Position Statement from the Australian Diabetes Society*, New Zealand Society for the Study of Diabetes†, Royal College of Pathologists of Australasia‡ and Australasian Association of Clinical Biochemists§.
Peter G Colman*, David W Thomas‡, Paul Z Zimmet*, Timothy A Welborn*, Peter Garcia-Webb§ and M Peter Moore†.
First published in the Medical Journal of Australia (MJA 1999, 170: 375-378). Reprinted with permission.
Introduction
Recently, there has been major growth in knowledge about the aetiology and pathogenesis of different types of diabetes and about the predictive value of different blood glucose levels for development of complications. In response, both the American Diabetes Association (ADA) and the World Health Organization (WHO) have re-examined, redefined and updated the classification of and criteria for diabetes, which have been unchanged since 1985. While the two working parties had cross-representation, they met separately, and differences have emerged between their recommendations.
The ADA published its final recommendations in 19971, while the WHO group published its provisional conclusions for consultation and comment in June 19982.
The WHO process called for comments on the proposal by the end of September 1998, with the intention of finalising definitive classification and criteria by the end of December 1998 and of publishing these soon thereafter. However, WHO publications need to go through an internal approval process and it may be up to 12 months before the final WHO document appears.
A combined working party of the Australian Diabetes Society, New Zealand Society for the Study of Diabetes, Royal College of Pathologists of Australasia and Australasian Association of Clinical Biochemists was formed to formulate an Australasian position on the two sets of recommendations and, in particular, on the differences between them. This is an interim statement pending the final WHO report, which will include recommendations on diabetes classification as well as criteria for diagnosis. We see it as very important to inform Australasian health professionals treating patients with diabetes about these changes.
Key messages
Diagnosis of diabetes is not in doubt when there are classical symptoms of thirst and polyuria and a random venous plasma glucose level ≥ 11.1 mmol/L.
The Australasian Working Party on Diagnostic Criteria for Diabetes Mellitus recommends:
- immediate adoption of the new criterion for diagnosis of diabetes as proposed by the ADA and the WHO – fasting venous plasma glucose level ≥ 7.0 mmol/L
- immediate adoption of the new classification for diabetes mellitus proposed by the ADA and WHO, which comprises four aetiological types – type 1, type 2, other specific types, and gestational diabetes – with impaired glucose tolerance and impaired fasting glycaemia as stages in the natural history of disordered carbohydrate metabolism
- awareness that some cases of diabetes will be missed unless an oral glucose tolerance test (OGTT) is performed. If there is any suspicion or other risk factor suggesting glucose intolerance, the OGTT should continue to be used pending the final WHO recommendation.
What are the new diagnostic criteria?
The new WHO criteria for diagnosis of diabetes mellitus and hyperglycaemia are shown in Box 1. The major change from the previous WHO recommendation3 is the lowering of the diagnostic level of fasting plasma glucose to ≥7.0 mmol/L, from the former level of ≥7.8 mmol/L. For whole blood, the proposed new level is ≥6.1 mmol/L, from the former ≥6.7 mmol/L.
This change is based primarily on cross-sectional studies demonstrating the presence of microvascular4 and macrovascular complications at these lower glucose concentrations. In addition, the 1985 WHO diagnostic criterion for diabetes based on fasting plasma glucose level (≥7.8 mmol/L) represents a greater degree of hyperglycaemia than the criterion based on plasma glucose level two hours after a 75g glucose load (≥11.1 mmol/L)6. A fasting plasma glucose level of ≥7 mmol/L accords more closely with this 2 h post-glucose level.
Recommendation: The ADA and the WHO committee are unanimous in adopting the changed diagnostic level, and the Australasian Working Party on Diagnostic Criteria recommends that healthcare providers in Australia and New Zealand should adopt it immediately.
