Print PDF
Motor Accident Guidelines
General introduction to the Motor Accident Guidelines
You can also download the PDF version of this document.
This is version 9.2 of the Motor Accident Guidelines. See previous versions and their effective dates below.
Parts of the Guidelines
Parts of the Guidelines
The Guidelines are divided into the following parts:
- Part 1: Premium determination
- Part 2: Market practice
- Part 3: Business plans
- Part 4: Claims
- Part 5: Threshold injury (Soft tissue & threshold psychological or psychiatric injuries)
- Part 6: Permanent impairment
- Part 7: Dispute resolution
- Part 8: Health practitioners authorised to give evidence in court and other dispute resolution proceedings
- Glossary
Publication note
These Guidelines are published by the State Insurance Regulatory Authority (the Authority).
Part of the NSW Department of Customer Service, the Authority is constituted under the State Insurance and Care Governance Act 2015 and is responsible for regulating workers compensation insurance, motor accident compulsory third-party (CTP) insurance and home building compensation insurance in NSW.
Commencement and application of the Guidelines
These Guidelines commence on 10 November 2023 and replace the Motor Accident Guidelines version 9.1, except for claims arising from motor accidents before 1 April 2023.
For claims arising from motor accidents occurring before 1 April 2023:
- Clauses 4.36, 4.37, 4.40 and 4.41 of these Guidelines do not apply, and
- Clauses 4.36, 4.39, 4.40, 4.41, 5.1(c), 5.15 and 5.16 in the Motor Accident Guidelines version 9 continue to apply.
Unless otherwise indicated to the contrary for a particular part or clause, these Guidelines:
- apply to all claims and applications made before or after the commencement of these Guidelines, and
- do not invalidate a step previously taken under Version 9 of the Motor Accident Guidelines.
The Guidelines apply until the Authority amends, revokes or replaces them in whole or in part.
Existing Guidelines made under the Motor Accidents Compensation Act 1999 and continue to have effect in relation to the scheme established under that Act which applies to motor accidents from 5 October 1999 to 30 November 2017.
Legislative framework
The Motor Accident Injuries Act 2017 (the Act) establishes a scheme of CTP insurance and the provision of benefits and support relating to the death of, or injury to, people injured as a consequence of motor accidents in New South Wales (NSW) on or after 1 December 2017.
Injury or death to a person as a result of a motor accident occurring before 1 December 2017 is governed by either the Motor Accidents Act 1988 or the Motor Accidents Compensation Act 1999 and the relevant Regulation and Guidelines made under the Motor Accidents Compensation Act 1999.
The objects of the Act, as described in section 1.3 are to:
- encourage early and appropriate treatment and care to achieve optimum recovery of persons from injuries sustained in motor accidents and to maximise their return to work or other activities
- provide early and ongoing financial support for persons injured in motor accidents
- continue to make third-party bodily insurance compulsory for all owners of motor vehicles registered in NSW
- keep premiums for third-party policies affordable by ensuring that profits achieved by insurers do not exceed the amount that is sufficient to underwrite the relevant risk and by limiting benefits payable for threshold injuries
- promote competition and innovation in the setting of premiums for third-party policies, and provide the Authority with a role to ensure the sustainability and affordability of the compulsory third-party insurance scheme and fair market practices
- deter fraud in connection with CTP insurance
- encourage the early resolution of motor accident claims and the quick, cost‑effective and just resolution of disputes
- ensure the collection and use of data to facilitate the effective management of the CTP insurance scheme.
The Motor Accident Injuries Regulation 2017 (the Regulation) contains provisions that supplement the operation of the Act in a number of key areas.
Guideline-making power
These Guidelines are made under section 10.2 of the Act, which enables the Authority to issue Motor Accident Guidelines with respect to any matter that is authorised or required by the Act.
Provisions in each individual Part of the Guidelines are also made under relevant specific guidelines making powers in the Act.
Interpretation of the Guidelines
These Guidelines should be read with relevant provisions of the Act and the Regulation, and interpreted and applied in a manner that supports the objects of the Act in section 1.3 of the Act.
A reference in these Guidelines to a number of days is a reference to a number of calendar days, unless otherwise specified.
Purpose of the Guidelines
The Guidelines support the administration of the CTP scheme and the objects of the Act and the operation of the Regulation by establishing clear processes and procedures, scheme objectives and compliance requirements. In particular, the Guidelines describe and clarify expectations that apply to respective stakeholders in the scheme. It is a condition of an Insurers licence to comply with relevant parts of the Guidelines that apply to them.
Application of the Guidelines
Relevant parts of the Guidelines apply to key customers of the scheme, including:
- vehicle owners and policyholders
- injured persons and other claimants.
Relevant parts of the Guidelines also apply to key scheme stakeholders and service providers, including:
- insurers
- health practitioners
- lawyers and other representatives
- staff of the Authority
- courts and other dispute resolution bodies.
Under the Act, including section 10.7, it is a condition of an insurer’s licence that it complies with relevant provisions of the Guidelines.
Compliance with the Guidelines
The Authority will monitor and review compliance with the Guidelines. Compliance and enforcement will be undertaken in accordance with the Authority’s Compliance and Enforcement Policy (July 2017).
Part 1 of the Motor Accident Guidelines: Premium determination
Determination of insurance premiums for third-party policies
Introduction
1.1 These Guidelines provide mechanisms for the regulation of insurance premiums matters under Part 2, Division 2.3 and clause 2 of Schedule 4 of the Motor Accident Injuries Act 2017 (NSW) (the Act). They are issued by the State Insurance Regulatory Authority (the Authority).
Commencement and revocation of previous Guidelines
1.2 This Part of the Guidelines is effective for policies that come into effect on or after 15 January 2024. For policies that come into effect from 15 January 2023 to 14 January 2024, Part 1 of the Motor Accident Guidelines v 9.1 continue to apply.
Definitions
1.3 In this Part of the Guidelines, bonus malus refers to a percentage decrease or increase in the insurer’s base premium using approved risk-rating factors. Bonus has the same meaning as discount and malus has the same meaning as loading in this Part.
Guiding principles
1.4 The primary objects under section 1.3 of the Act relating to a premium framework are to:
(a) promote competition and innovation in the setting of premiums
(b) ensure the sustainability and affordability of the scheme and fair market practices
(c) keep premiums affordable by ensuring that the profits realised by insurers do not exceed the amount that is sufficient to underwrite the relevant risk.
1.5 To promote competition and innovation by insurers, the Authority allows risk-based pricing, but this must be done within limits in order to keep premiums affordable. The premium framework recognises that this liability scheme, which is compulsory and privately underwritten, blends risk-based and community-rated approaches to assist with the object of affordability.
1.6 Filed premiums must be adequate and not excessive (under section 2.22(1)(a) of the Act). The Authority will closely scrutinise filed premiums against the objects of the Act and against any range of premiums for transitional policies it has determined under clause 2(3)(c) of Schedule 4 of the Act.
1.7 In aligning with the competition and innovation objects, the Authority recognises that insurers will pursue their own particular business objectives that will be reflected as an integral part of each insurer’s pricing strategy. On this basis, technical (actuarial) pricing will not be considered in isolation and an explanation by insurers is encouraged for non-technical pricing considerations, including:
(a) business plans and short, medium and long-term growth strategies
(b) response to pricing by competitors
(c) market segmentation and distribution strategies
(d) innovation and efficiencies in their business model.
1.8 The Authority will take into account the objects of the Act by considering both qualitative and quantitative explanations when reviewing insurer filings.
Premium filing process
Filing requirements
1.9 A premium filing under Division 2.3 of the Act must be provided in soft copy and must include:
(a) covering letter
(b) filing report
(c) the Authority’s motor accident filing template
(d) any other additional information reasonably required by the Authority.
Covering letter
1.10 The premium filing covering letter must be signed by the NSW CTP product executive or equivalent office holder of the licenced insurer and include:
(a) the proposed commencement date for the premium and the period nominated by the insurer for the Authority to reject the premium (cannot be less than six weeks)
(b) an executive summary of the filing
(c) the overall average premium
(d) any significant changes to the most recent business plan approved by the Authority impacting competitive strategies or market positioning
(e) any significant rating factor changes
(f) any changes in bonus malus levels
(g) implementation plan detailing how the insurer will meet the proposed commencement date
(h) an outline of the policyholder impact analysis.
Filing report
1.11 Every filing report must include:
(a) a summary of the changes proposed and any changes in business strategy
(b) explanation of each filing assumption change made since the previous filing
(c) completed motor accident filing template commentary and analysis of the estimated effects on the portfolio composition as described in ‘Portfolio analysis’ section below
(d) an analysis of the change in average premium and base premium against the previous filing
(e) signed endorsement of the filing from the NSW CTP Product Executive or equivalent office holder
(f) any other information requested by the Authority.
1.12 Nothing further is required to be included in the filing report if all the following conditions are met:
(a) the expiry date of the filing lodged is within 12 months from the commencement date of the most recent filing approved by the Authority
(b) the change in average premium excluding GST and the Fund levy reported in Schedule 1C of the Authority’s motor accident filing template is less than 4% when compared to the most recent filing approved by the Authority
(c) the change in Base Premium Rate (Class 1 Metro) excluding GST, Fund levy reported in Schedule 1C of the Authority’s motor accident filing template is less than 4% when compared to the most recent filing approved by the Authority.
1.13 If any of the above conditions are not met, the filing report must also include:
(a) how the proposed insurance premiums (excluding the Fund levy and GST, and assuming no policyholders are entitled to any input tax credit (ITC)) were determined by the insurer
(b) the factors and assumptions considered in determining the premiums, how those factors were derived, and any variation relative to the Authority's independent actuary’s costing assumptions (Schedule 1E, provided by insurers in the form specified in Table 1.3), taking into account the insurer’s business mix by class and region and other (claims experience related) factors against those of the industry
(c) an explanation of the non-technical pricing factors where applicable
(d) how the insurer assessed projected future frequency of:
- claims for the industry (inclusive of nominal defendant claims, and by subdivision as set out in Schedule 1E)
- claims for the insurer (by subdivision as set out in Schedule 1E and disclosing the treatment of shared claims and nominal defendant claims).
(e) how the insurer assessed projected future average claim size of:
- claims for the industry (inclusive of nominal defendant claims, and by subdivision as set out in Schedule 1E)
- claims for the insurer (by subdivision as set out in Schedule 1E and including the estimated net effects of shared and nominal defendant claims).
(f) a summary of claim frequency and average claim size (in current values), and resulting cost per policy, by claim component (including nominal defendant), allowing for sharing and net of ITCs, should be included in the filing report. This should reconcile to item 1c in Schedule 1C for claim frequency and indicate the adjustment to claim sizes required to reconcile to item 2b in Schedule 1C.
(g) economic and investment assumptions, including:
- assumed future rates of wage and price inflation
- full yield curve adopted and the single equivalent rate of discount
- assumed future claim payment pattern for the underwriting period covered by the filing specifying whether the basis is current values, inflated or discounted.
(h) superimposed inflation (SI) assumption, including:
- assumed future rates of SI
- disclosure of the single equivalent rate of SI where different rates have been used for different claim segments and/or different rates of SI have been adopted in future years
- an explanation of the approach taken in setting the SI assumptions.
(i) insurer expenses, including average past actual and expected future rates and amounts of:
- acquisition and policy-handling expenses (excluding commission or other remuneration) associated with third-party policies with appropriate explanation provided and a description of the methodology used to allocate overhead expenses
- commission or other remuneration expenses (for the purpose of determination of insurance premium the filed percentage per policy cannot exceed 5% of the proposed insurance premium)
- claims-handling expenses, including an explanation of what is included in this item, and a description of the methodology used to allocate overhead expenses
- net cost of reinsurance.
(j) disclosure of the above past and expected future expenses on a total pool basis as well as on a cost per policy basis for acquisition and policy expenses, and on a per claim basis for claims-handling expenses (for clarity, claims-handling cost per claim expected to arise during the period covered by the filing)
(k) the expense assumptions used and an explanation of how they relate to the above information
(l) proposed profit margin: the percentage of gross insurance premiums intended to be retained as profit, before tax
(m) adjustments to insurer premium to obtain the class 1 metro base premium by disclosing a full explanation of the calculation of the:
- ratio of the class 1 metro premium to the average premium
- average bonus malus factor: commentary should be included where the filed average bonus malus factor varies from the average implied by the expected future number and mix of insured vehicles by vehicle class and rating region at each bonus malus level (as provided in the portfolio analysis)
(n) details of how the percentage loading applied to the nil ITC premium rates to obtain the ITC premium rates was determined
(o) details of how the short-term loading parameters A, B, X and Y were determined
(p) a comparison with the previous filing of the filed average premium and the actual average premium received by the insurer, together with an explanation of the allowance made for non-annual policies in calculating these average amounts, including:
- how the assumptions regarding future experience in the current premium filing differ from the corresponding assumptions in the previous filing by the insurer
- the changes in assumptions and the effect of those changes on the proposed premiums, including reconciliation between the previous and proposed new base premium for a Sydney passenger vehicle for which the policyholder is not entitled to any ITC.
