Workers compensation system explanatory note October 2019
About this month’s system performance results
Effectiveness
Further deterioration in RTW rates but at a slower rate than previously observed
The rate at which workers return to work (RTW) following a work-related injury is a key measure of system effectiveness. RTW rate is measured using work status codes at 4 weeks, 13 weeks and 26 weeks.
As shown in the following table the RTW rate at 4 weeks has dropped by 5.72 percentage points since October 2018. That is, as a proportion of all workers who had an absence from work following a workrelated injury in the 12 months to October 2019, the percentage who had returned to work by the end of the fourth week after the date of injury was 5.72 percentage points fewer than for the 12 months to October 2018. Similarly, the RTW rate at 13 weeks deteriorated by 6.11 percentage points; and the rate at 26 weeks deteriorated by 6.19 percentage points.
Compared to the 12 months between September 2018 and September 2019 (set out in the previous monthly dashboard published by SIRA), there has been a slower deterioration of RTW rates at 4, 13 and 26 weeks. However, the 52-weeks rate for the same periods shows a higher level of deterioration.
Table 1 – Comparison of the year on year RTW performance
RTW rates (Weeks) | October 2018 | October 2019 | Percentage points change between October 2018 and 2019 | Comparison percentage points change between September 2018 and 2019 | |
|---|---|---|---|---|---|
4 | 67.97% | 62.25% | - 5.72 | -6.80 | |
13 | 81.66% | 76.56% | -6.11 | -6.50 | |
26 | 87.63% | 81.44% | - 6.19 | -7.00 | |
52 | 91.32% | 86.57% | - 4.75 | -3.95 | |
Efficiency
Increase in payments to and for workers and decrease in insurer expense rate
As at the 30 June 2019 average insurer operating costs and expenses as a proportion of all scheme expenditure reduced from 30% to 28% for the 2018/19 financial year. Payments directly to workers and for workers each increased by 1%. This is the lowest expenses rate and the highest rate of payments to and for workers in the 4 years that SIRA has monitored expenditure in this way. In dollar terms, the 1% increases in payments to and for workers equates to an additional $180M in payments to workers and an additional $105M for services to support workers’ recovery.
Viability
Increases in aggregate and per claim weekly compensation payments
Trends in claim numbers and per-claim costs can significantly impact system stability and viability. Month-on-month and year-on-year claim numbers, per-claim costs and active claim numbers are key measures in this regard. Active claims are those for which liability has been accepted (or where a liability decision is pending) and that have had a payment within the last 3 months.
In October 2019 the number of active claims across the system was 100,222, up from 92,314 in October 2018. This increase is only marginally attributable to an increase in claims volumes: the number of reported claims in October 2019 was only 262 more than the number reported in September 2019, and for the NI average number of reported claims per month remains relatively stable at approximately 6,000.
The increase in active claims suggests an increase in average claim duration. This is supported by the continuing deterioration in RTW rates, which results in more workers being in receipt of weekly payments of compensation at any given time. This is a trend across all insurer types but is most pronounced for the
NI.
The average duration (in days) for which a worker received weekly payments in the first 6 months following an injury was 23.3 days in 2013/14. This average has steadily increased to 27.8 days in 2018/19. Continuation of this trend is a significant risk to the long-term viability of the scheme.
Continued increases in weekly payments can be observed across the system, with $228M more in payments in the 12 months to October 2019 compared to the 12 months ending October 2018. The NI’s total weekly payments increased by $170M between these two 12-month periods, an increase of 24%. This is significantly higher than the increase for other insurer types (self-insurers 4%; TMF 15% and specialised insurers 18%).
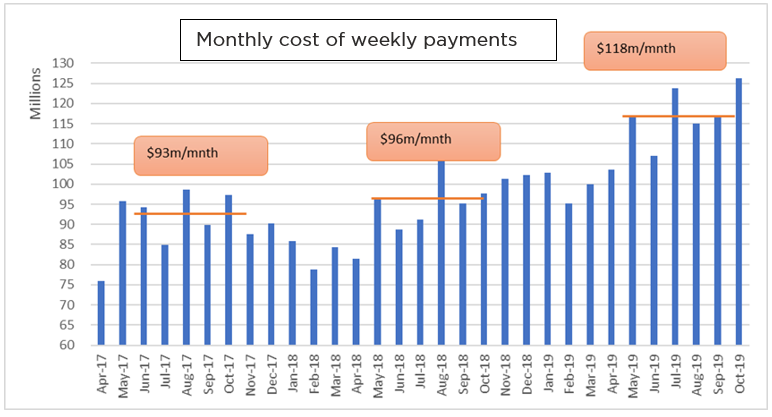
The upward trend in weekly payments is now accelerating. The graph below shows that the average total cost of weekly payments per month during the 6 months ending October 2019 was 23% higher than average for the 6 months ending October 2018. This is a much sharper increase than for the 6 months
ending October 2017.
