Print PDF
Summary of the SIRA customer experience and health outcomes study
1. Introduction
The experience people have in interacting with a compensation scheme can significantly impact their recovery. In 2019, SIRA commissioned an independent study to measure customer experience and health outcomes in the compulsory third party (CTP) and workers compensation schemes.
This study went well beyond standard customer satisfaction tests to measure customer experience with insurers, trust in the schemes, perceptions of justice, return to work and other activities, and health and social outcomes.
The study also considered the extent to which insurers are delivering services in line with SIRA’s Customer Service Conduct Principles. The principles are:
- Be efficient and easy to engage
- Act fairly, with empathy and respect
- Resolve customer concerns quickly, respect customers’ time and be proactive
- Have systems in place to identity and address customer concerns
- Be accountable for actions and honest in interactions with customers
Where present, these principles support positive outcomes for people who make a claim for compensation. From 2020, all insurers operating across CTP, workers and home building compensation are required to attest to these principles and provide detailed information about how they intend to deliver on these principles in their business plans.
The results of this study are summarised below, and the full report is available on the SIRA website. Caution should be taken in comparing the results of the CTP and workers compensation schemes, given the differences in how these schemes operate and injury types and severity.
1.1. How the study worked
SIRA engaged the Social Research Centre (SRC) to undertake this study with people who have claims in the NSW CTP and workers compensation schemes and had dealings with an insurer between 1 April 2019 and 31 March 2020. The participants selected were representative of the general population of people making claims in the schemes.
A total of 893 people with CTP claims and 885 people with workers compensation claims participated in the baseline survey online or over the phone. The survey coincided with social distancing restrictions to limit community transmission of COVID-19. Where possible, questions were added to the survey to understand the impact of the pandemic.
This survey was the first phase of a larger program of work that will take place in 2021.
2. Key insights
This study has revealed key insights into the factors that influence a person’s recovery from injury and their experience within the CTP or workers compensation schemes.
Overall, certain groups of people tended to report poorer experience and outcomes – regardless of injury severity or scheme. This includes people who are in the schemes for longer, have symptoms of probable serious mental illness, or are experiencing moderate to severe pain.
People who had been in the compensation system for longer periods were more likely to report poor customer experience, a lesser sense of justice in the compensation process, lower trust in the scheme to get them better, and had poorer outcomes. This finding reinforced the importance of providing tailored early intervention to promote safe return to work and activities.
Similarly, the study reinforced the importance of early identification of poor mental health and providing easy access to treatment sooner. Mental health was reported as an issue across both schemes with one quarter of people with a CTP claim (25%) and one in five (19%) people with a workers compensation claim assessed as having a probable serious mental illness. People with poor mental health were more likely to report poorer results, including in relation to customer experience, trust, return to work and activities, and self-reported health and social outcomes.
Pain affected many people who participated in the survey and their outcomes. One in five (22%) people with a CTP claim reported moderate to extreme pain and discomfort and one in eight (12%) people with a workers compensation claim. People experiencing higher degrees of pain were more likely to have had a poor customer experience, have lower trust in the scheme, reduced perceptions of justice in the scheme, and there was a decreased likelihood of them having returned to work or other activities. The early identification of ongoing pain and early access to treatment could help to reduce pain and promote recovery and outcomes.
Generally, people with a CTP claim were found to be more impacted by their injury than people with a workers compensation claim reporting more pain and discomfort, anxiety and depression, social isolation, and they were less likely to have their ‘life back on track’. In workers compensation, people with a psychological injury claim were more likely to have worse outcomes and experience than those with a physical injury claim. On most measures there were few differences in experience and outcomes between insurers in both the CTP and workers compensation schemes.
This study has identified areas that SIRA and insurers can focus on to improve customer experience and outcomes. On the customer service front, the lowest scoring Customer Service Conduct Principle for both schemes related to insurers resolving a person’s concerns quickly. This presents a tangible focus for insurers moving forward. In terms of health outcomes, the early identification of probable mental illness and pain, as well as opportunities for safe return to work and activities, will facilitate improved recovery and experience.
3. Customer experience
The study measured insurers’ performance against SIRA’s Customer Service Conduct Principles by asking participants to agree or disagree with a series of statements about their customer experience with their insurer.
3.1. CTP
The percentage of people who agreed or strongly agreed with each statement mapped to the Customer Service Conduct Principles are provided at Figure 1.