(q) Insurers must undertake sensitivity analysis on key assumptions that are subject to significant uncertainty to quantitatively illustrate the impact of uncertainty on proposed premiums. Such sensitivity analysis includes the use of scenarios to test the impact of multiple assumptions simultaneously.
- The extent of the variation assumed on key assumptions for sensitivity testing should reflect an alternate reasonable and plausible situation. Insurers must document the results of the sensitivity analysis in the filing report.
- The Authority may provide guidance on the specific assumptions or scenarios to be tested and included in a filing before its submission.
(r) any other matter the insurer considered in determining premiums.
1.14 The Authority may request additional information or amendments to the premium filing.
Rejection of premiums by the Authority
1.15 The Authority may reject a premium filed under Division 2.3, section 2.22 of the Act if it is of the opinion that the premium:
(a) is excessive or inadequate in relation to actuarial advice and to other relevant financial information available to the Authority
(b) does not conform to the relevant provisions of these Guidelines, or
(c) will not fall within the range of premiums determined by the Authority under clause 2(3)(c) of Schedule 4 of the Act, ‘Savings, transitional and other provisions’.
1.16 The Authority will conduct a review of all filings lodged in accordance with Division 2.3 of the Act and these Guidelines. The Authority may also obtain actuarial advice or other relevant financial advice.
1.17 The Authority’s review will consider:
(a) whether a filing is considered incomplete. The Authority will determine completeness by reviewing the documentation, schedules and motor accident filing template required by these Guidelines. The Authority must be satisfied that there is materially sufficient explanation of the assumptions and filed premiums to enable a review of the quantitative and qualitative elements of the filing, and
- if classified as incomplete, the Authority may request further information from the insurer in accordance with section 2.20(7) of the Act, which will mean that time does not run in relation to the period allowed for rejecting the premium until the insurer complies with the Authority’s request, or
- the Authority may request its withdrawal and, if not withdrawn, will exercise its discretion to reject the filing.
(b) whether the premium has been determined in accordance with the process set out in these Guidelines. This will include the requirement to provide additional information regarding the premiums filed and to justify premiums that have been filed.
Special provisions for premiums during the transitional period
1.18 In determining the Authority’s opinion on whether the premium is adequate and not excessive under section 2.22(1)(a) of the Act, the Authority will consider the comparison between its assumptions (in Schedule 1E) and those filed by the insurer.
Premium components and factors
Motor accident schedule of premium relativities
1.19 As part of the motor accident filing template, the Authority will provide a Motor Accident Schedule of Premium Relativities. Insurers must classify vehicles based on this Schedule.
1.20 Insurers must apply the relevant premium relativities that are applicable to the vehicle class and region.
Base premium
1.21 The base premium for each vehicle classification and region must be:
(a) calculated as the class 1 metro vehicle base premium for which the policyholder is not entitled to any input tax credit (ITC)
(b) multiplied by the relativity for the particular vehicle class and region published in the motor accident schedule of insurer premium relativities current at the date the third-party policy begins
(c) divided by 100.
1.22 The nominated base premium is used to define the allowable range of premiums in terms of the limits for bonus malus, the relative premiums for vehicle classifications and regions, and the loading that allows for policyholder entitlement to an ITC. It is equal to:
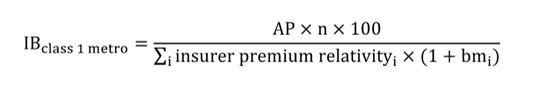
Where:
- IBclass1metro = The insurer’s base premium for class 1 metro including GST but excluding the Fund levy, calculated as if no policyholders are entitled to any ITC. The Fund levy is the combined total of the Motor Accidents Operational (MAF) Fund levy, Lifetime Care & Support (LTCS) Fund levy and Motor Accident Injuries Treatment & Care (MAITC) Fund levy
- AP = The insurer’s average premium including GST but excluding the Fund levy, calculated as if no policyholders are entitled to any ITC, as shown in the filing assumptions summary sheet (Table 1.2, Schedule 1C)
- insurer premium relativityi = The premium relativity applicable to the i-th policy, as anticipated to be underwritten over the period of the premium filing based on the motor accident schedule of insurer premium relativities
- bmi = The bonus malus rate (%) applicable to the i-th policy, as anticipated to be underwritten over the period of the premium filing
- n = The number of policies anticipated to be underwritten over the period of the premium filing.
Ratio of insurer’s average premium to class 1 metro (item 13 in Table 1.2)
1.23 This factor expresses the ratio of the insurer’s average premium based on the insurer’s projected portfolio mix (annual policy equivalent, taking into account the insurer’s vehicle class and region mix of business), relative to the base premium of a class 1 metro vehicle. This is calculated by:
(a) determining the percentage of the insurer’s projected portfolio (based on the number of vehicles) that will be written in each vehicle class and region
(b) multiplying each of the above proportions by the motor accident schedule of premium relativities published by the Authority for the corresponding vehicle class and region
(c) adding up all of the values calculated in (b) above
(d) dividing (c) above by 100.
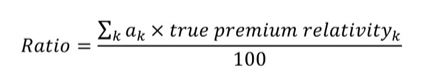
1.24 The formula for the calculation is:
Where:
- αk = The proportion (as a %) of the insurer’s projected portfolio (based on vehicle count) for the k-th vehicle class and region
- true premium relativityk = The premium relativity for the k-th vehicle class and region in the motor accident schedule of insurer premium relativities published by the Authority.
Bonus malus factor (item 14 in Table 1.2)
1.25 This factor expresses the average bonus malus applied by an insurer to its projected annual policy equivalent portfolio (after taking into account the insurer’s vehicle class and region mix of business). This is calculated by:
(a) determining the total portfolio premium (before GST and levies) to be collected, inclusive of the bonus malus rates to be applied, for the portfolio of risks projected to be written by the insurer. This portfolio of risks should take into account the insurer’s mix of business by vehicle class, region and rating factors
(b) determining the total portfolio premium (before GST and levies) to be collected, before the application of any bonus malus rates, for the portfolio of risks projected to be written by the insurer
(c) dividing (a) by (b).
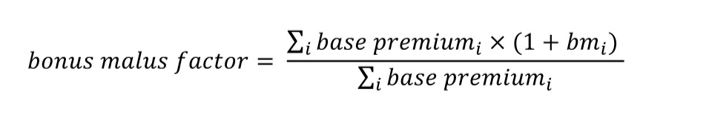
1.26 The formula for the calculation is:
Where:
- base premiumi = The applicable base premium ($) for the i-th policy based on its vehicle class and rating region
- bmi = The bonus malus rate (%) applicable to the i-th policy given the rating factors and bonus malus structure adopted by the insurer.
Bonus malus limits, rating structure and risk rating factors
1.27 Each risk rating factor proposed by an insurer must be objective and evidence-based. A risk rating factor must not be used unless approved by the Authority. Insurers can apply to use objective risk rating factors except race, policy duration, ITC entitlement and postcode.
1.28 Insurers can apply to use objective risk rating factors except race, policy duration, ITC entitlement and postcode.
1.29 Insurers may apply separately to the Authority for approval to use any proposed new objective risk rating factor.
1.30 The Authority encourages insurers to apply to use innovative rating factors that differentiate risk with quantifiable data, including telematics. Alternative pricing mechanisms, including initial premium payments combined with premium refund or extra premium options, are possible for all vehicle classes. Insurers may refund part of the premium paid for a third-party policy during or after the period for which the policy is issued, by reference to digital information recorded about the safe driving of the insured vehicle during that period, or other factors including the distance travelled. If insurers wish to apply these refund provisions to any vehicle class, the basis and methodology must be approved by the Authority.
1.31 Where there is a significant change to an insurer’s bonus malus structure or change in the bonus malus applied to a group of policyholders (more than 10% change in the bonus malus percentage applied compared to the current rating structure in force, in absolute terms), an insurer must include in their filing:
(a) analysis showing the technical relativity (or cost) for each group of policyholders within the rating factor for which bonus malus changes are proposed
(b) a comparison of the technical relativity (or cost) against the actual premium relativity or bonus malus percentage (or cost) proposed.
1.32 Where an insurer proposes a rating structure that is significantly different from the technical basis, reasons for the difference must be discussed in the filing report.
1.33 The various levels of the bonus malus filed by a licensed insurer for each vehicle class and rating region must be supported by experience-based evidence or a reasoned assessment of risk and/or strategic commercial reasons, except where an absolute bonus malus has been mandated by the Authority. An insurer must not charge the maximum malus for all vehicles in a particular vehicle classification unless this is supported by such evidence or assessment.
Malus limits
1.34 The maximum malus percentage may be calculated exactly or rounded to the nearest one tenth of 1%. For example, a multiple calculated as 51.2657% may be applied without rounding or rounded to 51.3%.
1.35 Premiums charged by an insurer must be no greater than the multiple shown in of the insurer’s base premium, excluding GST, for the vehicle classification and each region.
Table 1.1: Multiple of the insurer’s base premium, excluding GST
Vehicle classes | Maximum malus |
|---|---|
1, 3c, 3d, 3e, 5, 6a, 6b, 6c, 8, 9a, 9d, 9e, 9f, 11, 12a, 13 and 18a | (145% x RB + (IB – RB) x 30%)/IB |
7 | Not more than 140% of the insurer’s base premium excluding GST |
10d, 10e, 10f, 10g and 10h | (130% x RB + (IB – RB) x 30%)/IB |
6d, 6e, 12b, 14, 15a, 15c, 17, 18b, 18c and 21 | Not more than 110% of the insurer’s base premium excluding GST |
Where:
- IB = The insurer’s filed base premium for a class 1 metro vehicle for which the policyholder is not entitled to any ITC
- RB = The reference base rate at the time of filing.
Bonus limits
1.36 For premiums charged by an insurer for specific vehicle classifications by region:
(a) If the vehicle is a new non-fleet class 1 vehicle, premiums may be restricted to 80% of the base premium, excluding GST, for each region. If a bonus limit is applied under this provision, then the bonus malus limits in clauses 1.35 and 1.37 do not apply.
- New = Original (establish) registration for current year and including plus or minus one year.
- Non-fleet = A fleet of fewer than 5,000 class 1 or class 3c (or both) vehicles.
1.37 Otherwise for class 1 vehicles and class 3c vehicles that are not part of a fleet, if the youngest driver is aged:
(a) under 55, the minimum premium is no less than 80% of the insurer's base premium, excluding GST, for these vehicle classes by region
(b) 55 or over, the minimum premium is no less than 75% of the insurer's base premium, excluding GST, for these vehicle classes by region.
1.38 Otherwise for fleet vehicles, if the:
(a) fleet comprises 5,000 or more class 1 or class 3c vehicles (or both) owned by a single entity or registered operator, or a group of related entities or registered operators, that proposes to insure third-party policies with one or more licensed insurers, the minimum premium is no less than 60% of the insurer's base premium, excluding GST, for these vehicle classes by rating region.
1.39 Premiums charged by an insurer for vehicle classes 10d, 10e, 10f, 10g and 10h must be no less than 80% of the insurer's base premium, excluding GST, for the vehicle classes by region.
1.40 Premiums charged by an insurer for vehicle classes 3d, 3e, 5, 6a, 6b, 6c, 8, 9a, 9d, 9e, 9f, 11, 12a, 13 and 18a must be no less than 70% of the insurer's base premium, excluding GST, for the vehicle classes by region.
1.41 Premiums charged by an insurer for vehicle classes 6d, 6e, 12b, 14, 15a, 15c, 17, 18b, 18c and 21 must be no less than 90% of the insurer's base premium, excluding GST, for each of these vehicle classes by region.
1.42 Premiums charged by an insurer for vehicle class 7 must be no less than 80% of the insurer's base premium, excluding GST.
Premiums where entitlement to an ITC is applicable
1.43 Specific premiums apply when the vehicle owner is entitled to an input tax credit (ITC) for GST purposes to allow for the tax treatment. The insurer will determine two sets of premium rates:
(a) nil ITC premium rates, which apply to policyholders with no entitlement to any ITC for GST included in the premium
(b) some ITC premium rates, which apply to policyholders entitled to claim an ITC for at least some of the GST included in the premium. Some ITC premium rates will be the insurer's corresponding nil ITC premium rates increased by a loading.
1.44 Each insurer will determine the percentage loading it considers appropriate. However, the loading, expressed as a percentage of the corresponding nil ITC premium rates, must be within the range of 6.5% to 7.5%.
1.45 The loading will be determined in relation to the effect of policyholders' entitlement to claim an ITC on the insurer's entitlement to claim decreasing adjustments for claims costs attributable to those policyholders.