Graph 1 – Monthly cost of weekly payments
Continuing increase in payments for medical and related treatment
Medical costs have been increasing at above-inflation rates for several years and this trend shows no sign of abating. In aggregate, medical costs for the 12 months to October 2019 increased by 9% ($76M) compared to the 12 months to October 2018. This includes:
- 6% ($8M) increase in private hospital expenditure, which constituted 13% of total medical payments
- 11% ($7M) decrease public hospital expenditure, which constituted 5% of total medical payments
- increase in payments for allied health services, including
- 12% ($9M) increase in payments for physiotherapy services
- 32% ($6M) increase in payments for psychological services
- 23% ($6M) increase in payments for exercise physiologists
- 18% increase ($6M) increase in payments for 'other therapies and treatments, which includes pain management, case co-ordination services, external facilities fees and occupational therapists
- 15% ($16M) increase in payments for home care services and aids
- 11% ($8M) increase in payments for GP services
- 9% ($6M) increase in payments for diagnostic services and therapeutic procedures
Increases in lumpsum payments and worker travel and accommodation expenses
Lumpsum payments of compensation for permanent impairment and pain and suffering increased by 24% ($33M) for the 12 months to October 2019 compared to the 12 months to October 2018. Over the same period, payments for injured worker travel and accommodation increase by 14% ($6M).
Customer Experience
Declining numbers of enquiries and complaints
SIRA and WIRO received 2,538 enquiries and 818 complaints about the NSW Workers Compensation system in October 2019. This is fewer than for the previous month.
Dispute rate remains steady
The dispute rate as a proportion of active claims remains relatively stable at approximately 0.6%.
Feedback on these reports
This monthly dashboard includes several enhancements; feedback and comments on the dashboard
reports are welcome.
Please email us at: [email protected].
Feedback on these reports
This monthly dashboard includes several enhancements; feedback and comments on the dashboard reports are welcome.
Please email us at:[email protected].
About the data in this report
The dashboard reports data from multiple sources to provide insights into the system performance of the NSW Workers Compensation system. The report is structured on SIRA’s performance framework, reporting on performance measures of effectiveness, efficiency, viability, affordability, customer experience, and equity.
SIRA as the regulator of the NSW Workers Compensation system monitors the system regularly and defines parameters of the system in alignment with the glossary and descriptions in the attached table. From time to time there are discussions and presentations from providers within the Workers Compensation ecosystem including insurers, medical and allied health providers etc about these metrics. One such discussion currently within the landscape is that of the definition of active claims.
Methodology, data notes and data sources
The data presented in this report are derived from monthly claims submission data, annual declarations provided to SIRA from NSW workers compensation insurers, the Workers Compensation Commission and the Workers Compensation Independent Review Office.
The financial and cost information in this report is presented in original dollar values with no indexation applied. Costs in the workers compensation scheme are subject to a variety of potential inflationary factors including wage and salary rates, medical fee schedules, statutory benefit indexation and general price inflation. As there is no single index which adjusts for all potential factors, costs have been shown in their original dollar values for simplicity.
The premium value used for the Nominal Insurer in this report is calculated as total premium payable net of GST and levies, such as the dust disease levy and mine safety levy. Premium for self-insurers is deemed premium, calculated as wages covered multiplied by the premium rate applicable for the appropriate industry class. Premium for Government self insurers (TMF) is the value of the deposit contributions made by each member agency. Premium for specialised insurers is the gross written premium, net of GST and levies, such as the dust disease levy and mine safety levy.
Insurers regularly update claims data based on the progression of a claim. This may result in changing claim details month on month.
Additional efficiency information
System costs – weekly payments
SIRA in the previous reports offered additional data on the Workers Compensation system performance. These additional data sets have been included at the end of the dashboard report to show the following.
- The cost to the system of weekly benefits paid per month.
- The number of workers receiving weekly benefits per month.
- The average duration of weekly benefits paid to workers in the first 6 months following their injury.