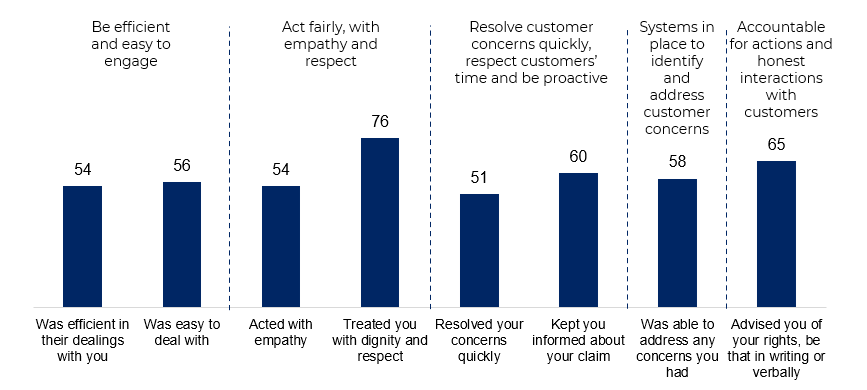
Three in five (59%) people with a CTP claim reported having a good customer service experience, while one quarter (23%) reported poor customer service. There were no significant differences in customer service experience based on injury severity or minor injury class. However, certain groups were more likely to report poor experience:
- People who were in the scheme for more than 130 days were more likely to report poor customer service (29%) compared to those who were in the scheme for less than 130 days (9%).
- People with severe or extreme pain and discomfort were more likely to report poor customer service (40%) compared to people with moderate (26%) and no, or slight, (13%) pain and discomfort.
- People who disagreed that they were able to easily access the medical treatment and services they needed were more likely to report having a poor customer service (57%) compared to people who agreed (11%).
- People who were assessed to have probable serious mental illness were more likely to report poor customer service (38%) compared to people who have no probable serious mental illness (17%).
- People who were legally represented were more likely to report poor customer service (32%) compared to claimants who were not legally represented (21%).
Performance against the principles were similar across CTP insurers. Although people with CTP claims with Allianz were more likely to agree they were kept informed about their claim (70%) compared to other insurers. People who were at fault were more likely than those who were not at fault to agree their insurer was easy to deal with, was efficient in their dealing, and acted with empathy.
3.2 Workers compensation
The study similarly measured the experience of people with a workers compensation claim against each one of the five Customer Service Conduct Principles. Figure 2 displays the percentage of people who agreed or strongly agreed with each statement.
Figure 2 Customer service conduct principles (% strongly agree / agree)

Two in three (68%) people with a workers compensation claim reported good customer service while one in seven (15%) reported having a poor customer service. Some groups were more likely to report a poor experience, including:
- People who were compensated for more than 130 days were more likely to report having poor customer service (34%) compared to those who were compensated for less than 130 days (14%).
- People with severe or extreme pain and discomfort were more likely to report having poor customer experience (38%) compared to people with moderate (20%) and no or slight pain and discomfort (9%).
- People who disagreed that they were able to easily access the medical treatment and services they needed were more likely to report having poor customer service (36%) compared to people who agreed (8%).
- Those with a mental illness claim were more likely to report having poor customer service (34%) compared to claimants with a physical injury claim (13%).
Performance against the principles was similar across all insurer types, with the exception that people with claims with the Nominal Insurer (managed by icare) had lower ratings for having their concerns resolved quickly (58%) and being kept informed about their claim (63%). This is compared to the results recorded for the Treasury Managed Fund (TMF) (66% and 72% respectively) and self and specialised insurers (71% and 76% respectively).
4. Trust
Participants were asked about the extent to which they trust the CTP and workers compensation schemes to help them get back to work or work and their usual activities.
4.1. CTP
Half (53%) of people with a CTP claim agreed that they trust the scheme to help them get back to work or their usual activities. Certain groups were more likely to trust the scheme, including people who were compensated for lesser periods, in no or slight pain and discomfort, had a low risk of poor recovery, and those who were not legally represented.
This study found a strong correlation between customer experience and trust. People who have low (66%) or medium (26%) trust in the scheme were more likely to report poor customer service compared to those who have high trust (5%).
Those who did not trust the CTP scheme to get them back to work or their usual activity were asked an open-ended question to suggest one change to the scheme that would increase their trust. The most common suggestion was to increase benefits, treatments or services (17%), followed by improving communication, contact or follow-up (14%), and better consideration or assessment of injury or condition (12%).