1.46 The ITC loading must be the same percentage for each vehicle classification and region. However, threshold variations in the percentage loading attributable only to the calculation of premiums for non-annual policies or to rounding are acceptable.
Loading of premiums for short-term policies
1.47 For quarterly or six-month policies, short-term insurer premiums may include a surcharge (the short-term policy surcharge), excluding GST, LTCS levy and MAF levy, which is calculated as follows:
- Quarterly premium = (annual premium + X) x (100% + Y%) / 4
- Half-yearly premium = (annual premium + A) x (100% + B%) / 2
Where:
Annual premium excludes GST, LTCS levy and MAF levy X, Y, A and B are amounts that each insurer will determine, subject to:
- X (administrative costs loading for quarterly policies) being no more than $15
- Y (a forgone investment income loading for quarterly policies) being no more than 2.2%
- A (administrative costs loading for half-yearly policies) being no more than $5
- B (forgone investment income loading for half-yearly policies) being no more than 1.5%.
1.48 Each licensed insurer must set one proposed rate for each of the factors X, Y, A and B that will be applied consistently across all short-term CTP policies offered by that insurer. The proposed loadings will be included in all filings and must be approved by the Authority. The surcharge does not apply to short-term periods for common due date policies. GST and the pro rata Fund levy for the relevant policy term are then added to calculate the total amount payable by the policyholder for a short-term policy, initially to the nearest one cent.
Justifying third-party premium assumptions
1.49 Insurers must specify how they have determined proposed premiums and explain the proposed premiums to the satisfaction of the Authority. Insurers are required to complete the Authority's motor accident filing template.
1.50 The total estimated claims cost (risk premium) adopted in the filing must:
(a) reflect the expected outcomes of the Act
(b) be on a central estimate basis; that is, an estimate of the mean, which must not be intentionally or knowingly conservative or optimistic.
Basis of estimate
1.51 Expense assumptions adopted in the filing must be set with reference to:
(a) maximum rates of expense assumptions specified by the Authority
(b) excluding expenses not directly relevant to the acquisition, policy administration or claims management of the insurer's third-party insurance business
(c) the suitability of the expense type for inclusion in a compulsory insurance product and the efficiency of the insurer's own administration and claims processes
(d) the insurer's best estimate of expenses, taking into account current internal management budgets and internal strategies to control costs.
Level of explanation
1.52 Filed assumptions for must be explained with sufficient information that an analysis of the filing can lead to a conclusion that the results stated in the filing:
(a) have been determined on a central or best estimate basis where required
(b) meet the adequate test under section 2.22(1)(a) of the Act
(c) represent a genuine effort on the part of the insurer to offer competitive premiums and thereby allow the Authority to form an opinion under section 2.22(1)(a) of the Act that the filed premium is adequate and not excessive.
1.53 The level of detail to be provided will depend on the price impact of the assumptions, the extent of the uncertainty surrounding the assumptions, the nature of the analysis and considerations of materiality as viewed by the Authority.
Actuarial valuation report
1.54 Each licensed insurer must provide the Authority with a copy of its latest full valuation report (when it is completed, including all appendices) relating to its NSW CTP business. If a full valuation of the NSW CTP portfolio is conducted more frequently than annually, the insurer must provide the most recent full valuation report available. A comparison and explanation of any differences between the filed assumptions and the following assumptions from an insurer's NSW CTP portfolio insurance liability valuation report assumptions must be provided in filings:
(a) claim frequency assumed for premium liabilities†
(b) average claim size assumed for premium liabilities†
(c) superimposed inflation
(d) economic assumptions
(e) claim-handling expense assumed for premium liabilities†
(f) policy and administration expense assumed for premium liabilities†.
† If premium liabilities are not estimated at a given balance date, then the insurer should use the latest accident year/underwriting year. Claim frequency and average claim size may be considered in aggregate (for example, as a risk premium) if an insurer's adopted methodology for the full valuation does not enable such a breakdown.
1.55 Insurers must explain any developments in experience since the most recent full valuation as part of this comparison.
CTP business plan and management accounts
1.56 Each licensed insurer must provide the Authority annually with a copy of its current NSW CTP business plan and disclose all relevant business and distribution strategies when significant changes are made. Each licensed insurer must provide the Authority with a copy of its NSW CTP management accounts annually. In addition, the insurer must provide a:
(a) comparison of budgeted expenses and actual expenses for the previous filing period
(b) detailed budget of expenses covering the proposed filing period.
1.57 The above expense analysis should show the following expenses separately (to the extent they have been broken down as such in the management accounts):
(a) commission
(b) acquisition and policy administration expenses
(c) claims-handling expenses
(d) any other expense components itemised in the insurer's own management accounts.
Discount rate assumptions
1.58 Insurers must use rates of discount that are no less than the risk-free rates based on the forward rates implied from market information available at the time of preparing the filing, being applied to the average underwriting date of the period filed.
1.59 Insurers must disclose the single weighted average discount rate calculated by applying the payment pattern or expected weighted mean term for the claim liabilities underlying the policies to be underwritten to the insurer's adopted rates of discount.
Maximum rates of assumptions used in the determination of premiums
1.60 The Authority's intention in setting maximum rates of assumptions is to reflect current market conditions. Alignment to changing market conditions will be considered through periodical reviews. The following assumptions are subject to a maximum rate used in the determination of premiums:
(a) claims-handling expense assumptions must not exceed a rate of 8% of risk premium
(b) acquisition and policy-handling expenses, including commission and other remuneration, are subject to a maximum rate of $43.60 per policy (on average across the policies underwritten by an insurer), indexed with movement in CPI
(c) the superimposed inflation assumption must not exceed a rate of 2.5%
(d) the maximum profit margin for determining premiums is 8% of the proposed average gross premium (excluding levies and GST).
1.61 The Authority will review these maximum rates periodically.
1.62 Under section 2.22(8) of the Act, the Authority is not bound by any of the maximum rates of assumptions if it considers that it would be unreasonable to apply them in the particular circumstances of the case. The Authority may choose not to reject a premium filing that exceeds the maximum rates if the insurer:
(a) has made allowances for innovation and efficiency that are forecast to improve scheme and policyholder outcomes, or
(b) has held its licence for less than three years.
(c) To avoid doubt, the Authority may still reject the insurer's premium filing even if such circumstances exist.
Risk equalisation mechanism (REM)
1.63 In determining proposed premiums, the insurer must consider any risk equalisation arrangements that the Regulation may impose under section 2.24(2) of the Act or in accordance with section 2.24(7) of the Act.
Calculating net REM amount
1.64 Insurers must calculate the net REM amount consistent with the Authority's motor accident filing template and Schedule 1D related to the filing period by:
(a) projecting the number of annualised policies to be issued for the filing period by each REM pool and for the total of other classes and regions that are not part of the REM pools
(b) multiplying the projected number of annualised policies for the filing period above by the REM $ amount for each REM pool prescribed by the Risk Equalisation Mechanism Deed
(c) the sum of all the REM amounts for all REM pools from the above clause divided by the projected number of annualised policies for all classes and regions (including those not in REM pool) for the filing period
(d) This result is the net REM amount per policy that is included in item 12a of Schedule 1C of these Guidelines.
Portfolio analysis
1.65 Insurers must provide a portfolio analysis consistent with the format detailed in the Authority's motor accident filing template. The following information and analysis relating to portfolio mix must be provided:
(a) the expected future number and mix of insured vehicles by vehicle class and rating region at each bonus malus level, including commentary on strategies that are expected to result in any changed mix of business
(b) actual past number and mix of insured vehicles for the previous 12 months (for a period ending no earlier than two months before the rate filing is submitted) by vehicle class and rating region at each bonus malus level that applied for each policy written within that 12-month period
(c) for each REM pool, compare the projected mix of business from the last filing against actual mix, including a detailed explanation of any variation of projected mix from recent experience
(d) the net impact of the REM based on the projected mix
(e) the proposed use of bonus malus, and the basis on which they will be offered to all vehicle owners, including a complete description of the rating structure, each rating factor with relevant qualifying time periods, where applicable, definitions of generic terminology, a summary of the explicit changes in bonus malus since the previous filing and the impact on the insurer's required and expected average premium
(f) for all policyholders to be issued a renewal notice during the proposed filing period (assuming 100% retention), the distribution by numbers of policies experiencing a price increase/decrease (including Fund levy and GST) using incremental bands designated in the Authority's motor accident filing template compared to the actual premium paid for in force policies for each of the following vehicle classes (in Excel format):
- class 1 by rating region
- class 3c by rating region
- class 3d
- class 3e
- class 6a
- class 7 by plate type
- classes 10d, 10e, 10f, 10g and 10h combined
- classes 6d, 6e, 12b, 14, 15a, 15c, 17, 18b, 18c and 21 combined
- all remaining classes combined
- all classes combined in aggregate.
(g) the expected number of policies by underwriting quarter split by vehicle class, region, ITC entitlement, policy duration and at each bonus malus level, with premium income split by insurer premium, MAF levy, LTCS levy, MAITC levy, GST and total payable (in Excel format)
(h) the resulting average bonus malus factor for each vehicle class and rating region (in Excel format).
Motor accident filing template
1.66 The Authority's motor accident filing template must be attached to every filing report and the data format must not vary from the specifications prescribed in the motor accident filing template. The following documents and the Authority's motor accident filing template are to be attached to every filing report.
Schedule 1A
1.67 Insurers must provide the base premium, including GST but excluding Fund levy, for each vehicle classification and region for policyholders who are not entitled to any ITC (PDF version in filing report and Excel version using the Authority's motor accident filing template).
Schedule 1B
1.68 Insurers must provide a full description of the proposed bonus and malus structure and the actual amounts (after applying any rounding) proposed to be charged for each vehicle classification, region and bonus malus rate, subdivided into separate amounts of:
(a) GST
(b) insurance premium excluding GST
(c) Fund levy
(d) total payable by the policyholder.
1.69 Separate schedules are required for nil ITC premium rates and some ITC premium rates respectively, for both annual and short-term policies.
Schedule 1C
1.70 Insurers must provide a summary of the assumptions adopted and base premium filed (PDF version in filing report in the form specified in Table 1.2 and an Excel version using the Authority's motor accident filing template).
Table 1.2: Premium filing summary sheet
Item | Premium factors | Assumption |
|---|---|---|
1a. Assumed frequency | Claims for an industry mix of vehicles (net of sharing and nominal defendant) | % |
1b. | Relativity of the claims frequency for the insurer’s mix of vehicles to the claims frequency for an industry mix of vehicles | |
1c. | Claims for insurer (net of sharing and nominal defendant) | % |
2a. Average claims size, start of underwriting period | Claims in current dollar values for an industry mix of vehicles (gross of reinsurance, net of sharing and nominal defendant)1 | $ |
2b. Average claims size, start of underwriting period | Claims in current dollar values for insurer (gross of reinsurance, net of sharing and nominal defendant)1 | $ |
3a. Average claims size for filing period | Claims for an industry mix of vehicles for filing period (from item 2), fully inflated and discounted to the middle of the period filed1 | $ |
3b. | Relativity of the claims average claim size in current dollar values for the insurer’s mix of vehicles to the claims average claim size in current dollar values for an industry mix of vehicles | |
3c. Average claims size for filing period | Claims for insurer for filing period (from item 2c) fully inflated and discounted to the middle of the period filed1 | $ |
4. | Insurer average risk premium (formula used to combine above assumptions to arrive at average risk premium) (1c x 3c)1,2 | |
5. Average risk premium | Excluding GST calculation (substitute values in formula)1 | $ |
6. Acquisition and policy-handling expenses, including commission | Per cent gross premium excluding GST and Fund levy | $ |
7. Claims-handling expenses | Per cent gross premium excluding GST and Fund levy | % |
8. Net cost of reinsurance loading | Per cent gross premium excluding GST and Fund levy | % |
9. Other assumptions | Specify nature and value of assumption | % |
10. Profit margin | Per cent gross premium excluding GST and Fund levy | % |
11. Average premium | Formula used to arrive at average premium excluding GST and Fund levy) ((5 + 9)/(1 -(6 + 7 + 8 + 9 + 10))2 | |
12. | Excluding GST and Fund levy (substitute values in formula)1 | $ |
12a. | Net overall impact of the REM (net REM $ per policy) (refer to the Authority motor accident filing template D3) | $ |
12b. | Required average premium (item 12 less item 12a) | $ |
13. | Ratio class 1 metro to average premium calculated in accordance with the formula in ‘Ratio of insurer’s average premium to class 1 metro’ section of this Part of the Motor Accident Guidelines | |
14. Bonus malus | Bonus malus factor calculated in accordance with formula in ‘Bonus malus factor’ section of this Part of the Motor Accident Guidelines | |
15. Class 1 metro premium | Nil ITC class 1 metro base premium excluding GST and Fund levy (12b ÷ 13 ÷ 14) | |
16. | Nil ITC class 1 metro base premium including GST but excluding Fund levy | $ |
17. | Minimum nil ITC class 1 metro premium including GST but excluding Fund levy (ignoring premiums calculated using a bonus factor of less than 80%) | $ |
18. | Minimum nil ITC class 1 metro amount payable by policyholder including GST and Fund levy (ignoring amounts calculated using a bonus factor of less than 80%) | $ |
19. | Maximum nil ITC class 1 metro amount payable by policyholder including GST and Fund levy | $ |
20. | Loading applied to nil ITC premium rates to calculate some ITC premium rates (0% ITC premium rates) | % |
21. | MAF levy (class 1 metro) | $ |
22. | Administrative costs loading for quarterly policies (X) | $ |
23. | Forgone investment income loading for quarterly policies (Y) | % |
24. | Administrative costs loading for half-yearly policies (A) | $ |
25. | Forgone investment income loading for half‑yearly policies (B) | % |
26. | Period premiums are proposed to apply |
Notes:
- Estimates of average claim sizes and average premiums must be those applicable to the nil ITC premium rates; that is, calculated as if no policyholders have any entitlement to an ITC, and as if the insurer has an entitlement to decreasing adjustments or ITC for all claims costs directly attributable to specific policies. The loading applied to nil ITC premium rates to calculate the insurer's some ITC premium rates is then shown as item 20.