- The percentage of workers who have returned to work (including those who received medical benefit only with no lost time), at 4, 13 and 26-week intervals.
As indicated above, analysis of this additional information reveals an upward trend for both the costs associated with deteriorating RTW rates and the number of workers receiving weekly benefits.
The “Claim payment development” chart has again been developed for the August 2019 dashboard. The chart shows claim payments by accident year. That is, comparing payments of accidents occurring in the 2019/20 financial year with the prior accident period at the same stage of development. This chart allows for like for like comparisons across financial years and presented in original dollar values with no indexation applied.
Data source information
Effectiveness
Reported claims
Standard terms | Definitions |
|---|---|
Active claim | An active claim is defined as a claim with any payment within a three-month period. |
Reportable claims | A reportable claim for workers compensation or work injury damages is a claim that a person has made or is entitled to make under the Workplace Injury Management and Workers Compensation Act 1998. Claims become reportable once they meet certain liability conditions and/or have received payments. For example, the injury or illness may be physical or psychological and employment must be a substantial contributing factor to injury, except for those claims made by police officers, paramedics, fire fighters, volunteer bush fire fighters and emergency and rescue services volunteers for injuries suffered during journeys to and from work or place of volunteering. Reportable claims include claims from workers whose employer is uninsured. Where a split by insurer segment is shown, claims of uninsured employers are included with the Nominal Insurer segment. Exclusions Reportable claims exclude administration error claims, claims closed with zero gross incurred cost, claims shared between two or more workers compensation agents/insurers and the agent/insurer is not responsible for the management of the claims, and claims with payments only for recoveries, vocational programs or invalid payment classification numbers. Reportable claims also exclude claims for:
|
Records submitted | All records received from insurers across NSW. This data excludes administration errors. |
Lost time | Monthly average, over the last 12 months, of workers who had lost time. |
Claim types
Standard terms | Definitions |
|---|---|
Claim types | Claims reported in the reporting month, classified as either 'psychological injuries' for mental disorder claims or 'all non-psychological injuries' for all other claims |
Psychological Injury (ies) | The range of psychological conditions for which workers compensation may be paid, including post-traumatic stress disorder, anxiety/stress disorder, clinical depression and short-term shock from exposure to disturbing circumstances. |
Return to work
Standard terms | Definitions |
|---|---|
Return to work rate | The Return to work (RTW) rate is the percentage of workers who have been off work as a result of their employment-related injury/disease and have returned to work at different points in time from the date the claim was reported (i.e. 4, 13 and 26 weeks for the SIRA Stats report). RTW rates are calculated monthly for the last 13 months up to the date of data. The cohort for each RTW measure is based on claims reported in a 12-month period, with a lag to allow for claim development (i.e., the lag for the 4-week measure is 28 days; the lag for the 13-week measure is 91 days; and the lag for the 26-week measure is 182 days). Calculation method for 4-week measure for November 2018 is given below as an example:
RTW Rate=b/a multiplied by 100 SIRA identified data quality issues with the accuracy and completeness of data submitted by the Nominal Insurer (NI). The data revealed a significant deterioration in the NI’s RTW performance. To address the data quality and potential performance concerns with the NI, SIRA carried out a Data Quality audit in December 2018 and commenced a Compliance and Performance Review in February 2019. SIRA published the Review and associated documents in December 2019 and the reports are available here. |
Claims by body locations
Standard terms | Definitions |
|---|---|
Bodily location of injury / disease | The bodily location of injury/disease classification is intended to identify the part of the body affected by the most serious injury or disease. Only 1-digit bodily location of injury is used. |
Mechanism of incident | Mechanism of incident applies to claims entered into the insurer’s system on or after 1 July 2011 and uses the Type of Occurrence Classification System, 3rd Edition (Revision 1) Australian Safety and Compensation Council, Canberra 2008. |
Nature of injury /disease | The nature of injury/disease classification is intended to identify the type of hurt or harm that occurred to the worker. The hurt or harm could be physical or psychological. |
Efficiency and viability
Claim payment types
Standard terms | Definitions |
|---|---|
Payment data | Payments made are based on the transaction date. Payments with payment date within the reporting period. |
Common Law (WID) payments | Lump sum payments for damages and common law legal expenses incurred by the worker or agent/insurer, pursuant to Part 5 Common Law remedies, Sections 149 to 151AD, Workers Compensation Act 1987 and Section 318H, Workplace Injury Management and Workers Compensation Act 1998. WID stands for ‘Work injury damages’ and this term is used interchangeably with ‘common law’ |
Commutations | The actual gross amount of commutation awarded or agreed upon for the claim. This refers to compensation where a commutation of the claimant's right to compensation has been made by the insurer. The up-front lump sum payment is made to an injured worker in place of continuing weekly compensation award and future medical and hospital expenses, pursuant to Part 3, Division 9 Commutation of compensation, Sections 87D to 87K, Workers Compensation Act 1987. |
