Regulatory requirements for workplace rehabilitation service provision in NSW personal injury schemes
1. Introduction to consultation paper
Purpose of the consultation paper
The purpose of this discussion paper is to seek input from stakeholders on the NSW policy and framework underpinning the approval, engagement and performance of workplace rehabilitation providers. The aim of the review is to inform the future workplace rehabilitation service provision and regulatory framework to achieve:
- improved recovery and return to work performance for people in NSW personal injury schemes;
- a value and outcome-based policy framework; and
- a sustainable provider market, ensuring availability of services.
For the purposes of this paper workplace rehabilitation (WR) refers to the breadth of services, supports and interventions designed to assist people with an injury or illness to achieve their recovery and return to work goals.
Why is SIRA doing this?
The State Insurance Regulatory Authority (SIRA) is responsible for the regulatory functions in relation to workers compensation (WC) insurance and motor accidents compulsory third party (CTP) insurance. SIRA is responsible for developing the policy and guidance regarding return to work (RTW) and measuring how the schemes are performing in terms of RTW. SIRA play an important role in identifying what works well and areas for improvement across the system.
There are four key drivers which are particularly significant in the context of the review:
- Return to work rates following workplace injury are decreasing in WC; medical costs associated with injuries are increasing; and referrals to workplace rehabilitation are decreasing. In the time of COVID-19, the need to keep people job-ready and job-fit when return to work is not available has also emerged as a priority.
- WR services need to be outcome focussed to deliver value-based care within the personal injury schemes as outlined in the recently published Health Outcomes Framework.
- Reforms to the CTP scheme that better support people injured on our roads were introduced less than three years ago and opportunity exists to harness synergies and improve recovery and RTW goals and outcomes regardless of the scheme.
- The environment in which we operate is continually evolving. Best practice in workplace rehabilitation, emerging challenges, and system and service opportunities are all considerations in the sustainability of the schemes.
2. Background and context
Current legislative and policy landscape
The Workplace Injury Management and Workers Compensation Act 1998 sets out clear expectations and objectives for WR. All NSW employers must have a RTW program in place within 12 months of starting a business. It must be consistent with the insurer’s injury management program and any guidelines issued by SIRA. A RTW program is the foundation supporting an organisational culture of recovery at work and is a written description of the steps an employer will take when a worker sustains an injury or illness that necessitates them taking time off work.
In 2017 the NSW Government reformed the CTP scheme to better support people injured on our roads and to reduce the cost of Green Slips for vehicle owners (Motor Accident Injuries Act 2017 ( MAI Act).
The new CTP scheme started 1 December 2017 and introduced entitlements for all injured road users, regardless of fault, to weekly income payments (if time off work is needed), medical and treatment expenses and commercial attendant care (for help needed around the home).
A large proportion of those injured on our roads participate in the workforce and delays in payment of expenses, such as lost income, can create significant financial hardship and stress at a time when people need to recover. This can impact on a person’s ability to return to work and lead a normal life again.
While there is currently no approval framework for WR under the CTP scheme the new MAI Act focuses on early and appropriate treatment and care to maximise return to work or other activities.
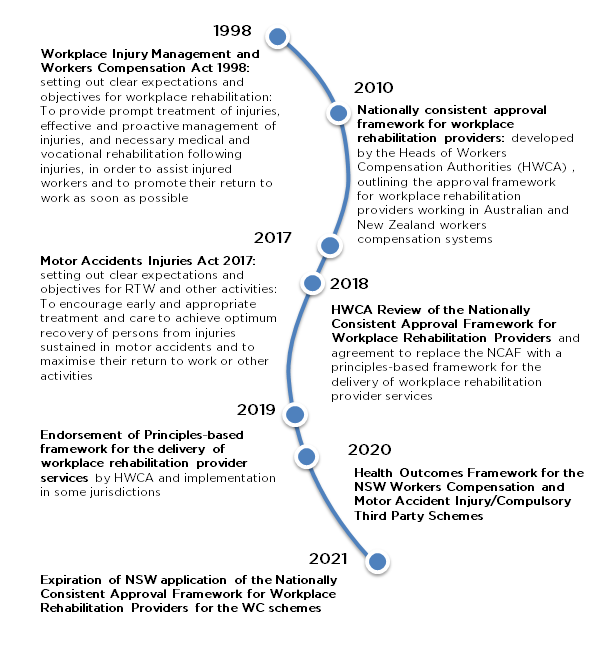
Figure 1: relevant milestones in the evolution of regulatory requirements for workplace rehabilitation in NSW
Nationally consistent approvals framework for WR providers in the workers compensation scheme
In 2010 the Heads of Workers Compensation Authorities (HWCA), agreed the Nationally consistent approvals framework1 (NCAF) to ensure minimum standards for workplace rehabilitation providers working in Australian and New Zealand workers compensation systems were consistently met for the delivery of services to workers and employers.