- Use item number for formula description.
Schedule 1D
1.71 Insurers must provide details of the calculation of the net REM amounts in the form specified in the Authority's motor accident filing template.
Schedule 1E (transition period only)
1.72 Each insurer must use the form specified in Table 1.3 to provide a summary of its filed assumptions compared to the Authority’s costing assumptions for the Scheme.
Table 1.3: Summary of the insurer’s filed assumptions compared to the Authority’s costing assumptions for the Scheme
Assumption description (column A) | Authority’s costing assumptions for the Scheme (column B) | Insurer’s adjusted assumption for the industry (column C) | Relativity of insurer assumption to industry assumption (column D) | Insurer assumption (column E) |
|---|---|---|---|---|
Claims frequency: at‑fault (AF) threshold injury claims | 0.030% | |||
Claims frequency: not at‑fault (NAF) threshold injury claims | 0.086% | |||
Claims frequency: NAF claims WPI >10% | 0.024% | |||
Claims frequency: NAF claims WPI <=10% | 0.035% | |||
Claim frequency - Death, Interstate and Workers’ Compensation (WC) | 0.015% | |||
Claim frequency - Early Notification | 0.006% | |||
Total claims frequency | 0.195% | |||
Average claims size (ACS): AF claims (15/01/24 dollars) | $28,600 | |||
ACS – NAF threshold injury claims (15/01/24 dollars) | $11,400 | |||
ACS: NAF claims WPI >10% (15/01/24 dollars) | $636,200 | |||
ACS: NAF claims WPI <=10% (15/01/24 dollars) | $138,600 | |||
| ACS - Death, Interstate and WC (15/01/24 dollars) | $103,700 | |||
| ACS - Early Notification (15/01/24 dollars) | $200 | |||
Total ACS all claims (15/01/24 dollars) | $119,700 | |||
Total ACS (inflated/discounted and 15/07/24 dollars)† | $126,600 | |||
Weighted average duration of payments (15/01/24 dollars) | 3.65 | |||
Claims inflation: wage inflation (overall weighted average) | 3.56% | |||
Claims inflation: superimposed inflation (overall weighted average) | 2.15% | |||
Discount rate (overall weighed average) | 4.26% | |||
Risk premium: inflated and discounted risk premium for underwriting year beginning 15 January 2024† | $247 | |||
Claims-handling expense (% of risk premium) | 8.00% ($19.73) | |||
Net reinsurance expense | $1.20 | |||
Policy and acquisition expense | $43.60 | |||
Profit margin (% of premium excl. GST and levies) | 8.00% ($27.05) | |||
GST (10%) | $33.82 | |||
| REM Adjustment | $1.13 | |||
Insurer premium (incl. GST) | $373 | |||
| Estimated additional costs | ||||
MAF levy | $14.10 | |||
LTCS levy | $102.43 | |||
MAITC levy | $24.61 | |||
Total premium payable (incl. GST and levies) | $514 |
Uninflated undiscounted average claim size in 15/01/24 dollars.
Totals may not add due to rounding.
† Discounted to the middle of the underwriting year beginning 15 January 2024 (i.e. 15 July 2024).
Description of each column
Column A: describes the type of assumption.
Column B: sets out the Authority's scheme-wide premium parameters for the industry to achieve the overall target average premium.
Column C: insurer industry assumption for an industry mix of business - allows for comparison against the Authority's independent actuary assumptions in column B.
Column D: relativity of insurer assumption to industry assumption to allow for differences in the insurer's portfolio of risks to be better or worse experience than the industry before business mix adjustment (which is based on the mix by class/region from relativities) and any other claims-related differences.
Column E: insurer assumption.
Other notes
- Total claims frequency for column C should be the same figure as in item 1a in Schedule 1C.
- Total claims frequency for column E times the relativity for the insurer's mix of vehicles should be the same figure as in item 1c in Schedule 1C.
- Average claims size (1/04/2023 dollars) for column C should be the same figure as in item 2a in Schedule 1C.
- Average claims size (1/04/23 dollars) for column E times the relativity for the insurer's mix of vehicles should be the same figure as in item 2b in Schedule 1C.
- Average claims size (inflated/discounted dollars) for column E times the relativity for the insurer's mix of vehicles should be the same figure as in item 3c in Schedule 1C.
- Column E for risk premium (fully inflated and discounted to the middle of the period filed) should be the same figure as in item 5 in Schedule 1C.
- For the accident period referenced above, the following is relevant:
- The period represents accidents that occur from 1 April 2023 to 31 March 2024.
- The period represents statutory benefit claims that will be reported from 1 April 2023 to 30 June 2024 allowing for the statutory 3 months reporting period. There will also be claims reported after 30 June 2024 that may also be accepted as valid statutory benefit claims depending on the circumstance of their lodgement (known as late claims). Only after all of the late claims have been reported and accepted will the actual number of statutory benefit claims be known i.e. after 30 June 2024.
- The period represents claims for damages that will be lodged from 1 April 2023 (for claims assessed at greater than 10% whole person impairment) and from 1November 2024 (for claims assessed at equal to or less than 10% whole person impairment) to 31 March 2027. There will also be claims for damages lodged after 15 January 2026 (for accidents on 1 April 2023) and after 31 March 2027 (for accidents on 31 March 2024) that may also be accepted as valid claims.
Part 2 of the Motor Accident Guidelines: Market Practice
Market practice
Definitions
2.1 Table 2.1 shows the meanings of terms used in this part of the Motor Accident Guidelines.
Table 2.1: Terms used in this part of the Motor Accident Guidelines
Term | Definition |
|---|---|
Distribution channel | A mechanism or method through which licensed insurers issue and administer third-party policies. This can include but is not limited to agents, telephone call centres, the internet and over-the-counter operations. |
eGreenSlip | The electronic notification of a third-party policy by an insurer to Roads & Maritime Services. |
Input Tax Credits (ITC) | That is, the credit an entity registered for GST can claim for any GST included in the third-party premium paid. |
Roads & Maritime Services (RMS) | A NSW statutory authority constituted by the Transport Administration Act 1988 (NSW). |
Introduction
2.2 This Part of the Guidelines is issued under Part 9, Division 9.2, section 9.16 of the Act, to provide the regulatory framework for issuing of third-party policies by licensed insurers.
Note: Clause 8.3 of Version 2 of the Motor Accident Guidelines: Determination of insurance premiums for taxis and hire vehicles provides that the Motor Accident Guidelines: Determination of insurance premiums for taxis and hire vehicles apply to taxis and hire vehicles and, in the case of taxis and hire vehicles, the Motor Accident Guidelines: Determination of insurance premiums for taxis and hire vehicles apply in place of other current Motor Accident Guidelines, but only to the extent of any inconsistency.
2.3 These Guidelines are principles-based. They articulate a set of objectives for issuing of third-party policies and expectations for standards of market practice for insurers. The Authority’s adoption of principles-based regulation of market practice is intended to:
(a) encourage flexibility and innovation in the delivery of services to third-party insurance customers
(b) promote a competitive market for all insurers and encourage insurers to act in good faith when interacting with customers.
2.4 Insurers’ market practice, including distribution arrangements, must align with these Guidelines and not contravene these Guidelines.
2.5 To further assist compliance with these Guidelines, the Authority may publish practice notes.
Commencement and revocation of previous Guidelines
2.6 This Part is effective for market practice from the commencement of these Guidelines and will remain in force until they are amended, revoked or replaced.
Application of these Guidelines
2.7 The Authority will monitor and review compliance with these Guidelines, which may include audits of insurers from time to time.
2.8 Internal auditing of compliance with these Guidelines must form part of each insurer’s own risk management and compliance program. Insurers have a responsibility to report to the Authority any results of audit programs conducted on issuing third-party business.
2.9 If the Authority regards an insurer or any intermediary acting on behalf of the insurer as having breached the Guidelines, the Authority may take regulatory and enforcement action, in accordance with its regulatory and enforcement policy.
2.10 All contracts or arrangements entered into by the insurer in relation to a quote and sales services for third-party policies must comply with these Guidelines.
Guiding principles
2.11 When issuing, administering or renewing third-party policies, the insurer and their agents must:
(a) act in good faith with all customers
(b) use processes and business practices that do not unfairly discriminate against individual customers or groups of customers
(c) engage in processes and business practices that are transparent and practical for the purpose of issuing policies to customers
(d) make third-party policies readily accessible and available to all customers.
Acting in good faith
2.12 The Authority’s regulation of premiums includes an element of community rating, as some policies are underpriced and others overpriced relative to insurance risk. Accordingly, it may be in the insurers’ financial interests to build portfolios that are overweight in low risk (overpriced) policies. Notwithstanding such financial interests and the REM, under Division 2.3, section 2.24 of the Act, insurers must make third-party policies available to all customers in a manner that complies with all of the guiding principles. In particular:
(a) insurers and their agents are required to issue policies to all properly identified vehicles
(b) insurers must avoid distribution methods and sales techniques that prejudice this obligation in any way.
Processes and business practices that do not unfairly discriminate
2.13 Insurers and their agents must use processes and business practices that do not unfairly discriminate against individual customers or groups of customers, directly or indirectly. This applies to each distribution channel.
(a) Direct discrimination includes when a person is treated less favourably than another because they happen to belong to, or are associated with, a particular group of persons. Indirect discrimination is the result of unintentional practices and processes that appear to be fair to everyone but in fact have an unfair or unequal impact on a particular group of persons.
(b) Discrimination may not be considered unfair if it is based upon actuarial or statistical data from a source on which it is reasonable to rely, and is reasonable having regard to the data and any other relevant factors.
2.14 Each insurer and its agents must apply reasonable service standards to their processes and business practices. The Authority may impose standards or restrictions on any or all insurers and their agents for specific or general circumstances where it is considered to be in the public interest.
(a) Reasonable service standards include the provision of equitable access to insurer and agent services for persons with disability.
2.15 All existing customers who are due to receive a renewal notice must be provided with a renewal notice/offer within the prescribed timeframes as specified in this Part of the Guidelines. A delay in sending renewal notices may only occur with prior approval from the Authority.
2.16 Insurers must not refer customers to other insurers or encourage customers to take their business elsewhere. Agents must not refer customers to insurers unless they have an agency arrangement with them.
2.17 Insurers must not advise customers of the prices offered by other insurers. Agents must not advise customers of prices offered by insurers unless they have an agency arrangement with them.
Transparent and practical processes and business practices
2.18 All information provided to customers must be clear and accurate, expressed in plain language and not in any way misleading.
2.19 Insurers and their agents must only charge premiums as filed and approved by the Authority. Insurers are to categorise vehicles correctly and charge the correct filed premium for that category. In order to charge the correct premium, insurers and their agents must take into account all risk factors approved by the Authority and the ITC status used to determine the customer’s premium.
2.20 All agents contracted by an insurer to provide quotes and sales must ensure they disclose to customers the identity of all insurers they have a commercial arrangement with before they proceed with quotes or sales. Neither the insurer nor their agent may enter into a commercial arrangement with another agent or third party that accesses data from the Authority’s Green Slip Price Check without the relevant insurer first obtaining the Authority’s permission. The Authority will not unreasonably withhold such permission.
2.21 Where requested by a customer, insurers must act promptly and expeditiously when sending documents by mail or electronically:
(a) all documents agreed to be sent by mail must be lodged with Australia Post within three business days of agreeing to do so
(b) all documents agreed to be sent electronically must be sent within 24 hours of agreeing to do so
(c) should technology outages occur, the documents must be sent within 24 hours of the insurer’s systems being repaired.
