Workers compensation regulation bulletin - Issue 86
What’s driving escalating healthcare costs in the NSW Workers Compensation scheme?
Healthcare costs account for more than $1 billion each year in personal injury insurance schemes in New South Wales. In recent years, the costs have grown faster in the NSW workers compensation scheme than in Medicare and private health insurance.
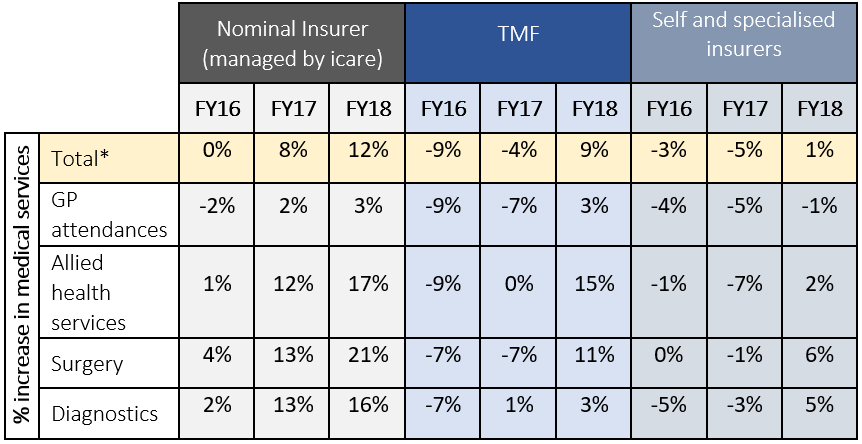
SIRA Chief Executive Carmel Donnelly said, “While health care fees in SIRA-regulated schemes are in some cases higher than other states, this has been the case for many years. The recent changes in healthcare expenditure relate primarily to increases in service utilisation – not medical fees.”
To better understand and address the drivers of escalating healthcare costs and service utilisation, SIRA is leading a Review of Regulatory requirements for health care arrangements in the NSW Workers Compensation and CTP schemes. Under the review, SIRA is considering the full range of healthcare arrangements in the Workers Compensation and CTP schemes, including fees, clinical quality, data and reporting, monitoring and compliance and regulation.
“Since 2016 we’ve seen increases in healthcare utilisation among some insurers, without a corresponding improvement in return to work outcomes. The review is not about reducing expenditure or the treatment available to injured people. SIRA’s objective is to make sure that every dollar spent delivers quality and value and optimises recovery,” Ms Donnelly said
Submissions and themes
SIRA received 53 submissions to the review, 43 of which will be published in the coming weeks. SIRA also held a series of stakeholder briefings. A final report will be published in the second half of 2020. In the meantime, SIRA is working with insurers to tighten controls around treatment payments and approvals and with the medical community on value-based care and fees models.
The submissions include the following themes:
- the importance of strengthening insurer controls over health provider billing
- the need for insurers to more closely scrutinise proposed treatments
- the importance of early treatment in medical costs across the life of a claim
- the need for insurers to better identify injured people at risk of not returning to work
- a link between adversarial claims and disputes and non-medically appropriate care
- an increase in degenerative, rather than traumatic injuries
- health providers seeing patients for long periods without clinical justification
- the need for increased data publication
- consideration of outcome-based fee models
- the need for SIRA to set clinical frameworks and standards
Changes in service utilisation
Increased service utilisation accounts for around 61 percent of the total growth in workers compensation medical expenditure between 2016/17 and 2017/18. By comparison, increases in the unit cost (i.e. the fee paid per service) accounts for around 5 percent of the total growth in healthcare expenditure. Other contributing factors include growth in active claims.