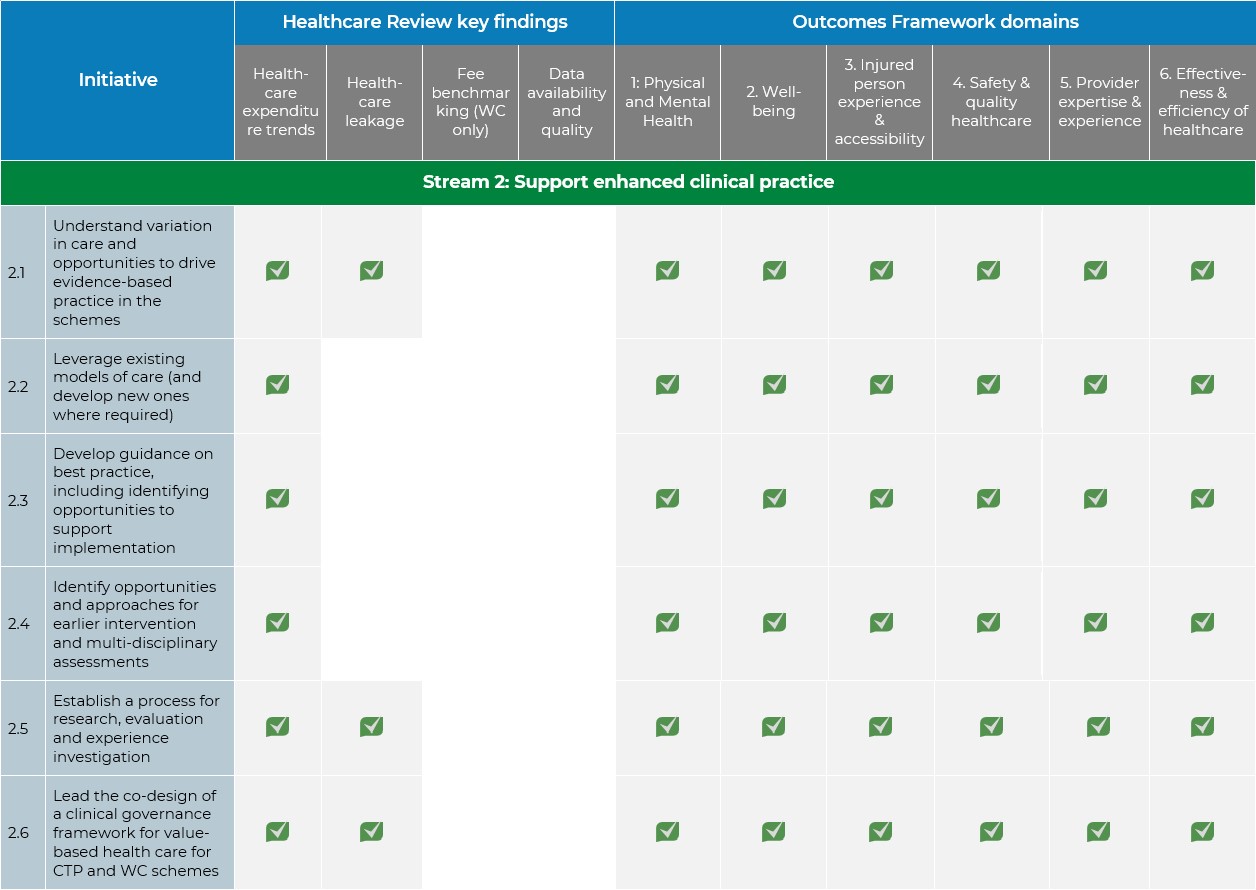
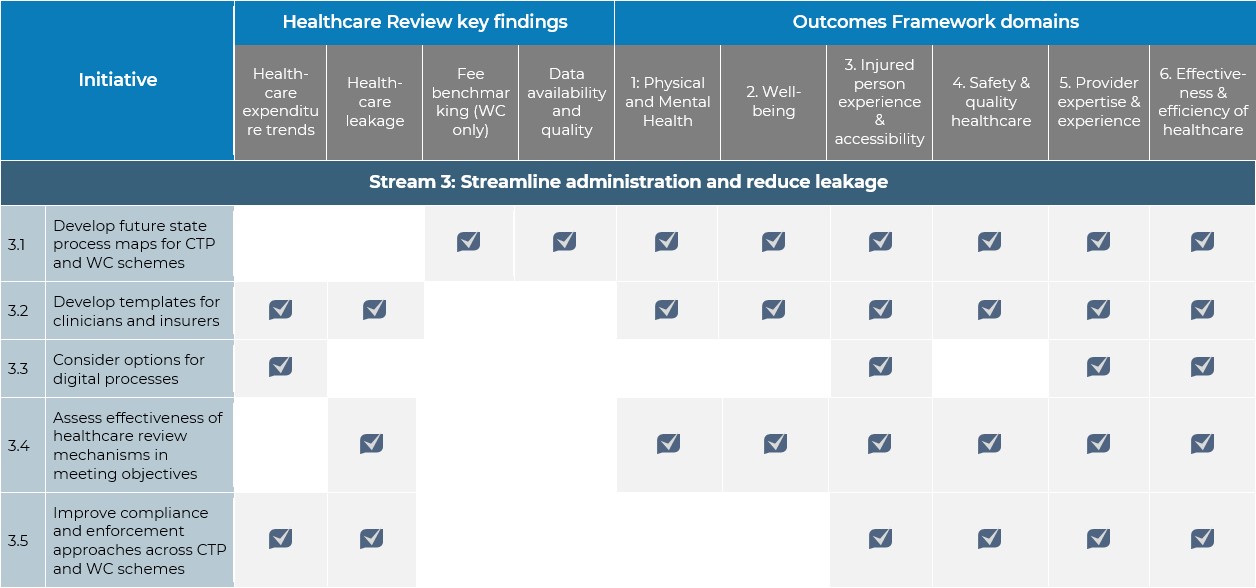
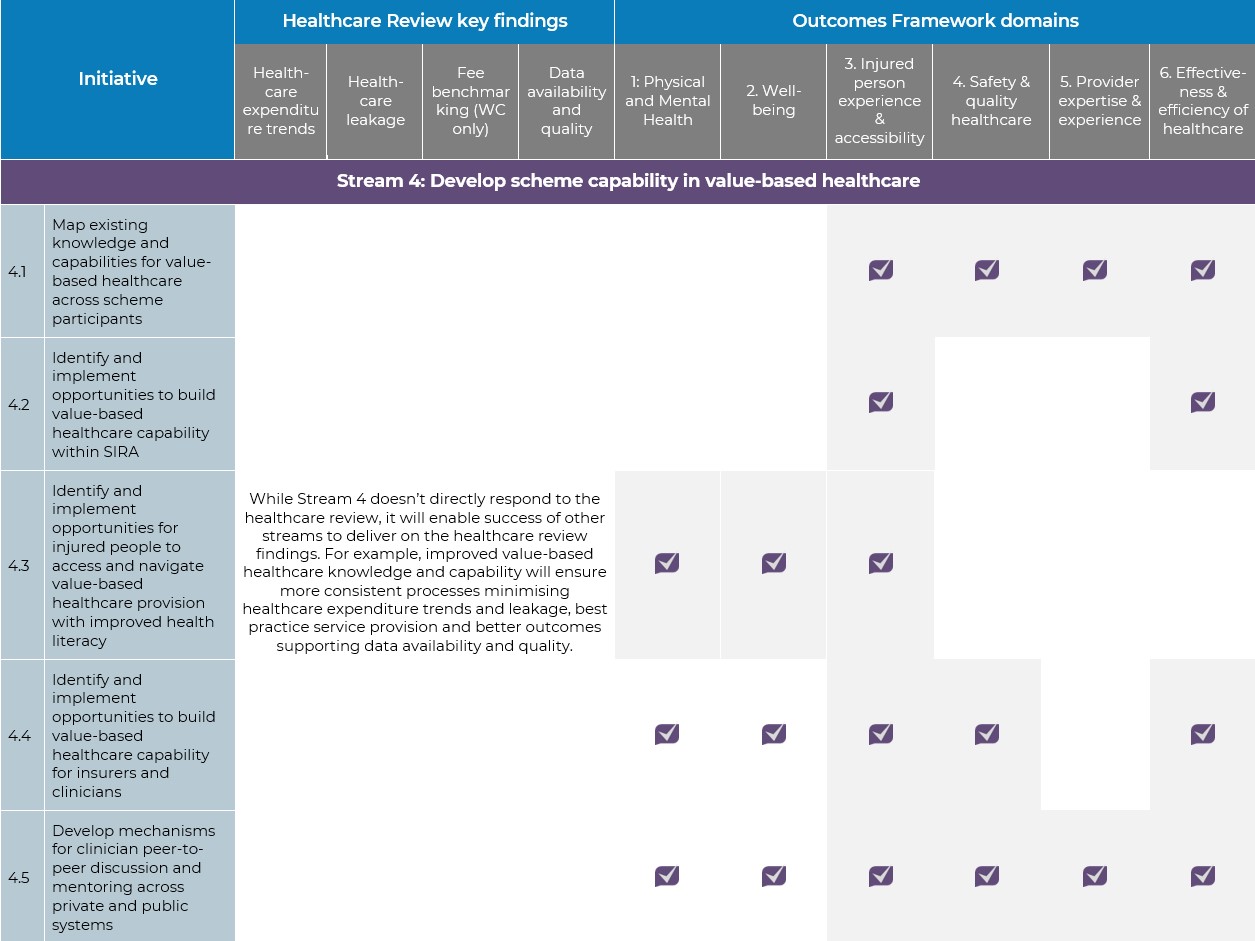
Appendix A: The implementation plan’s alignment with the findings of the Healthcare Review and the domains of the health outcomes framework
This implementation plan responds to the Independent Review Report (independent review conducted by retired Supreme Court Judge, the Hon Robert McDougall QC of icare and State Insurance and Care Governance Act) recommendation that SIRA should develop an accelerated plan for implementation of the findings of its Healthcare Review, with additional resources allocated where necessary. SIRA has also recently published the Value-Based Healthcare Outcomes Framework with six domains for achieving the vision of value-based healthcare. Table 7, below, outlines how the initiatives respond to these two documents.
Table 7: Alignment of initiatives to the Healthcare Review’s key findings and health outcomes framework domains