2.22 Offers of renewal, including eRenewals, must be sent at least four weeks and no more than six weeks in advance of the expiry date.
2.23 All information regarding third-party policies must be sent to each customer by post unless they have consented to receiving policy information electronically.
2.24 Where an incorrect address has been used, including returned letters and failed emails, insurers must take reasonable steps to correctly issue the policy information.
2.25 When a customer purchases a third-party policy or renewal or new registration, the insurer must electronically transmit an eGreenSlip to RMS within the timeframes shown in Table 2.2. These timeframes are based on the method by which a customer pays for the eGreenSlip.
(a) The Authority may nominate a period during which the regulatory relief timeframes in Table 2.2 apply in place of the usual required timeframes. Such regulatory relief timeframes are intended to apply during a disaster, emergency or similar event where insurers as a whole would be expected to experience delays in transmitting an eGreenSlip through no fault of insurers. They are intended to apply for the shortest reasonable duration.
Table 2.2: Timeframes for insurers electronically transmitting an eGreenSlip
Method of payment | Requirement | Regulatory relief timeframes |
|---|---|---|
Directly to the insurer via a branch, telephone or electronic means | Within 1 hour of payment | Within 48 hours of payment |
To the insurer’s agent, including Australia Post | Within 5 business days of payment | Within 7 business days of payment |
By BPAY | Within 3 business days of payment | Within 5 business days of payment |
By mail to the insurer | Within 5 business days of the date of postage | Within 7 business days of the date of postage |
2.26 A written quote or a renewal notice/offer for a third-party policy must:
(a) clearly communicate all relevant pricing factors applied to the third-party policy or quotation
(b) provide information about how to raise any incorrect pricing factors with the insurer or its agent, before the purchase
(c) disclose the name of the licensed insurer and if they operate under a trading name that is different from the licensed insurer name, the quote or offer must disclose both the trading name and the insurer name
(d) provide contact details for third-party policy queries
(e) detail the timeframe for eGreenSlips to be sent to RMS, including the timeframe associated with purchasing through different channels.
2.27 Common Expiry Date Fleets and Multiple Expiry Date Fleets are exempt from the transparency requirements of pricing factors. Private use vehicle classes 1, 10 and 3c are not exempt and must show the pricing factors used on Green Slips. For example, age of youngest driver, age of vehicle etc.
2.28 All customer communication must include any information required by the Authority. Insurers must ensure they and their agents use specific scripts when required by the Authority.
Readily accessible and available
2.29 Third-party policies (both quotes and sales) must be readily accessible and available to all customers. Insurers are required to give prompt, uniform access and availability to all customers who approach them, irrespective of the risk characteristics of the vehicle and its owner. Insurers may use a range of distribution channels provided that every customer has ready access to their third-party policy through at least one of those channels. Insurers must not use distribution channels to avoid sales. In particular:
(a) insurers and their agents must not refuse to provide a third-party quote for any motor vehicle required to be insured under the Act
(b) insurers and their agents must provide customers with the ability to obtain a quote for any vehicle or vehicle class without the need to identify themselves or their vehicle’s registration number
(c) insurers and their agents must make reasonable efforts to help customers provide accurate information to determine the correct premium
(d) insurers must provide customers with at least one payment option for a quote or renewal offer that is available 24 hours a day, seven days a week.
Schedule 2A: Circumstances for refusal to provide a third-party policy
2.30 This schedule relates to the section ‘Readily accessible and available’.
2.31 Insurers and their agents may refuse to issue a third-party policy in the following circumstances:
(a) where the customer does not pay the required premium, the Fund levy and GST, for the third-party policy within the timeframe as agreed between the customer and the insurer or agent
(b) where the vehicle is recorded as a statutory written-off vehicle on the NSW written-off vehicles register (WOVR)
(c) where the customer is seeking to purchase a new third-party policy from an insurer and the customer does not provide the correct key identifiers used to locate and retrieve information held by RMS.
2.32 Key identifiers are:
(a) registration ID (also known as billing number) and plate number, or
(b) a combination of a customer identifier, one of:
- NSW driver or rider licence number of the vehicle owner
- NSW photo card number
- RMS customer number, and
a vehicle identifier, one or a combination of:
- vehicle identification number (VIN)
- chassis number
- engine number
- plate number.
Breaches and temporary regulatory relief arrangements
2.33 Insurers must notify the Authority of any breach of these Guidelines.
2.34 The Authority may consider a temporary relief from an enforcement response if an insurer is unable to issue timely third-party policy renewals due to unforeseen system issues.
2.35 An application for temporary regulatory relief can be made in writing to the Authority at any time. The Authority will take into account:
(a) the reasonableness of the request
(b) the length of time the relief is requested
(c) community requirements and priorities
(d) other relevant factors.
2.36 The Authority will respond to requests in a timely manner and, where appropriate, work with the insurer to help it comply with the Guidelines as soon as possible.
Part 3 of the Motor Accident Guidelines: Business Plans
Business plans
Requirements of the business plan
3.1 Under Division 9.2, section 9.18 of the Act, each insurer must prepare and deliver to the Authority a Motor Accident Business Plan (business plan) as soon as practicable after it is requested to do so by the Authority.
3.2 Insurers are to prepare and deliver to the Authority a business plan within the timeframe provided by the conditions of their license. Insurers are also to prepare and deliver a revised business plan before implementing any significant change to the conduct of their third-party insurance business (including but not limited to strategy in respect of claims handling, pricing or product distribution).
3.3 If the insurer operates more than one third-party insurance business (for example, the insurer issues third-party policies under multiple brands), then the insurer must prepare and deliver a business plan covering all of the third-party insurance businesses and any business associated with third-party policies of the insurer either in a single business plan (highlighting where the practices of the businesses/brands differ from one another) or separate business plans for each. For co-labelling or white labelling arrangements, the Insurer’s business plan must include where any operations are different from the arrangements otherwise outlined in the business plan.
3.4 A business plan prepared by a licensed insurer under section 9.18 must include a complete description of the manner in which the third-party insurance business is to be conducted (including but not limited to claims-handling, management, expenses and systems). This includes:
(a) details of the structure and operations of the third-party insurance business and any plans for change within the next 12 months in line with Schedule 3A below
(b) a demonstration of how the insurer’s conduct, culture and appetite for risk meets the needs of customers, the objects of the Act and the Authority’s Customer Service Conduct Principles, in line with Schedule 3B below
(c) a letter from the board of directors of the insurer to the Authority (whether signed by the directors, or on behalf of the directors by an officer authorised to sign on their behalf) confirming present and continuing compliance with Australian Prudential Regulation Authority’s (APRA) Prudential Standard CPS 232 or, if replaced, with the APRA prudential standard addressing business continuity management by authorised general insurers, including the development and maintenance of a business continuity plan.
3.5 The Authority may require further details by notice in writing in order to clarify the business plan.
3.6 Insurers must, on request from the Authority, submit copies of their customer communication templates, including third-party certificates and customer information packs.
3.7 When requested by the Authority, insurers must submit scripts, training manuals and other supporting tools used by sales staff for review and approval. Each insurer must, on request from the Authority, provide other documents related to third-party policies.
3.8 Insurers must amend any document submitted to the Authority if required to do so by the Authority.
Schedule 3A: Operational requirements for insurers
3.9 An insurer’s business plan must include the matters enumerated below relating to the structure and operations of the business, and detail how these comply with the Act and align with its objects.
3.10 A detailed plan of the insurer’s business structure, operations and relevant key performance indicators (and intended changes in the next 12 months), including:
(a) focus areas for the next 12 months and how progress is monitored and evaluated
(b) premiums and policy
(c) pricing strategy and distribution, including third-party agreements
(d) claims and injury management (claims segmentation models, caseloads, claims management strategies, outsourcing and third-party agreements)
(e) fraud deterrence and prevention under section 6.39 of the Act
(f) internal review and disputes (structure and approach to continuous improvement)
(g) supply chain management including panel arrangements and oversight of non-panel providers (cost, performance and conduct)
(h) use of in-house specialist resources (for example, legal or fraud specialists)
(i) systems management
(j) data quality framework
(k) engagement of staff and customers that aligns with the requirements in Schedule 3B.
(l) An insurer’s business plan must include a summary of the systems and processes in place to support injured people with psychological symptoms or injury. The insurer must demonstrate that it has systems and processes in place to ensure that claims are managed by a case manager, or the case manager is supported by specialist staff, with the skills, knowledge and experience to manage claims involving psychological symptoms or injury.
3.11 A detailed plan covering the insurer’s business structure and operations regarding offshore arrangements.
Schedule 3B: Culture requirements for insurers
3.12 An insurer’s business plan must include the matters enumerated below relating to the alignment of institutional culture with the objects of the Act.
3.13 A definition of the insurer’s target institutional culture.
3.14 A detailed plan of the steps to be taken to maintain or, if necessary, create an institutional culture understood by insurer senior managers and employees that:
(a) meets the objects of the Act
(b) meets the Authority’s Customer Service Conduct Principles below:
- be easy to engage and efficient
- act fairly, with empathy and respect
- resolve customer concerns quickly, respect customers’ time and be proactive
- have systems in place to identify and address customer concerns
- be accountable for actions and honest in interactions with customers.
3.15 A detailed plan of the steps to be taken to embed, monitor and (where appropriate) effect changes to the insurer’s institutional culture as it relates to each of the matters outlined in the above clause. This must include a strategy to report performance in these areas when requested by the Authority.
3.16 Details of:
(a) arrangements for conducting an annual employee engagement survey
(b) processes for assessing the results of employee engagement surveys.
3.17 Details of the:
(a) mechanisms established for personnel to elevate and report concerns about practices within the insurer, even when not making any specific allegation of wrongdoing
(b) processes for assessing such reports and identifying and addressing any unsatisfactory practices.
3.18 Details of:
(a) how the key performance indicators outlined in clause 3.10 (above) applying to personnel engaged in the insurer’s third-party insurance business demonstrate alignment with the target institutional culture
(b) the processes for assessment of personnel against those key performance indicators and the effectiveness of those key performance indicators to influence desired behaviours.
3.19 Details of the processes for:
(a) annual independent assessment of the insurer’s institutional culture as it relates to the matters enumerated in clause 3.14 (above)
(b) development of action items arising out of this assessment
(c) implementation of these action items.
3.20 An explanation of the organisational structures to monitor the effectiveness of, and ensure accountability for, the arrangements, mechanisms, processes and performance metrics enumerated in clauses 3.16 to 3.18 (above). This must include a strategy to report performance in these areas when requested by the Authority.
3.21 An explanation of the governance structures by which the board of directors of the insurer will form a view of the risk culture in the institution and the extent to which that culture supports the ability of the institution to operate consistently within its risk appetite, identifies any desirable changes to the risk culture and ensures the institution takes steps to address those changes.
Complaints
3.22 A complaint is an expression of dissatisfaction made to the insurer or its agent related to its products or services, or the complaints-handling process itself, where a response or resolution is explicitly or implicitly requested. Insurers must keep a record of all complaints they or any of their agents receive in a complaints register and provide a summary report to the Authority every six months. This report is due within 30 business days of the end of the 30 June and 31 December reporting periods. It should be formatted as set out by the Authority and include a complaints trend analysis of the risks and issues.
3.23 All complaints made to the insurer or its agents in relation to a third-party policy or claim must be handled in a fair, transparent and timely manner.
3.24 A robust complaints-handling process provides the complainant with confidence that they are heard, their feedback is taken seriously, and insurers are accountable for their actions. The insurer must have a documented internal complaint and review procedure, the terms of which must be set out in the insurer’s business plan.
3.25 Information about how to make a complaint and the complaints-handling procedures must be readily available and accessible to all stakeholders.
3.26 Complaints-handling procedures must refer to the rights of the customer to escalate a complaint to the Authority if they are dissatisfied with the insurer’s response to their complaint.
3.27 The insurer must acknowledge all complaints in writing within 5 business days of their receipt. The acknowledgement must include:
(a) if the insurer can resolve the complaint to the satisfaction of the complainant within 5 business days from the receipt of the complaint – the insurer’s written decision resolving the complaint
(b) if the insurer cannot resolve a complaint to the satisfaction of the complainant within 5 business days from the receipt of the complaint – a copy of the insurer’s complaints procedure and the contact details of the representative(s) of the insurer handling the complaint.
3.28 If the insurer cannot resolve the complaint to the satisfaction of the complainant within 5 business days, the insurer must resolve the complaint within 20 business days from the date of receipt and notify the complainant in writing of:
(a) the insurer’s decision and the reasons for that decision
(b) the opportunity to have the complaint considered by a more senior representative of the insurer who is independent of the original decision-maker
(c) information on the availability and the contact details of external complaint or dispute resolution handling bodies (including the Authority) in the event that the complainant is dissatisfied with the insurer’s decision or procedures.