Clinicians should note that the diagnostic criteria differ between clinical and epidemiological settings. In clinical practice, when symptoms are typical of diabetes, a single fasting plasma glucose level of ≥7.0 mmol/L or 2 h postglucose or casual postprandial plasma glucose level of ≥11.1 mmol/L suffices for diagnosis. If there are no symptoms, or symptoms are equivocal, at least one additional glucose measurement (preferably fasting) on a different day with a value in the diabetic range is necessary to confirm the diagnosis. Furthermore, severe hyperglycaemia detected under conditions of acute infective, traumatic, circulatory or other stress may be transitory and should not be regarded as diagnostic of diabetes. The situation should be reviewed when the primary condition has stabilised.
In epidemiological settings, for study of high-prevalence populations or selective screening of high-risk individuals, a single measure – the glucose-level 2 h post glucose load – will suffice to describe prevalence of impaired glucose tolerance (IGT).
Box 1: Values for diagnosis of diabetes mellitus and other categories of hyperglycaemia2
| Glucose concentration (mmol/L (mg/dL)) | ||||
|---|---|---|---|---|
| Whole blood | Plasma | |||
| Venous | Capillary | Venous | Capillary | |
| Diabetes mellitus fasting | ≥6.1 (≥110) | ≥5.1 (≥110) | ≥7.0 (≥126) | ≥7.0 (≥126) |
| or 2 h post-glucose load | ≥10.0 (≥180) | ≥11.1 (≥200) | ≥11.1 (≥200) | ≥12.2 (≥220) |
| or both Impaired glucose tolerance (IGT) Fasting (if measured) and 2 h post-glucose load) | <6.1 (<110) ≥6.7 (≥120) and <10.0 (<180) | <6.1 (<110) ≥7.8 (≥140) and <11.1 (<200) | <7.0 (<126) ≥7.8 (≥140) and <11.1 (<200) | <7.0 (<126) ≥8.9 (≥160) and <12.2 (<220) |
| Impaired fasting glycaemia (IFG) Fasting | ≥5.6 (≥100) and <6.1 (<110) | ≥5.6 (≥100) and <6.1 (<110) | ≥6.1 (≥110) and <7.0 (<126) | ≥6.1 (≥110) and <7.0 (<126) |
| 2 h post-glucose load (if measured) | <6.7 (120) | <7.8 (<140) | <7.8 (<140) | <8.9 (<160) |
For epidemiological or population screening purposes, the fasting or 2 h value after 75g oral glucose may be used alone. For clinical purposes, the diagnosis of diabetes should always be confirmed by repeating the test on another day, unless there is unequivocal hyperglycaemia with acute metabolic decompensation or obvious symptoms. Glucose concentrations should not be determined on serum unless red cells are immediately removed, otherwise glycolysis will result in an unpredictable underestimation of the true concentrations. It should be stressed that glucose preservatives do not totally prevent glycolysis. If whole blood is used, the sample should be kept at 0–4ºC or centrifuged immediately, or assayed immediately. Table reproduced with permission from Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional Report of a WHO Consultation. Diabet Med 1998; 15: 539-553. Copyright John Wiley & Sons Limited. | ||||
What about the oral glucose tolerance test?
Previously, the oral glucose tolerance test (OGTT) was recommended in people with a fasting plasma glucose level of 5.5–7.7 mmol/L or random plasma glucose level of 7.8–11.0 mmol/L. After a 75g glucose load, those with a 2 h plasma glucose level of <7.8 mmol/L were classified as normoglycaemic, of 7.8–11.0 mmol/L as having IGT and of ≥11.1 mmol/L as having diabetes.
The new diagnostic criteria proposed by the ADA and WHO differ in their recommendations on use of the OGTT. The ADA makes a strong recommendation that fasting plasma glucose level can be used on its own and that, in general, the OGTT need not be used1. The WHO group2 argues strongly for the retention of the OGTT and suggests using fasting plasma glucose level alone only when circumstances prevent the performance of the OGTT.
There are concerns that many people with a fasting plasma glucose level <7.0mmol/L will have manifestly abnormal results on the OGTT and are at risk of microvascular and macrovascular complications. This has major ramifications for the approach to diabetes screening, particularly when the Australian National Diabetes Strategy proposal7, launched in June 1998 by Dr Michael Wooldridge, then Federal Minister for Health and Aged Care, has early detection of type 2 diabetes as a key priority.