The NSW Supplement to the Guide: Nationally consistent approval framework for workplace rehabilitation providers2 was developed to supplement the NCAF and outlines specific requirements for providers approved to deliver workplace rehabilitation services in NSW.
Workplace rehabilitation providers operating in NSW are currently approved by SIRA. Part 7 of the Workers Compensation Regulation 2016 legislates that SIRA can approve workplace rehabilitation providers to operate in the workers compensation system. There are currently 100 approved workplace rehabilitation providers. In contrast, workplace rehabilitation providers are undefined in the CTP legislation so that mechanisms for approval are not available. At the same time, supporting optimal recovery following an injury or illness includes supporting return to work, irrespective of the scheme in which someone participates. There is an opportunity to leverage standards and approval mechanisms across schemes in NSW.
Principles of practice for WR providers3
In 2018, the HWCA agreed to replace the NCAF and in September 2019 they endorsed a principles-based framework for the delivery of workplace rehabilitation provider services. These principles have been developed to support WR providers in the delivery of services to workers with a compensable injury. The Principles recognise the importance of work in recovery and are intended to:
- guide WR providers in delivering workplace rehabilitation services to a worker
- inform the WR provider approval and management frameworks of workers’ compensation authorities
- support the vision of the National Return to Work Strategy 2020-2030
- complement the Clinical Framework for the delivery of health services.
In NSW, the current NCAF continues to be in place until June 2021 and pending the outcome of this review.
WR providers
Providers in the field of workplace rehabilitation have the qualifications, experience and expertise appropriate to provide independent services in accordance with the following definition based on the National Occupational Health and Safety Commission (NOHSC; 1995):
Workplace rehabilitation is a managed process involving timely intervention with appropriate and adequate services based on assessed need, and which is aimed at maintaining injured or ill employees in, or returning them to, suitable employment.
There is no single regulatory body with oversight of workplace rehabilitation services. Individual rehabilitation consultants may need to be members of the Australian Health Practitioner Regulation Agency or have accreditation or membership with a professional association. This membership is specific to their background profession and not specific to the service/s they provide as a rehabilitation consultant for a workplace rehabilitation provider. SIRA has established processes to facilitate administrative and regulatory efficiencies and ensure no overlap or duplication with other regulatory frameworks or requirements.
Current RTW performance
The following information is based on the available data at the time of writing this consultation paper. It is not intended to be exhaustive but provide a brief overview.
RTW is an important and measurable component of physical and mental health, wellbeing and recovery. Current data on RTW and related scheme performance provides valuable insight into current challenges and opportunities for future improvement.
In recent years trends in RTW show:
- a decline in RTW performance in NSW WC
- increasing recognition of the importance of RTW goals for CTP participants, with approximately two thirds of those injured on the roads being active in the workforce
- since the CTP scheme is relatively new to RTW measurement trends in performance are not yet evident.
At the same time, trends in related scheme performance measures show:
- the proportion of WC claims receiving WR services is decreasing
- the spend on WR services in WC is decreasing. In 2018-19 FY the WC scheme spent $158million on WR providers, equating to 15% of the total medical and related health spend. This is a reduction in spend on WR providers from 19% for 2017/18
- the overall healthcare costs in the WC system are increasing, with workers receiving more care from more providers.