4.2. Workers compensation
Three in five (60%) people with a workers compensation claim agreed they trust the scheme to help them get back to work. Some people were more likely to trust the scheme, including those who have been compensated for lesser periods, those with a physical injury claim compared to a mental illness claim, those who had no probable serious mental illness, and those that agreed that they were able to easily access the medical treatment and services they needed. People who had returned to work or expected to recover within the next few months or sooner were also more likely to trust the scheme.
Similar to the CTP scheme, the workers compensation scheme results found a strong correlation between customer experience and trust. People who had low (36%) or medium (18%) trust in the scheme were more likely to report having poor customer service compared to people who reported high trust (2%) in the scheme.
People who did not trust the workers compensation scheme to get them back to work were also asked to suggest one change to the scheme that would increase their trust. The most common response related to improving communication, contact or follow-up (22%). The second most common response related to better consideration or assessment of injury or condition (11%), and increased benefits, treatments or services (11%).
5. Perceived justice
Participants were asked questions about their perceptions of justice or fairness in their compensation experience in the CTP and workers compensation scheme. This is an important measure as research shows that the higher the perceived injustice, the poorer the recovery outcomes.
5.1. CTP
Participants were asked questions across four dimensions of perceived justice. The highest performing dimension of perceived justice related to the insurer treating the person in a polite manner and with dignity and respect (interpersonal justice). The lowest performing dimension related to perceptions of whether the amount of benefits paid were fair and acceptable (distributive justice).
Certain groups of people with a CTP claim recorded lower rates of perceived justice across all four dimensions. This includes people who were not at fault, in the scheme for more than 130 days, had a higher risk of poor recovery, or were legally represented.
Performance was similar across insurer types, with the exception that people insured by Allianz had higher ratings for the provision of information (informational justice) than those insured by NRMA and QBE.
5.2. Workers compensation
Similar to the CTP scheme, people in the workers compensation scheme rated interpersonal justice as the highest performing dimension of perceived justice, and the lowest performing dimension as distributive justice. Overall, people with a workers compensation claim reported higher ratings across all four dimensions than people with a CTP claim.
In the workers compensation scheme, people who were compensated for more than 130 days, have a mental illness claim, have not returned to work, have moderate or worse pain, have a probable serious mental illness, or have an expectation that their recovery will take more than a year, have lower rates of perceived justice.
There was no difference in the ratings of perceived justice between the different workers compensation insurer types.
6. Return to work and other activities
The study considered participant’s experience returning to work and their everyday life activities after an injury on the roads or at work. Return to work and other activities are key objectives of the CTP legislation and return to work is a key objective of the workers compensation legislation.
6.1. CTP
Two in three (68%) people with a CTP claim had returned to their main activity at some time since their injury. People who were assessed as having a minor injury or not legally represented were more likely to have returned to their main activity.
The study considered the returned to work rate based on the National Return to Work Survey measure as the proportion of people who had returned to work for any period of time since their first day off work. Three quarters (75%) of people with a CTP claim who were working at the time of their injury had returned to work at some time since their injury. There were no significant differences in the returned to work rate between people from the different insurers.
Poorer return to work performance was recorded by people with a non-minor injury, moderate or severe injuries, probable serious mental illness, in higher degrees of pain and discomfort, or by those that were legally represented.
This study also used the current return to work rate which is the proportion of people working at the time of the survey. Excluding those who were retired, three-fifths (60%) of people with a CTP claim were working at the time of the survey. Of those that were not working at the time of the survey, nearly half (47%) indicated that they were unable to work while one in five (21%) were unemployed as shown in Figure 3.
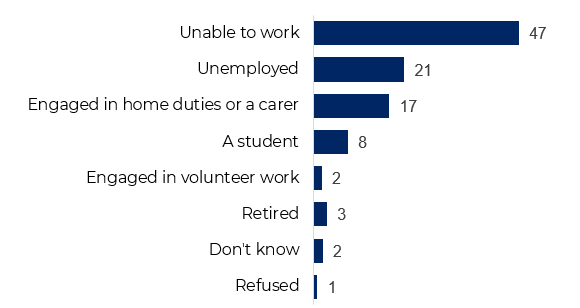
One-fifth (22%) of people who were not working or retired and identified that their reason for not working was not related to their injury, identified that their reason for not working was related to the COVID-19 pandemic.
Overall, two in five CTP participants reported being unable to participate in regular activities such as work or study (41%), do simple activities such as standing, reaching, sitting or walking (38%), normal social activities (38%) or normal household activities (38%). Participants who rated their customer service from the insurer as poor were more likely to have difficulty with all activities compared to those who rated their customer service higher. People with severe injuries had significantly more difficulty with work or study, normal social activities and simple actions such as standing, reaching, sitting or walking.