Fraud
3.29 An Insurer’s business plan must include a summary of the processes they have in place to prevent, detect and respond to fraud as detailed below.
3.30 At all stages of the claims management and premium determination process, the insurer should have systems and processes in place to:
(a) prevent fraud - proactively putting into place measures and controls designed to help reduce the risk of fraud from occurring at the outset
(b) detect fraud - designing and implementing controls to uncover instances of fraud or potential fraudulent behaviour
(c) respond to fraud – taking action to mitigate the impact of fraudulent activity.
Information and data integrity
3.31 Information and data integrity is critical to the scheme and to demonstrating insurer performance. Accurate, up-to-date and complete information promotes the credibility and accountability of the scheme and those operating within it.
3.32 At the direction of the Authority, an insurer must provide timely, accurate and complete information, including but not limited to:
(a) insurer claims manuals, policies and procedure documents, including updates as they occur
(b) policyholder and claimant information packs
(c) standard letter templates
(d) self-audit results, including quality assurance reporting
(e) complaints received by the insurer about its handling of matters
(f) policyholder and claimant survey results
(g) training plans and logs, and/or data breaches that affect the privacy of a policyholder, claimant or their family.
3.33 An insurer must:
(a) code the claimant’s injuries by using appropriately trained coders applying the most recent Abbreviated Injury Scale (AIS) Revision (or as otherwise prescribed by the Authority) and claims in accordance with the Authority’s Motor Accident Insurance Regulation Injury Coding Standards and agreed timeframes
(b) provide up-to-date, accurate and complete data to the Universal Claims Database (UCD), in accordance with the Act and the Universal Policy Database (UPD) and the UCD Claims Data Manual, as amended from time to time, or as otherwise required by the Authority
(c) inform the Authority of any data quality issues as soon as the insurer becomes aware
(d) maintain consistency between information on the claim file and data submitted to the UCD and record any changes in accordance with the UCD Claims Data manual, as amended.
3.34 If the Authority becomes aware of any data quality issues, the Authority may request the insurer to resubmit the data and provide information on data quality controls.
3.35 Insurers must correct any errors that are notified through the UCD according to the timeframes for each of the following categories defined in the UCD Claims Data manual:
(a) Tier 0 validation checks for corrupted or wrongly formatted data - next business day
(b) Tier 1 validation checks for data essential to scheme performance measures - 10 business days
(c) Tier 2 and Tier 3 validation checks for all other data - 20 business days.
3.36 Insurers must comply with any Authority requirements for data exchange and centralised claim notification. Insurers must participate in online claims submission as determined by the Authority.
3.37 Insurers must retain digital claims files information and data for a minimum of:
(a) 30 years after the date the claim was made, or
(b) 30 years after the claimant turns 18 years of age, whichever is later.
3.38 Where an insurer notifies customers, claimants, service providers and/or the Australian Information Commissioner of a Notifiable Data Breach (in accordance with the Privacy Act 1988 (Cth)), the insurer must, at the same time, also notify the Authority. The notification to the Authority must:
(a) confirm that the insurer has fully complied with the law in terms of the notification
(b) confirm that the insurer has investigated, or is investigating, where and why the breach occurred
(c) set out what steps are being taken or have been taken to remedy the breach and future breaches
(d) set out what has been, or is being, suggested to rebuild trust with the affected claimants, customers and/or other stakeholders in terms of the handling of their personal and health information.
Self-assessment
3.39 An insurer must undertake self-assessment of its compliance with the Act and Guidelines in its management practices annually or more frequently as directed by the Authority. The self-assessment must comply with the requirements set out in SIRA’s Self-Assessment Tool.
3.40 An insurer must provide an annual self-assessment report to the Authority. This report must include the insurer’s assessment of its compliance with the Act and statutory instruments made under the Act (including these Guidelines), and details of all instances of its failure to comply (non-compliance) with legislative, guideline and Customer Service Conduct Principle requirements.
3.41 The Authority may conduct a review of an insurer’s self-assessment at any time by auditing the insurer’s files.
Part 4 of the Motor Accident Guidelines: Claims
Claims
Application of the Guidelines
4.1 This Part applies from the commencement of these Guidelines to all current and future claims made on insurers in respect of motor accidents that occur on or after 1 December 2017. They apply until they are amended, revoked or replaced.
4.2 The Motor Accident Guidelines: ‘Claims handling & medical (treatment, rehabilitation & care)’, which were issued by the Authority on 1 January 2017, continue to apply to claims in respect of motor accidents occurring on and from 5 October 1999 to 30 November 2017.
Introduction and purpose
4.3 These Guidelines are made under the Motor Accident Injuries Act 2017 (NSW) (the Act), including Section 6.1 of the Act. They make provision with respect to the manner in which insurers and those acting on their behalf are to deal with claims.
4.4 These Guidelines are to be read together with relevant provisions of the Act and Regulation. They are ordered in accordance with the claimant journey to help insurers read and apply them with the Act and Regulation, and to progress claims promptly.
Principles
4.5 Insurers and those acting on their behalf are to deal with claims in a manner consistent with the objects of the Act, the below principles and the general duties under Division 6.2 of the Act.
4.6 These principles apply across all claims management aspects for the life of a claim:
(a) proactively support the claimant to optimise their recovery and return to work or other activities
(b) make decisions justly and expeditiously
(c) act objectively with honesty and professionalism at all times
(d) detect and deter fraud
(e) communicate with the claimant and keep them informed of the progress of their claim
(f) take into account the health emergency caused by the COVID-19 pandemic on a claimant’s circumstances when making decisions about a claim, including decisions related to disputes, and the claimant’s ability to comply with obligations or timeframes under the Act, regulations or these Guidelines.
4.7 If an insurer does not deal with claims in a manner consistent with these principles, the Authority will take appropriate action as per the Authority’s compliance and enforcement strategy.
4.8 In circumstances where more than one insurer is involved in the management of a claimant’s statutory benefits claim and/or damages claim, the insurers must:
(a) proactively and regularly share information with each other
(b) promptly respond to requests from each other
(c) ensure the claimant understands which insurer will be managing each aspect of the claim process and the reasons why
(d) work collaboratively to ensure a consistent and seamless claim experience for the claimant.
Communication with claimants
4.9 When communicating with claimants, insurers must:
(a) communicate directly with the claimant to deal with the claim, regardless of whether the claimant is legally represented, unless the clause below applies
(b) where a friend assists the claimant with the claim, communicate directly with that friend instead of, or in addition to, the claimant, as appropriate, regardless of whether the claimant is legally represented
(c) if requested in writing to do so by the claimant, friend or the claimant’s legal representative, copy the claimant’s legal representative into all written correspondence
(d) in this clause: friend means a person, including a family member, who is assisting the claimant with the claim and has authority from the claimant to give and receive information about the claim. It does not include a legal representative acting on instructions. The claimant can revoke the authority at any time by notifying the insurer or can limit the friend’s authority to a specified timeframe.
4.10 If a dispute arises between the insurer and a legally represented claimant and is before the Personal Injury Commission, the insurer is not to communicate with the claimant directly about the dispute and must communicate only with the claimant’s legal representative.
Making a statutory benefits claim
Verifying motor accident
4.11 As per Division 6.3, section 6.8 of the Act, to verify a motor accident before making a claim for statutory benefits, a claimant should:
(a) report the accident to the NSW Police Force within 28 days after the accident, unless a police officer attended the motor accident, and
(b) provide the accident event number from the NSW Police Force to the insurer if available.
4.12 If a claimant cannot provide the accident event number, the insurer must request other information from the claimant to verify the motor accident. Information requested may include:
(a) photographs taken at the scene of the accident
(b) witness statements
(c) a hospital discharge summary
(d) media reports
(e) property damage insurance claim information
(f) CCTV or dashcam footage.
4.13 If the claimant cannot provide the information requested by the insurer, they must provide a statutory declaration explaining why. It should include whether or not the NSW Police Force provided an accident event number.
4.14 Division 6.3, section 6.9 of the Act provides for the circumstances in which a claim may be dealt with even though the claimant has not met the above requirements.
Time for making a statutory benefits claim
4.15 As per Division 6.3, section 6.12 and section 6.13 of the Act, to make a claim for statutory benefits, a claimant must give notice of the claim to the relevant insurer within the following timeframes:
(a) three months after the date of the motor accident to which the claim relates, or
(b) to be entitled to receive weekly payments of statutory benefits from the day after the date of the motor accident, within 28 days after the date of the accident.
4.16 Where the at-fault vehicle is unidentified or uninsured, a statutory benefits claim must be made on the Nominal Defendant within 28 days after the date of accident to be entitled to receive weekly payments of statutory benefits from the day after the date of the motor accident.
4.17 If a claim is made on the CTP insurer of the vehicle alleged to be at fault in the accident and the CTP insurer is not a licenced insurer under the Act, the insurer must notify the Authority of the claim as soon as possible.
Notice of a statutory benefits claim
4.18 As per Division 6.3, section 6.15(1)-(3) of the Act, a claimant can give notice of a claim either:
(a) online using the online claims submission system operated by the NSW government,
(b) in writing using the claim form available on the Authority’s website and sent to the insurer by email, personal delivery, facsimile or post or
(c) online using an online claims submission system operated by the insurer.
4.19 The notice must be given in the following manner and must contain the following information:
(a) For notice of a claim for statutory benefits for a personal injury claim using:
- the CTP Green Slip claim form – Application for personal injury benefits containing the information relevant to the claim as set out in Table 4.1 of Schedule 4.1, or
- the CTP Green Slip claim form – Online Application for Personal Injury Benefits containing the information relevant to the claim as set out in Table 4.2 of Schedule 4.1, or
- if submitted online using a claims submission system operated by the insurer - a form containing the information relevant to the claim as set out in Table 4.2 of Schedule 4.1.
(b) For notice for a claim for statutory benefits for funeral expenses using:
- the CTP Green Slip claim form – Application for funeral expenses containing the information relevant to the claim as set out in Table 4.3 of Schedule 4.1, or
- if submitted online using a claims submission system operated by the insurer - a form containing the information relevant to the claim as set out in Table 4.3 of Schedule 4.1.
(c) If the insurer wishes to use its online claims submission system to collect additional information that is not included in Table 4.2 or Table 4.3 of Schedule 4.1, it must first seek approval from the Authority.
4.20 A claimant must provide a signed authority within the claim form authorising the insurer to release information and documents to relevant parties, and obtain information and documents relevant to the claim.
4.21 In claims for personal injury, a claimant must also provide a certificate from a treating medical practitioner such as a Certificate of Fitness.
4.22 A licensed insurer must enable a notice of claim for statutory benefits for personal injury to be received electronically in the following manner:
(a) as a single transfer of data from the NSW government’s online claims submission system directly to the insurer’s Electronic claims-handling system, or
(b) as a transfer of data to the Insurer portal, but only if the Authority grants permission to the insurer for a specified period of time.
For the purposes of this clause:
- Electronic claims-handling system means an electronic system designed to enable an insurer to hold information about CTP claims made on it.
- Insurer portal means the system maintained by the NSW Government which insurers can use to download attachments submitted by claimants (including the claim summary PDF form) and to enable the making of a claim.
4.23 If a claimant gives a notice of claim via the online claims submission portal, the notice must be made available electronically to the insurers when the claimant (or their representative) receives an email notification and reference number confirming a successful transmission.
4.24 If a claimant contacts the insurer by phone and provides the required details, the insurer must send a pre-filled claim form to the claimant for their review and declaration that the information is correct. Notice of the claim is not given until the completed form is returned to the insurer.
4.25 The insurer must acknowledge the date of receipt of the claimant’s claim form, the assigned claim number and the dedicated insurer contact assigned to manage the claim, in the communication method preferred by the claimant.
4.26 In accordance with Division 6.3, section 6.15(4) of the Act, if notice of a claim has been given to an incorrect insurer and the claim must be transferred to the relevant insurer, the claimant is excused from giving notice of a claim to the relevant insurer. The insurers must cooperate so that the necessary information is exchanged, and the claimant’s recovery and benefits are not adversely affected.
Sharing Agreements
4.27 If more than one vehicle is involved in the accident and the insurers agree to share the claims between or among themselves, a relevant insurer will be nominated by the insurers to manage the claims on behalf of all the insurers.
4.28 Until the relevant insurer has been nominated, the insurers on whom the claims are made must continue to manage the claims.
4.29 When the relevant insurer has been agreed to and appointed, the insurers on whom the claimant has made a claim must each immediately write to the claimant and inform the claimant:
(a) that the sharing agreement has been applied
(b) the name, contact details and reference number of the relevant insurer
(c) the role of the relevant insurer in managing all the claims,
(d) and provide a copy of this notice to the relevant insurer.