Death payments | Funeral expenses, weekly payments for dependent children and lump sum payments paid to the dependants or estate of the deceased worker, pursuant to the Workers Compensation Act 1987 No. 70 and Workers Compensation (Dust Diseases) Act 1942. |
Injury Financial year | The financial year in which the injury occurred. Starts on 1st July and ends on 30th June the following year |
Investigation payments | Payments for insurer and worker investigation expenses, pursuant to Sections 9A, 11A and 44A, Workers Compensation Act 1987 and Sections 45A, 330, 331, 337, 339 and 376, Workplace Injury Management and Workers Compensation Act 1998. |
Number of workers receiving weekly benefits per month | Number of injured workers receiving weekly benefit payments excluding Section 39 claimants that exited the system until June 2018. |
Other payments | Payments for repair to or replacement of artificial limbs and clothing because of the workplace injury, amounts paid to any approved interpreter service for English language assistance to the claimant, transport and maintenance expenses related to travel costs incurred by the worker and shared claim payments. |
Lump sum (S66 and S67) | Section 66 payments are lump sum payments for the permanent loss or impairment of a specified bodily function or limb, or severe facial or bodily disfigurement, including interest, pursuant to Section 66, Workers Compensation Act 1987 and as provided by the Table of Disabilities or whole person impairment (WPI) and Ready-reckoner of Benefits Payable. |
Rehabilitation payments | Payments for a single workplace rehabilitation service, a suite of services provided to assist a worker to RTW with the same employer, a suite of services provided to assist a worker to RTW with a different employer or travel costs of the workplace rehabilitation provider in the delivery of rehabilitation services, pursuant to Sections 59, 60 and 63A, Workers Compensation Act 1987. Rehabilitation treatment includes the initial rehabilitation assessment, workplace assessment, advice concerning job modification, and rehabilitation counselling. Rehabilitation treatment does not include medical, hospital, physiotherapy or chiropractic treatment. |
Weekly benefits paid per month | Weekly benefit payments paid to injured workers for incapacity excluding Section 39 claimants that exited the system until June 2018. |
Weekly payments | Weekly payments paid to an injured worker for incapacity. |
Compliance and Enforcement
Standard terms | Definitions |
|---|---|
Compliance promotion and assurance | The count of individual cases within the reporting period that SIRA has undertaken a compliance assurance activity. These include proactive compliance assurance activities and assessments of referred cases of alleged non-compliance. |
Escalated enforcement and fraud | The count of individual cases within the reporting period that SIRA has undertaken an assessment or investigation of alleged fraud or escalated matters consideration for an enforcement response. |
Penalties and prosecutions | SIRA enforcement actions undertaken with the reporting period, including the issuing of infringement notices, recoveries of avoided premiums and prosecutions. |
Benefits paid to and for workers as a percentage of total claims expenditure
Standard terms | Definitions |
|---|---|
Benefits paid directly to workers | Includes weekly payments, common law, s66, death benefits, commutations and miscellaneous payments. |
Benefits paid for services for workers recovery and return to work | Includes medical costs, allied health services e.g. rehabilitation payments to support claimants. |
Insurer expenses | Includes administration and operating expenses, regulatory costs, investigations, insurer’s legal fees etc. |
Affordability
Insurance affordability
Standard terms | Definitions |
|---|---|
Affordability | A reflection of the cost of premiums for workers compensation as a percentage of the reported NSW wages bill. The premium value used for the Nominal Insurer is calculated as total premium payable net of GST and levies, such as the dust disease levy and mine safety levy. The premium for self-insurers is deemed premium, calculated as wages covered multiplied by the premium rate applicable for the appropriate industry class. The premium for Government self insurers (TMF) is the value of the deposit contributions made by each member agency. The premium for specialised insurers is the gross written premium, net of GST and levies, such as the dust disease levy and mine safety levy. Premium information is updated annually. |
Customer experience and equity
Enquires, complaints, and perceptions of equity
Standard terms | Definitions |
|---|---|
Enquiry | An enquiry is defined as a customer call regarding information or advice that is general in nature. The number of enquiries received in the reporting period. |
Complaint data | Is derived verbatim from reports from customers. Whilst some data cleansing processes are undertaken by SIRA the reporting is verbatim from customers and may from time to time reference an incorrect insurer and/or insurer type. The number of complaints received in the reporting period. |
Level 1 complaints | A level 1 complaint is defined as a complaint received by frontline staff where an insurer is notified (via email) by the Customer Advisory Service on behalf of the complainant. |
Level 2 complaints | A level 2 complaint is an escalation of an unresolved level 1 complaint. |
Justice | The Perceived Justice of the Compensation Process series of measures is a scale used to measure workers perceptions of fairness of their workers compensation experience. The Abridged Return to Work Outcomes Survey: NSW Workers Compensation System (October 2019) included three dimensions (procedural justice, information justice, and interpersonal justice).