6.2. Workers compensation
Using the returned to work rate based on the National Return to Work Survey, four in five (84%) people with a workers compensation claim had returned to work at some time since their work-related injury or illness.
Certain groups of people with a workers compensation claim recorded poorer return to work performance. This includes people who were compensated for longer periods of time, in higher degrees of pain and discomfort, reported poor customer service from their insurer, had a mental illness claim, had a probable mental illness, or had lower trust in the scheme.
In terms of the current return to work rate, four in five (79%) people with a workers compensation claim were working at the time of the survey. People who were insured by TMF or self and specialised insurers (90% and 86% respectively) were more likely to be currently working.
Of the people not working at the time of the survey, one half (48%) indicated that they were unable to work while nearly two-fifths (37%) were unemployed, as shown in Figure 4. Those with a mental illness claim were more likely to be unable to work (75%) compared to those with a physical injury claim (40%).
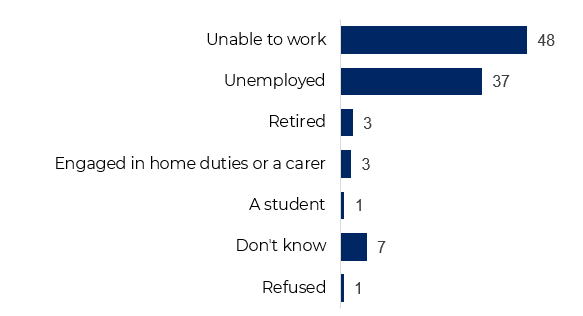
Where people were not working and identified that the reason was not related to their injury, one-third (30%) contributed their reason for not working to the COVID-19 pandemic.
Over one quarter of people with a workers compensation claim reported being unable to participate in regular activities such as work or study (29%), normal social activities (26%) or normal household activities (25%). People who had been compensated for longer periods or had not returned to work since their injury or illness were more likely to report difficulty on all activities.
7. Health outcomes
Participants were asked about their access to and the effectiveness of healthcare services in the CTP and workers compensation schemes. They were also asked about their current health and well-being, the status of their recovery, and what could be done to assist it.
7.1. CTP
The majority of people with a CTP claim (91%) rated their overall health prior to their injury as good, very good, or excellent. Only half (51%) rated their overall health at the time of the survey as good to excellent. People who received good customer service from their insurer, agreed that they were able to easily access the medical treatment and services that they needed, who were at fault, and with injuries assessed as minor, were more likely to rate their current health as good to excellent.
Two in three (64%) CTP participants agreed that they were able to easily access the medical treatment and services that they needed. One in two (50%) people with a CTP claim reported that the COVID-19 pandemic had made it much more, or slightly more difficult to access medical treatment and services.
One in four (25%) people with a CTP claim were assessed to have a probable serious mental illness using the Kessler Psychological Distress 6 scale. People whose injury was not minor, had medium or low trust in the scheme, believe they will not recover at all or only make a partial recovery, in severe or extreme pain and discomfort, or legally represented were more likely to have a probable mental illness.
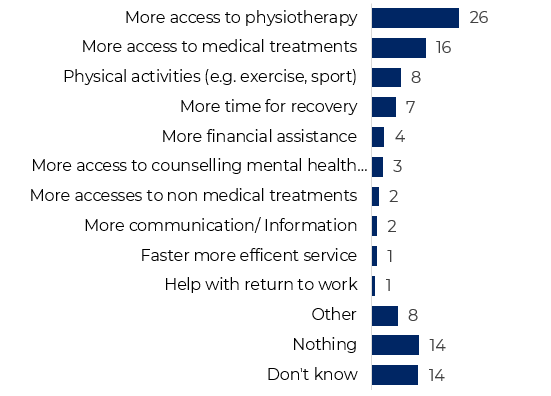
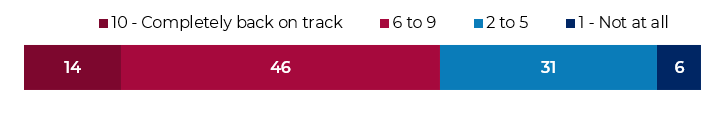
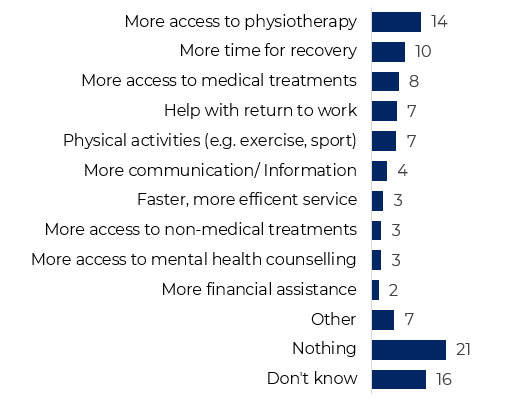
Only two in five (41%) people with a CTP claim believed they would make a complete or nearly complete recovery, and one in ten (11%) believed they would not recover at all People who expected to make a further recovery identified that more access to physiotherapy (25%) and medical treatments (16%) would most assist their recovery, as shown in Figure 5.