Appendix B: Impact and feasibility assessment of initiatives
SIRA invited stakeholders to provide feedback on the impact and feasibility of the different initiatives.
This feedback is mapped in Figure 9.
Appendix C: List of organisations and people consulted in the development of this plan
Individuals with lived experience of the compensation scheme
Australian Faculty of Occupational and Environmental Medicine
Australian Medical Association (NSW)
Australian Orthopaedic Association
Australian Physiotherapy Association
Australian Psychological Society
Australian Society of Anaesthetists
Australian Society of Orthopaedic Surgeons
Australian Society of Otolaryngology Head and Neck Surgery
Australian Society of Plastic Surgeons
Exercise and Sports Science Australia
Neurosurgical Society of Australasia
Occupational Therapy Australia
Pharmacy Guild of Australia
Royal Australian College of Surgeons (NSW)
Royal Australian College of General Practitioners
Individual clinicians working in the scheme
Individual medical and allied health academics
NSW Ministry of Health
NSW Agency for Clinical Innovation
Motorcycle Council of NSW
NSW Business Council
The Australian Industry Group
Australian Manufacturing Workers Union
Construction, Forestry, Mining and Energy Union
Allianz
Catholic Church Insurance
Coal Mines Insurance
Coles Limited
EML
Guild Insurance
IAG
icare
NSW Self-Insurers Association
QBE
Racing NSW
StateCover
Suncorp
Youi
Footnote
1. SIRA’s approach to value-based healthcare is consistent with the principles and definitions set out by NSW Ministry of Health.
2. “Outcome capture” includes data collected by SIRA and access to data collected and captured by others.
3. Multi-disciplinary assessments would be conducted by multi-disciplinary teams including the injured person’s GP, surgeon, and allied health provider.
4. Several employer groups were invited to the co-design workshop, however only one was able to attend. SIRA will continue to seek feedback from employer groups on implementation of value-based healthcare initiatives.