Recommendation: The Australasian Working Party on Diagnostic Criteria has major concerns about discontinuing use of the OGTT and recommends that a formal recommendation on its use in diabetes screening be withheld until the final WHO recommendation is made. However, in the interim, the OGTT should continue to be used.
Box 2: Aetiological classification of disorders of glycaemia*
Type 1 (β-cell destruction, usually leading to absolute insulin deficiency)
- Autoimmune
- Idiopathic
Type 2 (may range from predominantly insulin resistance with relative insulin deficiency to a predominantly secretory defect with or without insulin resistance)
Other specific types
- Genetic defects of β-cell function
- Genetic defects in insulin action
- Diseases of the exocrine pancreas
- Endocrinopathies
- Drug or chemical induced
- Infections
- Uncommon forms of immune-mediated diabetes
- Other genetic syndromes sometimes associated with diabetes
Gestational diabetes
Diabetes in pregnancy
The ADA has retained its old criteria for diagnosis of gestational diabetes1.These differ from those recommended by both WHO2 and the Australian Working Party on Diabetes in Pregnancy8 and are generally not recognised outside the United States. The new WHO statement retains the 1985 WHO recommendation that both IGT and diabetes should be classified as gestational diabetes. This is consistent with the recommendations of the Australasian Diabetes in Pregnancy Society, which recommended a diagnostic 2 h venous plasma glucose level on the OGTT of ≥8.0 mmol/L. In New Zealand, a cut-off level of ≥9.0 mmol/L has been applied8.
How has the classification of diabetes changed?
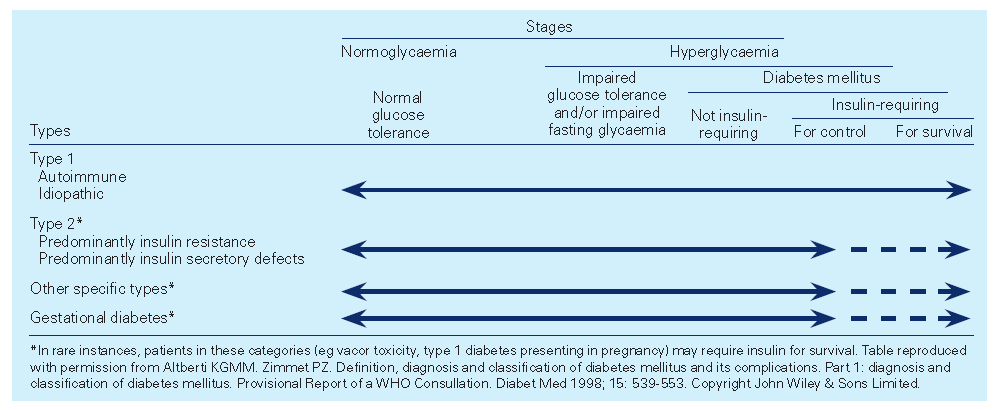
The proposed new classification encompasses both clinical stages and aetiological types of hyperglycaemia and is supported by numerous epidemiological studies. The classification by aetiological type (Box 2 above) results from new knowledge of the causes of hyperglycaemia, including diabetes. The terms insulin-dependent and non-insulin dependent diabetes (lDDM and NIDDM) are eliminated and the terms type 1 and type 2 diabetes retained. Other aetiological types, such as diabetes arising from genetic defects of β-cell function or insulin action, are grouped as ‘other specific types’, with gestational diabetes as a fourth category.
The proposed staging (Box 3 below) reflects the fact that any aetiological type of diabetes can pass or progress through several clinical phases (both asymptomatic and symptomatic) during its natural history. Moreover, individuals may move in either direction between stages.
Impaired glucose tolerance and impaired fasting glycaemia
Impaired glucose tolerance (IGT), a discrete class in the previous classification, is now categorised as a stage in the natural history of disordered carbohydrate metabolism. Individuals with IGT are at increased risk of cardiovascular disease, and not all will be identified by fasting glucose level.