Figure 5 What could be done to improve recovery (%)
Participants were asked about the extent to which they felt they have been able to get their life ‘back on track’ following an injury on the roads on a scale from one to ten, where one means ‘not at all’ and ten means ‘completely back on track’. Three in five (60%) people with a CTP claim rated the extent to which their life is back on track as six or more (see Figure 6). People who reported a good customer experience (72%) compared to a poor customer experience (35%) or were at fault (74%) compared to not at fault (56%) were more likely to rate the extent to which their life is back on track as six or more. There were no significant differences in this rating between the different CTP insurers.
Figure 6 Extent to which life is back on track (%)
7.2. Workers compensation
Nearly all (94%) of people with a workers compensation claim reported their overall health prior to their injury as good, very good, or excellent. Two thirds (68%) reported their overall health at the time of the survey as good to excellent. People who had high trust in the scheme (78%) and a physical injury claim (71%) compared to a mental illness claim (41%) were more likely to rate their current health as good to excellent. People with claims with the TMF were also more likely to rate their current health as good to excellent (74%) compared to those who are with the Nominal Insurer (65%).
Two-thirds (65%) of workers compensation participants agreed that they were able to easily access the medical treatment and services that they needed. When asked about the impact of COVID-19 on access to medical treatment and services, one in three (35%) people with a workers compensation claim reported that the situation had made it much more or slightly more difficult.
One in five (19%) people with a workers compensation claim were assessed to have probable serious mental illness using the Kessler Psychological Distress 6 scale. People with medium or low trust in the scheme or were compensated for a longer duration were more likely to have a probable mental illness.
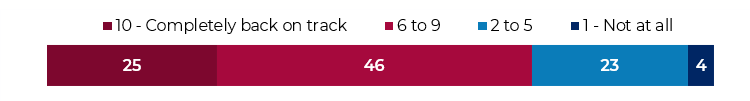
Two in three (63%) people with a workers compensation claim believed they would make a complete or nearly complete recovery, while one in twenty (7%) believed they would not recover at all. Those who expected to make a recovery were asked to describe what they thought could be done to improve their recovery. One in five (21%) indicated nothing could be done while one in six (16%) said they did not know what could be done to improve their recovery, as shown in Figure 7.
Figure 7 What could be done to improve recovery (%)
The majority (71%) of people with a workers compensation claim reported the extent to which their life was back on track as six or more on a scale of one to ten (see Figure 8). Those with a physical injury claim were more likely to rate the extent to which their life was back on track as six or more (74%) compared to those with a mental illness claim (42%). There were no significant differences in this rating between the different insurer types.
Figure 8 Extent to which life is back on track (%)
8. Conclusion
This study has provided key insights into the customer experience, trust, perceived justice, return to work and other activities, and health outcomes of the CTP and workers compensation schemes. Overall, people with a CTP claim were more likely to be affected by their injury, had poorer outcomes, and reported a greater impact from the COVID-19 pandemic. However, these results have been affected by differences in the mechanism of injury and injury severity across the schemes.
Certain groups of people across both schemes tended to report poorer experience and outcomes. This includes people who are in the schemes for longer, have mental illness claims, symptoms of probable serious mental illness, or are experiencing pain. While good customer experience does not directly lead to recovery, this study has shown that it is an important foundation to people achieving optimal health and social outcomes.
SRC is now in the process of conducting its first repeat survey as part of the larger program of work measuring customer experience and outcomes in the CTP and workers compensation schemes. SIRA will publish these results and will continue to undertake customer experience research at regular intervals, using the results to inform scheme design, support recovery and return to work and activity, and regulatory supervision activities.