4.30 Insurers must communicate in a clear and timely manner and give sufficient information to enable the claimant to progress the claim, including where the sharing agreement is relevant. The insurer must not require the claimant to gather evidence as to fault or as to other matters that are not needed in the circumstances. Any sharing disputes between insurers must not impede the delivery of statutory benefits to the claimant.
4.31 If the claim is transferred after resolution of the dispute, the insurer must contact the claimant and advise the reasons for the transfer of the claim and the date of the official transfer. Notice of the transfer must be given to the claimant by all insurers within two days of the transfer.
Liability decisions in a statutory benefits claim
4.32 Acceptance of liability for a claim for statutory benefits is detailed in section 6.19 of the Act.
4.33 The insurer must give written notice to the claimant to confirm if the insurer accepts or denies liability for the payment of statutory benefits, including when the decision will take effect and how it will take effect (for example, weekly payments will be paid fortnightly for a specific amount each week).
4.34 The notice must include:
(a) an explanation of why the insurer must determine liability
(b) an explanation of the consequences of the decision, including any effects on the claimant’s entitlement to statutory benefits or damages
(c) the reasons why the insurer has made the decision with reference to the information relied upon in making the decision (where the insurer denies liability on the basis of fault, the insurer must include its assessment of contributory negligence and threshold injury)
4.35 If the insurer denies liability for all or part of the claim for statutory benefits, the notice must also include:
(a) where the insurer declines the payment of statutory benefits on the basis that the claimant’s injury was not caused by the motor accident, an explanation of which injury the insurer asserts is not covered and why
(b) a list of all information relevant to the decision, regardless of whether the information supports the decision, including copies of all listed information
- if the claim for statutory benefits is related to a death, vulnerable person or psychological injury, insurers should apply their discretion in identifying and withholding potentially traumatising information. Where a claim for statutory benefits is identified as related to a vulnerable person the insurer should outline the reasons for such an identification clearly on the file.
(c) an explanation of the insurer’s internal review process, including the timeframe in which an application for internal review must be made and/or right to make an application to the Personal Injury Commission
(d) the claimant’s right to seek independent legal advice
(e) information on how a claimant may make a complaint with the Independent Review Office (IRO), including the IRO’s contact details.
4.36 The insurer must give notice as follows:
(a) for statutory benefits during the first 52 weeks after the accident:
- clearly identified as ‘Liability Notice – benefits up to 52 weeks’
(b) for statutory benefits after the first 52 weeks after the accident:
- clearly identified as ‘Liability Notice – benefits after 52 weeks’.
(c) if the insurer is wholly denying liability for payment of statutory benefits during the first 52weeks after the accident, and wishes at the same time to notify the claimant of its decision regarding liability for benefits after 52weeks:
- clearly identified as Combined Liability Notice, and containing two sections titled ‘Liability Decision - benefits up to 52 weeks’ and ‘Liability Decision- benefits after 52 weeks ‘
- the section ‘Liability Decision - benefits up to 52 weeks’ must contain all the information required under clauses 4.34 and 4.35
- the section ‘Liability Decision- benefits after 52 weeks’ must contain all the information required for a notice under clause 4.34.
4.37 Where a claimant is legally represented, the insurer must provide the claimant’s legal representative with a copy of the liability notice at the same time notice is provided to the claimant.
4.38 If the insurer denies liability in whole or in part for the payment of statutory benefits, the insurer must also provide to the legal representative copies of all information provided to the claimant with the notice.
4.39 Where the vehicle considered at fault was registered under the law of a place other than NSW, the NSW insurer managing payment of statutory benefits on behalf of the Nominal Defendant must provide a copy of the liability notice to the insurer of the vehicle considered at fault when the initial liability decision is made and each subsequent liability decision made under section 6.19 including Liability Notice – benefits after 52 weeks.
4.40 If the insurer denies liability and issues a notice to the claimant, the insurer must inform the service provider when responding to any treatment and care requests that treatment and care benefits may not be available after 52 weeks.
4.41 If the claimant is a participant (interim or lifetime) in the Lifetime Care & Support Scheme, the insurer must provide the Lifetime Care & Support Authority with a copy of the Liability Notice – benefits after 52 weeks at the same time the notice is given to the claimant.
4.42 If the insurer is considering ceasing, reducing or suspending weekly payments of statutory benefits to a claimant who is a participant in the Lifetime Care & Support Scheme, the insurer must notify the Lifetime Care and Support Authority of NSW before the decision is made and briefly explain the basis of the decision.
New information relevant to a liability decision
4.43 If at any time an insurer receives new information relevant to its liability decision, the insurer must:
(a) ensure the claimant has a copy of the new information
(b) ask the claimant for any other relevant information not previously provided
(c) review the liability decision and notify the claimant of the outcome of the review within 21 days after it has received all relevant information
(d) if the new information causes the insurer to change its liability decision, issue a new liability decision in writing
(e) if the change results in a denial of liability in whole or in part, the new decision must address the matters set out in the section ‘Liability decisions in a statutory benefits claim’ in this Part of the Guidelines.
Weekly payments decisions
4.44 After an insurer accepts liability for statutory benefits, weekly payments may be payable to a claimant. The insurer must commence weekly payments of statutory benefits as soon as possible and in any event within 10 working days after its decision to accept liability.
4.45 Division 3.3 and Schedule 1 of the Act provide for Guidelines to be made in relation to:
(a) the first 13 weeks – interim payment (i.e. where pre-accident weekly earnings cannot yet be determined)
(b) earning capacity decisions
(c) student pre-accident weekly earnings.
First 13 weeks – interim payment
4.46 The interim payment amount referred to in section 3.6(5) of the Act is calculated at 12.5% of the maximum weekly statutory benefits amount set out in section 3.9 unless the claimant nominates a lower amount.
4.47 The insurer and claimant may negotiate payment of a higher interim rate at the discretion of the insurer.
4.48 If the correct amount of weekly payments is determined as being higher than the interim rate, the insurer must pay any difference owing within 10 business days.
4.49 If the correct amount of weekly payments is determined as being lower than the interim rate, the insurer should consider the amount of overpayment and the financial position of the claimant when identifying a means of recovery of overpayment.
Earning capacity decisions
4.50 Division 3.3, section 3.16(1)-(2) of the Act refers to decisions about earning capacity.
Decision-making principles
4.51 An insurer may follow its own procedures in connection with an earning capacity decision, but the procedures must align with the following principles and legal requirements:
(a) insurers comply with statutory duties
(b) claimants are given procedural fairness
(c) communication is in plain language
(d) insurers fix errors promptly.
Statutory duties
4.52 The procedures to be followed in connection with a decision about a claimant’s earning capacity must comply with the insurer’s statutory duty to act with good faith under Division 6.2 of the Act.
Procedural fairness
4.53 An insurer must give a claimant procedural fairness when it makes a decision about that person’s pre-accident earning capacity or post-accident earning capacity. In addition to the statutory duties, this includes:
(a) giving the person a fair opportunity to give information to the insurer to consider for the decision
(b) ensuring the decision-maker is not, or is not reasonably perceived to be, biased toward a particular outcome
(c) providing the person with all the information the insurer is considering in making its decision, regardless of whether that information supports the decision
(d) giving the claimant a right of response, including the right to provide new relevant information held by the claimant within a reasonable time in respect of an earning capacity decision that may adversely affect them.
4.54 If the claimant is a participant in the Lifetime Care & Support Scheme, the insurer must consult the Lifetime Care & Support Authority before any potential adverse decision.
Plain language
4.55 An insurer must give information about all decisions to a claimant in plain language. This means a claimant must be able to easily find, understand and use the information they need.
Correcting errors
4.56 An insurer must correct any errors in its decisions about a claimant’s pre-accident earning capacity or post-accident earning capacity promptly after it becomes aware of the error, including after the decision has been made. An insurer is responsible for having procedures in place to fix an error of fact or law.
4.57 If an error can be corrected, the insurer must correct the error and not require a claimant to make an application for internal review or an application to the Personal Injury Commission.
Student pre-accident weekly earnings
4.59 In making a decision regarding a student’s pre-accident weekly earnings, the matters to be considered in determining the weekly earnings that the person would have received upon being employed on the completion of the course of studies in which the person was a full-time student include:
(a) the course of study being undertaken
(b) pre-accident academic results
(c) published wage data for new graduates relevant to the course undertaken
(d) previous work experience
(e) Australian Bureau of Statistics (ABS) data for age and industry
(f) the individual circumstances of the claimant
(g) any other relevant circumstances.
Post-accident earning capacity (after 78 weeks)
4.60 When determining employment reasonably available to a claimant at any time after the second entitlement period (from week 79 after the motor accident), the matters to be considered include:
(a) the nature and extent of the claimant’s injuries
(b) the claimant’s age, education, skills and work experience
(c) rehabilitation services that are being or have been provided
(d) the nature of the claimant’s pre-injury employment
(e) the claimant’s place of residence at the time of the motor accident
(f) the details given in the claimant’s Certificate of Fitness
(g) the length of time the claimant has been seeking employment
(h) any other relevant circumstances.
Non-compliance with providing evidence of fitness for work
4.61 Before an insurer can suspend weekly payments for failure of the claimant to comply with requirements for evidence as to fitness for work, the insurer must:
(a) contact the claimant (via the claimant’s preferred method of communication) to ensure that the claimant is aware of their duty to provide this evidence
(b) clearly state to the claimant the consequences of not providing the evidence
(c) provide the claimant with a reasonable time within which to comply
(d) if the claimant is a participant in the Lifetime Care & Support Scheme, the insurer must contact the Lifetime Care & Support Authority of NSW before any potential adverse decision is made
(e) provide the claimant with contact details of the Authority.
4.62 If the claimant continues to fail to comply without a reasonable excuse, a suspension notice giving the claimant seven calendar days to comply must be sent in writing.
4.63 The suspension notice must clearly state the insurer’s reasons for suspending weekly payments, actions the claimant must take to avoid suspension of their weekly payments and the claimant’s rights of review. A copy of this notice must be provided to the claimant’s legal representative where the claimant is legally represented.
Notice before benefits discontinued or reduced
4.64 If a decision is made to discontinue or reduce weekly payments, the insurer must give the required period of notice before that decision takes effect, in accordance with Division 3.3, section 3.19 of the Act.
4.65 Notice may be given verbally but must also be given in writing and delivered by electronic or postal means, using the claimant’s preferred method of delivery. The notice must include:
(a) information about the claimant’s rights of review of the insurer’s decision
(b) contact details of the Authority.
4.66 A copy of this notice must be provided to the claimant’s legal representative where the claimant is legally represented.
Claimant’s responsibilities for ongoing weekly payments
Evidence of fitness for work
4.67 A claimant must provide to the insurer a certificate of fitness for work to be eligible for weekly payments. The required form of a certificate given under section 3.15(3) of the Act is a Certificate of Fitness (including the declaration of employment).
4.68 The first certificate of fitness for work must be given by the claimant’s treating medical practitioner.
4.69 A second or subsequent certificate of fitness must be in a form approved by the Authority and given by:
(a) a medical practitioner, or
(b) if the injured person is receiving medical or related treatment for the injury by a physiotherapist or psychologist who is appropriately qualified — the physiotherapist or psychologist.
- In this clause, an appropriately qualified physiotherapist or psychologist is one with general registration under the Health Practitioner Regulation National Law (NSW) No 86a.
(c) If a subsequent certificate covers a period that overlaps wholly or in part with a period covered by an earlier certificate, the later certificate prevails for the whole of the period covered by the later certificate except to the extent that the later certificate relates to a period before the later certificate was provided.
(d) The insurer that receives a certificate of fitness for work given by a physiotherapist or psychologist must, as soon as possible after receiving the certificate, give a copy of the certificate to the injured person’s treating medical practitioner.
Change in circumstances
4.70 A claimant must notify an insurer of a change in circumstances, in accordance with Division 3.3, section 3.18(1)–(2) of the Act. Initial notice may be given verbally; however, notice must also be given in writing, which may include documentary evidence, such as payslips or certificates of fitness for work depending on the change notified. If requested, other documentary evidence or written notice must be provided to the insurer as soon as possible by the claimant.
Residing outside of Australia
4.71 Division 3.3, section 3.21(1)–(2) of the Act outlines details for weekly statutory benefits to claimants residing outside Australia. The claimant must submit a Certificate of Fitness (including declaration of employment) from a treating medical practitioner every three months to establish their identity and continued loss of earnings.
Minimising loss
4.72 The claimant must do all such things as may be reasonable and necessary for their rehabilitation.
4.73 If the claimant does not take all reasonable steps to minimise loss caused by the injury resulting from the motor accident as per Division 6.2, section 6.5(1)–(3) of the Act, the insurer is authorised to suspend weekly payments in writing, but only if the insurer contacts the claimant to ensure that the claimant:
(a) is aware of their duty to minimise loss
(b) understands what is expected of them to comply with the duty
(c) understands the consequences of failing to comply
(d) has had a reasonable opportunity to comply
(e) has the Authority’s contact details.