Box 3:
In reducing the use of the OGTT, the ADA recommended a new category – impaired fasting glycaemia (IFG) – when fasting plasma glucose level is lower than that required to diagnose diabetes but higher than the reference range (<7.0 mmol/L but ≥6.1 mmol/L). Limited data on this category show that it increases both risk of progressing to diabetes9 and cardiovascular risk5. However, data are as yet insufficient to determine whether IFG has the same status as IGT as a risk factor for developing diabetes and cardiovascular disease and as strong an association with the metabolic syndrome (insulin resistance syndrome).
IFG can be diagnosed by fasting glucose level alone, but if 2 h glucose level is also measured, some individuals with IFG will have IGT and some may have diabetes. In addition, the number of people with OGTT results indicating diabetes but fasting plasma glucose level <7.0 mmol/L is unknown, but early data suggest there may be major variation across different populations10. A number of studies, including the DECODE initiative of the European Diabetes Epidemiology Group, have reported that individuals classified with IFG are not the same as the IGT group11-15. The European Group believes that, on available European evidence, the ADA decision to rely solely on fasting glucose level would be unwise.
Recommendation: The Australasian Working Party on Diagnostic Criteria recommends immediate adoption of the new classification. However, clinicians should be aware that some cases of diabetes will be missed unless an OGTT is performed. Thus, if there is any suspicion or other risk factor suggesting glucose intolerance, the working party continues to recommend use of an OGTT pending the final WHO recommendation.
References
- Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997; 20: 1183-1197.
- Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional Report of a WHO Consultation. Diabet Med 1998; 15: 539-553.
- World Health Organization. Diabetes mellitus. Report of a WHO study group. Technical report series 727. Geneva: WHO, 1985.
- McCance DR, Hanson RL, Charles MA, et al. Comparison of tests for glycated haemoglobin and fasting and two hour plasma glucose concentrations as diagnostic methods for diabetes. BMJ 1994; 308: 1323-1328.
- Charles MA, Balkau B, Vauzelle-Kervoeden F, et al. Revision of diagnostic criteria for diabetes [letter]. Lancet 1996; 348: 1657-1658.
- Finch CF, Zimmet PZ, Alberti KGMM. Determining diabetes prevalence: a rational basis for the use of fasting plasma glucose concentrations? Diabet Med 1990; 7: 603-610.
- Colagiuri S, Colagiuri R, Ward J. National diabetes strategy and implementation plan. Canberra: Diabetes Australia, 1998.
- Hoffman L, Nolan C, Wilson D, et al. Gestational diabetes mellitus -- management guidelines. The Australasian Diabetes in Pregnancy Society. Med J Aust 1998; 169: 93-97.
- Charles MA, Fontbonne A, Thibult N, et al. Risk factors for NIDDM in white population. Diabetes 1991; 40: 796-799.
- Keen H. Impact of new criteria for diabetes on pattern of disease. Lancet 1998; 352: 1000-1001.
- DECODE Study Group on behalf of the European Diabetes Epidemiology Study Group. Will new diagnostic criteria for diabetes mellitus change phenotype of patients with diabetes? Reanalysis of European epidemiological data. BMJ 1998; 317: 371-375.
- De Vegt F, Dekker JM, Stehouwer CDA, et al. The 1997 American Diabetes Association criteria versus the 1985 World Health Organization criteria for the diagnosis of abnormal glucose tolerance. Diabetes Care 1998; 21: 1686-1690.
- Harris MI, Eastman RC, Cowie CC, et al. Comparison of diabetes diagnostic categories in the US population according to 1997 American Diabetes Association and 1980-1985 World Health Organization diagnostic criteria. Diabetes Care 1997; 20: 1859-1862.
- Unwin N, Alberti KGMM, Bhopal R, et al. Comparison of the current WHO and new ADA criteria for the diagnosis of diabetes mellitus in three ethnic groups in the UK. Diabet Med 1998; 15: 554-557.
- Chang C-J, Wu J-S, Lu F-H, Lee H-L, et al. Fasting plasma glucose in screening for diabetes in the Taiwanese population. Diabetes Care 1998; 21: 1856-1860.
Updated 11 October 2021