Moving towards value and outcomes
An overarching objective of SIRA is to make sure that every healthcare dollar spent delivers quality and value and optimises recovery and outcomes for injured people.
The Health Outcomes Framework for the NSW Workers Compensation and Motor Accident Injury/Compulsory Third Party Schemes4 sets a new vision for healthcare within the personal injury schemes which SIRA regulates. This vision drives how success is viewed and will be measured in respect of the key health outcomes. The vision is:
"The WC and CTP schemes regulated by SIRA deliver value-based care to injured persons covered by the schemes.”
Crucial to attaining this vision is optimising a worker’s recovery and capacity to work. It is envisaged that the Health Outcomes Framework will help to improve the understanding of the health outcomes injured people experience in our schemes. Better data on injured people’s health status and outcomes is essential to enabling SIRA and scheme participants to determine whether the schemes are delivering value-based healthcare.
Question
In the current landscape, are there aspects of the WC or CTP schemes that should be extended to the other scheme to optimise WR service provision?
3. WR in NSW personal injury schemes
Best practice in WR
A recent review commissioned by SIRA revealed there is strong evidence that the best practice for WR programs which consistently resulted in improved work-related outcomes, are the ones incorporating multiple components, specifically incorporating health care, service coordination and workplace/employer components. Programs that were intervened early and are individually tailored to meet worker’s needs were particularly successful.5
The most effective WR programs included these three components:
- Health care components: consist of a wide range of programs and support to promote health and wellbeing for workers who have experienced injury or mental health conditions, such as depression.
- Service coordination components: aim to better coordinate the delivery of and access to, services to assist return to work within and involving the workplace. These components facilitate interactions between workers, employers, health care providers, insurance agencies and other stakeholders.
- Workplace/employer components: incorporate worksite adjustments or accommodations offered to better facilitate the worker’s return to work process.
Multi-component WR programs, incorporating health care, service coordination and workplace components, not only addressed workers’ health care needs but also facilitated understanding, expectation and co-operation between workers, health care practitioners and employers, in the process of improving return to work outcomes.
Health care for injured workers is important but health care alone has little impact on work outcomes. The evidence shows that effective and cost-effective WR programs are those that also target employers to implement proactive approaches to injury and illness, along with temporary provision of work modification and accommodation tailored to workers’ needs. In best practice WR programs, it is imperative to target workers and employers to coordinate health care and workplace accommodation activities.
While there is strong evidence of best practice components for WR programs there are also challenges to overcome in service delivery and quality, the changing nature of work and the workplace and in the local system context for personal injury schemes.
Emerging challenges
The COVID-19 pandemic is presenting new and evolving challenges such as:
- safe operations in providing face-to-face WR support
- increased transition to remote/online WR support
- new challenges and complexity in supporting injured people RTW in a safe and timely manner
- increased job losses, or interruption to work, impacting injured workers’ RTW goals
- the need to ensure that people with injuries, regardless of the status of their employment, remain connected to the world of work
- the importance of keeping injured people, employers and treating health practitioners engaged, connected and supported during challenging COVID-19 circumstances.
Earlier this year SIRA engaged with NSW industry stakeholders to ensure continuity of WR services during the ‘COVID-19 lockdown’ as many programs aimed at job-readiness and RTW moved to virtual or home-based service provision within the limitations of social isolation.
The challenges that COVID-19 presents have emphasised the importance of programs to achieve and maintain job readiness and stay connected to the world of work. These programs must have the specific goal of keeping the worker:
- engaged in their recovery through the development of a recovery at/return to work plan
- connected with their employer, where possible, and their community
- work ready so when they are able to, they can recover at or return to work.
Psychological injury claims are a growing challenge in Australia. Psychological injury claims are increasing and RTW outcomes for these injured workers are poorer. While primary psychological injuries only account for 7.5 per cent of all workers compensation claims6, these claims typically result in a significantly longer time off work than other types of serious claims. The 26 week return to work rate for people with a psychological injury claim is 53%, compared to 85% for people with physical injury claims7. There is an important role for WR in supporting these workers in best practice programs of support, however specialist capabilities for working with psychological injury are not currently differentiated in the market. Similarly, injured workers with brain injury (BI) require specialised WR support and will make up a key group of CTP claimants.