For each dimension, respondents were asked to rate their level of agreement with a series of statements using a 5-point Likert type rating scale. A higher score denotes a higher level of agreement, or a higher perceived sense of justice / fairness. |
Complaints theme
The top 5 complaint themes may vary month by month.
Standard terms | Definitions |
|---|---|
Complaint types reported to SIRA | Complaints received in the reporting period, split by complaint type. |
Case Management Practice: Insurer conduct / behaviour | Where there is a general enquiry or complaint about insurer behaviour or conduct e.g. poor communication, or the way the claim is managed by the insurer. |
Communication | Clarity of insurer information. When an insurer has made a request of a worker, and the worker doesn’t understand the request, or why the request was made. |
Customer Service: Behaviour | Where the customer is dissatisfied with the behaviour of any stakeholder involved in management of the claim, e.g. insurer or provider. |
External Decision: WCC Determination | Enquiry or complaint about a determination not being applied or complied with, e.g. consent orders not being paid |
Independent Medical Examination: Guidelines | Where there is an enquiry or complaint regarding Independent Medical Examination (IME) guidelines, that is, where a worker believes the insurer is not adhering to the guidelines e.g. not being given 10 days’ notice to attend an appointment. |
Licensed Insurers: Claims Lodgement | Any enquiry about how to lodge a claim. |
Medical: Liability | Process /communication to determine liability including any reference to reasonably necessary treatment and s59A entitlement periods e.g. medical entitlements have not been approved and the worker believes they have not received the relevant communication. |
Medical: Payments | Delay in payments to the provider or reimbursement to worker. |
Medical: Timeframes | A worker has made a claim for medical treatment, but the request has not been responded to within legislated timeframes i.e. a decision has not been made within 21 days. |
Weekly payments: Payments | Enquiry or complaint about delays in payments to the worker or reimbursement to the employer |
Weekly payments: Calculations | Enquiry or complaint about the calculation of pre-injury average weekly earnings e.g. the worker not receiving correspondence detailing the calculation. Enquiry or complaint from exempt workers about their current weekly wage rate or average weekly earnings. |
Weekly payments: Liability timeframes | Enquiry or complaint about the relevant timeframes to determine liability, e.g. when a worker has lodged a claim form, but a decision has not been made within 21 days. |
Dispute rate
Standard terms | Definitions |
|---|---|
Disputes lodged/finalised | Disputes lodged/finalised in the reporting period. |
Dispute rate | The number of disputes lodged (internal review, merit review, procedural review and workers compensation commission disputes) in the reporting month divided by the number of active claims as at the end of the same reporting month. |
Active claim | An active claim is a claim that has had any payment activity in the three months as at the end of the same reporting month. |
Internal review | An internal review is a review of the work capacity decision by someone within the insurer other than the person who made the decision. The source of information for the number of internal reviews is the insurers’ submission data to SIRA. |
Merit review | A merit review is undertaken by an independent decision maker at SIRA who conducts a merit review of the insurer’s work capacity decision and outlines findings and recommendations. These reviews are binding on the insurers. |
Procedural review | A review by the Workers Compensation Independent Review Office (WIRO) can follow a merit review by SIRA and is a procedural review of the insurer’s work capacity decision. |
Workers compensation commission | The WCC is an independent statutory tribunal that has jurisdiction to deal with a broad range of disputes. Most of the compensation dispute applications are Applications to Resolve a Dispute (Form 2) and may involve claims for more than one type of compensation benefit, including weekly payments, medical and related treatment, and permanent impairment. |