Health outcomes and recovery oriented care: WR goals must reflect optimal outcomes for individuals and avoid simplistic metrics that can underpin perverse incentives and disadvantage groups that rely on the schemes to optimise their recovery, e.g. injured workers with more specialised WR support needs (such as ABI and psychological claims).
The breadth of services, supports and interventions continues to expand to meet our evolving understanding of need as it relates to whole-of-person recovery rather than only work specific task/fitness/readiness, e.g. the increasing body of evidence regarding the importance of the psychosocial context of injuries and work absence; increasing use of peer support and career connection services.
System and service delivery opportunities
It is the aim of personal injury schemes in NSW to provide appropriate and timely access to WR support and opportunities for increased focus are outlined below.
Identifying and meeting individual WR needs – it is fundamental to a) identify and understand the individual needs of an injured person at the beginning of their journey, and b) ensure appropriate referral to support services based on need. Current best practice suggests that targeting people who are at higher risk of delayed RTW is the optimal strategy for achieving appropriate referral for WR support. While approaches to identifying those who would benefit from WR programs are still being established5, there are a range of screening tools and frameworks that can be used by insurers and providers.
Timely access to WR – timely interventions are key to the success of WR programs as they raise employment propensity, improve income stability both during and after the intervention period and reduce the risk of transitioning to permanent disability benefits schemes. While the average time to first WR payment in NSW WC has been reducing, there remains considerable room for improvement.
Service delivery quality assurance – there is a need for the breadth of WR services, interventions and supports in the system to have appropriate governance arrangements to ensure quality and consistency and promote a culture of innovation and improvement.
Access and equity – successful WR programs are individually tailored to meet the needs of the worker’s health problem/s, work-related issues and include the worker, their employers, treating health care professionals and other stakeholders; working together to a common goal. Ongoing challenges exist with access and availability of WR services for: Aboriginal; culturally and linguistically diverse (CALD) workers; those with lower health literacy; those of mature age; and those in regional and remote areas of NSW.
Outcomes – we have an opportunity to ensure services are focused on outcomes and that we focus on the right metrics to encourage this. This includes measurement of timely, safe and durable RTW, effectiveness of work connected service provision and provider performance.
Optimal interaction between case management and workplace rehabilitation. Service coordination is a key component of best practice in WR. It includes coordinating the delivery of, and access to services and support to involve the workplace to assist workers’ recovery and RTW. Case management includes case administration, benefits payments and coordination and approval of services and support. There continue to be challenges in achieving an optimal balance between some functions of case management and WR. These have been evident as the system has undergone transformative change in recent years and in some cases has resulted in increased duplication of case coordination functions and reduced WR focus on core services leading to poorer performance.
WR workforce challenges - the WR workforce includes a diverse range of professionals with varying capabilities, training and approvals to provide WR in NSW. There are challenges with inclusion of some professions as approved WR providers; with appropriate use of non-approved providers; consistency and quality of services; and appropriate fee structures to support a sustainable market.
Questions
Do we have the breadth of WR services, interventions and supports required for optimal recovery and RTW outcomes for injured people in NSW?
What would be the best approach to building capability in WR service provision?
How do we support WR service provision to achieve optimal outcomes?
How do we promote best practice and continued innovation in WR service provision in NSW?
4. The full potential of WR to optimise recovery and RTW in personal injury schemes
Health and social care worldwide is changing with rising health costs, new technologies, and consumers taking a more active role in their healthcare and choices about what matters to them. Value based health and social care enables us to adapt to these changes, to improve health outcomes and experiences and ensure the sustainability of the personal injury system.
Traditional funding and payment models drive volume rather than value because they reward activity not outcomes. These pivotal levers in the systems do not align with providing outcome-focused and value-based care. Shifting from volume to value requires a new way of doing business. Outcomes based measurement and reward embeds value-based purchasing and delivery. It is well-recognised in health and social care that measurement of process is important to understand program fidelity in implementation; however, payment on achievement of outcomes is critical to focus providers on purposeful process in the interests of outcomes rather than process being an end in itself.
Value-based and outcomes focussed health and social care provides a new direction for thinking about how we organise systems to best serve the customers’ needs. Customer centricity is central to achieving this vision. The evidence suggests that a customer centric approach focussed on early and timely interventions, individually tailored programs, and multi component programs including healthcare, workplace and service coordination is most effective in optimising health and recovery.
The definition of value-based care used in the Health Outcomes Framework is consistent with national and international principles and definitions. These focus on the four essentials of value known as the Quadruple Aim for delivery of care that improves:
- health outcomes that matter to those receiving care
- experiences of receiving care
- experiences of providing care
- effectiveness and efficiency of care.
The Health Outcomes Framework sets out the outcomes to be achieved for the care that is provided to participants in the schemes. The framework supports the achievement of the vision for health and social care by specifying how success will be defined and measured. Better data on injured people’s health status and outcomes is essential to enabling SIRA and scheme participants to determine whether the schemes are delivering value-based care.
Questions
How do we most effectively measure outcomes associated with WR?
How can we drive value – as articulated in the SIRA Health Outcomes Framework - for WR in NSW personal injury schemes?
5. The policy framework to realise the potential of WR in NSW
SIRA is responsible for the regulatory functions in relation to WC insurance and motor accidents CTP insurance. SIRA is responsible for ensuring that the related key public policy outcomes are achieved in relation to service delivery to injured people, affordability, and the effective management and sustainability of these insurance schemes.
The opportunity to review the current policy framework to improve outcomes for workers and other stakeholders in the system now exists. The goal of a future policy framework is to support effective service delivery of workplace rehabilitation in NSW personal injury schemes, to address current and emerging challenges and to improve system and personal outcomes.
Elements of a policy framework
The elements of any policy framework must be both broad as well as enabling flexibility and innovation. The elements should ensure that WR providers can contribute to improving recovery and return to work outcomes. The following policy elements are identified as potential inputs to a revised future policy framework in NSW:
Guiding principles: are the fundamental building blocks to guide policy development and implementation; inform WR providers approval and management frameworks; and guide evidence based, best practice service delivery.
The current Principles of Practice for Workplace Rehabilitation Providers support WR providers in the delivery of services to workers with a compensable injury. The principles recognise the importance of good work in recovery with research suggesting that good work is not only good for health and wellbeing but that long-term absence from work has a negative impact on physical and mental health8. Furthermore, the principles guide the expectations for quality service delivery.
Governance – accountability and responsibility. Dynamic, effective and responsive governance is central to a policy framework. In this context, core elements of accountability and responsibility include:
- establishing standards to deliver high quality workplace rehabilitation
- creating and maintaining an efficient and effective system for the approval, implementation and monitoring of WR providers
- facilitating measurement and ensuring compliance of provider performance against established conditions and desired outcomes.
Measuring progress and outcomes: enables a view over time that reflects the extent to which the outcomes have been or are being achieved. Defined outcomes support planning, evaluation and response activities enabling improved transparency and accountability, and contribute to more effective supervision and regulation.
The Health Outcomes Framework reflects the desired changes in the status, functioning and experience of injured persons and other elements of the WC and CTP healthcare ecosystem resulting from interactions within the schemes.
Finally, any policy framework should consider best practice along with current and emerging trends to achieve positive return to work and health outcomes for individuals and minimise any economic, health and social consequences of work-related injury or illness.
Question
What elements does a policy framework need to drive quality, innovation, capability and outcomes in WR in NSW?
1.The Guide: Nationally consistent approval framework for workplace rehabilitation providers www.hwca.org.au.
5. John Walsh Centre for Rehabilitation Research, 2020. Best practice for vocational programs Rapid review, Prof Ian Cameron
6. SIRA data 2019 calendar year
7. SIRA data 2018/2019 financial year
8. Australasian Faculty of Occupational & Environmental Medicine - Royal Australasian College of Physicians: Australian Consensus Statement on the Health Benefits of Work (2017).