4.74 If the insurer considers that the claimant has had a reasonable opportunity to comply with the duty but has failed to do so, a suspension notice giving the claimant 14 days to comply must be given.
4.75 The duties of the claimant must be defined in the notice. The insurer may provide notice by phone or in person; however, the notice must be confirmed in writing to the claimant.
4.76 Insurers must contact the Lifetime Care & Support Authority before making adverse decisions regarding compliance for those claimants engaged in the Lifetime Care & Support Scheme or with severe injuries.
Treatment, rehabilitation, care and vocational support
Treatment before a claim is made
4.77 The insurer may approve access to treatment before a claim is made but after notification of injury has been given. This may also apply where a notice of claim has not included all required information and documents and the insurer is waiting for further information from the claimant.
4.78 Any treatment approved before a claim is made is approved at the insurer’s discretion and will only be approved within the first 28 days from the date of the motor accident. However, if further treatment is required after 28 days, a claim for statutory benefits must be made by the injured person. The insurers’ and claimants’ obligations about treatment, rehabilitation and vocational training are detailed in Division 3.3, section 3.17 and Division 6.2, section 6.5(1)–(3) of the Act.
Recovery plans
Recovery approach
4.79 People respond differently after a motor accident injury. The insurer must manage claims in a manner that is tailored to the claimant’s individual circumstances and needs, providing support based on best practice and a commitment to early and appropriate treatment and care.
4.80 The insurer should apply the principles of the nationally endorsed Clinical Framework for the Delivery of Health Services, which sets out five guiding principles for consideration by health professionals and insurers when reviewing treatment plans and requests for services:
(a) measure and demonstrate the effectiveness of the treatment
(b) adopt a biopsychosocial approach – consider the whole person and their individual circumstances
(c) empower the injured person to manage their recovery
(d) implement goals focused on optimising function, participation and return to work or other activities
(e) base treatment on the best available research evidence.
4.81 Consideration for service requests should also include Guidelines developed by the Authority, for example:
(b) the Neuropsychological Assessment of Children & Adults with Traumatic Brain Injury Guidelines.
Screen and assess risk of poor recovery
4.82 A claimant must be screened initially for risk of poor recovery and opportunities for early intervention within three business days of lodgement of their claim. This must include direct contact with the claimant where available and consideration of recent information by the treating doctor. The outcome of this screening must be recorded on the claimant’s file.
4.83 Where a claimant is identified to be at or above a medium risk of poor recovery, the insurer must take action to support the claimant through the appropriate internal claims management stream. The insurer should conduct a comprehensive assessment to determine the relevant actions to address identified risks. The outcome of this assessment must be integrated into the claimant’s recovery plan.
4.84 The insurer should regularly engage with the claimant and stakeholders involved to review progress and continue to assess and address risk of poor recovery. The outcome must be recorded on the claimant’s file and integrated into the recovery plan.
4.85 The insurer must screen for and identify claims where an injured person is psychologically vulnerable and, if such a risk is identified, promptly facilitate appropriate support.
(a) Where this risk is only identified after a recovery plan has been implemented, the insurer must update the recovery plan at the earliest possible opportunity.
Recovery plan
4.86 All claimants must have a tailored recovery plan with the following exceptions:
(a) where the claimant is performing their pre-injury duties
(b) where the claimant is performing their usual activities
(c) where the claimant is part of the Lifetime Care & Support Scheme
(d) where the claim is denied
(e) where a claimant has returned to their pre-injury duties and activities within 28 days of the claim being made.
4.87 The recovery plan will include intervention related to treatment and the injured person’s return to work and activity goals. The recovery plan may simply monitor treatment progress. It need not incorporate return to work support or vocational retraining where full return to work or other activities has been achieved.
4.88 The recovery plan must be established, in consultation with the:
(a) claimant who has an obligation under the Act to minimise loss and participate in reasonable and necessary treatment and care and rehabilitation
(b) recent status of the claimant from the claimant’s treating doctor
(c) claimant’s employer, where the claimant has authorised contact with the employer and the employer elects to be part of recovery, and to the maximum extent that their cooperation and participation allows
(d) any treating clinicians or therapists as appropriate.
4.89 An insurer must identify vocational support needs to support recovery at work and as far as possible, ensure that any vocational support provided or arranged under an individual’s recovery plan is reasonable and necessary to support the claimant’s return to work or other activities.
4.90 An insurer must fulfil its obligations under any recovery plan they have established for a claimant.
4.91 The recovery plan must be:
(a) developed in consultation with the claimant
(b) completed within 28 days of the claim being made or within 28 days of the claimant’s initial discharge from hospital in circumstances where the claimant has been admitted to hospital within two days of the date of the motor accident and remained in hospital for a period of not less than three continuous weeks, whichever is the later
(c) reviewed no less than at 12 weekly intervals or as pertinent changes occur
(d) followed up with the claimant regularly.
4.92 Where a claimant fails to comply with a recovery plan that has been developed with and provided to them, the insurer must provide notice to the claimant that weekly payments may be suspended during the period of non‑compliance in terms of Division 3.3, section 3.17(2) of the Act. See Division 3.3, section 3.19 of the Act for required notice periods when discontinuing weekly payments.
Development of a recovery plan
4.93 When developing a personalised recovery plan with a claimant, an insurer must take into account:
(a) the nature of the injury and the likely process of recovery
(b) the claimant’s pre-accident employment and usual activities
(c) treatment and rehabilitation needs, including the likelihood that treatment or rehabilitation will enhance earning capacity and any temporary incapacity that may result from treatment
(d) any employment engaged in by the claimant after the accident
(e) any Certificate of Fitness provided by the claimant
(f) the claimant’s, education, literacy including English literacy, training, skills and experience
(g) the age of the claimant
(h) accessibility of services within the claimant’s residential area
(i) the injured person’s psychological capacity (for example, concentration, memory, perception, mood, fears) when developing a recovery plan.
(j) any other relevant matters including non-accident-related disability or illness and carer responsibilities.
Minimum requirements in recovery plans
4.94 Within the recovery plan that is developed with and sent to both the claimant and their nominated treating doctor, the following details must be included at a minimum:
(a) name of claimant
(b) claim number
(c) date of injury
(d) current need for treatment and care and psycho-social support, being provided (including vocational and community support where relevant)
(e) likely future need for treatment and care and psycho-social support , being provided (including vocational and community support where relevant)
(f) current fitness for work and/or usual activities
(g) expected fitness for work and/or usual activities with milestones
(h) obligations of the claimant
(i) consequences for the claimant if they do not adhere to the recovery plan
(j) contact details of the insurer representative
(k) what action the claimant can take if they disagree with the recovery plan.
4.95 The recovery plan may be provided to all stakeholders including treating practitioners as deemed appropriate.
Obligations of the claimant
4.96 The claimant must agree to participate in the recovery plan and must, when requested to do so by the insurer, nominate a treating medical practitioner who is prepared to participate in the development of and in the arrangements under, the recovery plan.
4.97 The claimant may change their nominated treating practitioner if required due to, for example, the claimant moving house or their doctor leaving the area. The claimant needs to advise the insurer of any change and the reasons for the change.
4.98 A medical practice may be nominated as a treating medical practitioner for the purposes of a recovery plan. Such a nomination operates as a nomination of the medical practitioners of the practice who may treat the claimant from time to time. A reference in this section to the nominated treating doctor is a reference to the medical practitioners of the practice.
4.99 The claimant must authorise their nominated treating medical practitioners to provide relevant information to the insurer for the purposes of a recovery plan.
Treatment and care decisions
Limits on treatment and care expenses
4.100 In terms of section 3.31(4) of the Act, the limit is the applicable Australian Medical Association (AMA) rates at the time the treatment/service is provided.
Facilitating referrals
4.101 An insurer who has identified a claimant requiring treatment, rehabilitation and attendant care services must facilitate referral to an appropriate treatment provider (including vocational provider, if appropriate) within 10 days, with the claimant’s agreement.
4.102 The insurer must refer the claimant to an appropriate service provider reasonably accessible to the claimant.
4.103 If the claimant expresses a preference for a particular provider, the insurer must facilitate the referral of the claimant to that provider subject to the insurer is satisfied as to the suitability of that provider. If the insurer determines that the claimant’s preferred service provider is not suitable, the insurer must notify the claimant of the reasons for its decision and refer the claimant to an appropriate service provider reasonably accessible to the claimant.
4.104 Wherever possible, the insurer must use rehabilitation providers with expertise in managing psychological injury if return to work or other activities is likely to be delayed by the impacts of a psychological injury.
Determining requests
4.105 If the insurer receives the claimant’s request for the payment of treatment or care services, it must make a decision and advise the claimant and relevant service provider in writing of its decision as soon as possible but no later than 10 days from receipt of the request, and
(a) if approved:
- state the costs the insurer has agreed to meet
- pay the account as soon as possible but within 20 days of receipt of an invoice or expense
- advise the claimant of the insurer’s obligation to pay all reasonable and necessary costs and expenses – including travel expenses to attend approved treatment, rehabilitation services or assessments, including all services or assessments conducted by a medical assessor of the Personal Injury Commission – as soon as possible (no later than 20 days after receiving the account or request for reimbursement).
(b) if declined, in whole or in part, provide:
- the reasons for the decision with reference to the information relied upon in making the decision.
- a list of all information relevant to the decision, regardless of whether the information supports the decision, including copies of all listed information
- an explanation of the insurer’s internal review process, including the timeframe in which an application for internal review must be made and/or right to make an application to the Personal Injury Commission
- information on how a claimant may make a complaint with the Independent Review Office (IRO), including the IRO’s contact details.
(c) if the insurer has made a decision to decline the payment of treatment and care because further information is required,
- notify the claimant or relevant service provider of what further information is required and give the claimant or service provider or both a reasonable opportunity to provide the information
- outline the steps the insurer has previously taken to obtain the information
4.106 If requested by the claimant or the claimant’s nominated treating doctor (subject to the claimant’s authority), the insurer must provide the nominated treating doctor with a copy of any decisions relevant to the claimant’s treatment and care. The claimant can revoke the authority at any time by notifying the insurer.
4.107 Unless otherwise requested by the claimant, the insurer must provide the claimant with copies of all correspondence with the claimant’s treating practitioner, or
(a) in respect of oral communication with the nominated treating doctor, the insurer is to give the claimant written notification of the date or dates of the communications, the matters discussed and the outcome of the communication.
Claims involving a death
4.108 Claims involving a death of a person must be managed in a proactive, respectful and sensitive manner
4.109 The insurer must prioritise the making of the liability decisions in these claims and the prompt payment of statutory benefits to minimise delay and uncertainty.
4.110 When the insurer is notified of a claim related to an accident in which a person has died, it must contact the claimant or their nominated representative without delay to advise them of the insurer’s role, as well as the availability of CTP Assist to support the process of making a claim.
4.111 (omitted).
Verification of expenses
4.112 Where an invoice is issued to the insurer directly from a treatment or care provider, the following should be included on the invoice:
(a) the claimant’s first and last name
(b) the claim number allocated by the insurer
(c) payee details
(d) the Medicare provider number, if relevant
(e) the Australian Business Number (ABN) of the provider
(f) the name of the medical practitioner or service provider
(g) the date of the service (the date of invoice must be on the day of or after last date of service listed on the invoice)
(h) the payment classification code from the Authority or AMA item number, where applicable
(i) the service cost for each payment classification code from the Authority or AMA item number, where applicable
(j) the service duration, where applicable.
4.113 These provisions do not apply to reimbursement for treatment and/or expenses to the claimant. These expenses should be reimbursed to the claimant by the insurer on provision of a receipt confirming the expenses incurred, where the insurer has provided pre-approval and/or the expenses are reasonable and necessary in the circumstances. Insurers should request details of regular service providers to establish direct billing and reimbursement between the insurer and provider to reduce the financial burden on the claimant.
Making a damages claim
Time for making a damages claim
4.114 Division 6.3, section 6.14 of the Act provides for the timeframes in which to make a claim for damages.
Request to concede degree of permanent impairment
4.115 When the insurer receives a request by the claimant to concede that the injured person’s degree of permanent impairment as a result of the injury caused by the motor accident is greater than 10%, the insurer must accept or decline the request and notify the claimant of this decision within 90 days of receipt.
4.116 The insurer must acknowledge the request within 14 days of receipt. The acknowledgement must include:
(a) any request for relevant information from the claimant required to make an assessment of the injured person’s degree of permanent impairment
(b) the due date for providing a decision, and the claimant’s right to request an internal review if the decision is not provided by this due date.
4.117 The notification of the insurer’s decision must include:
(a) the insurer’s reasons for its decision
(b) the claimant’s right to request an internal review of the decision.
4.118 If the insurer fails to either accept or decline the request and notify the claimant within 90 days, the insurer’s decision is taken as declining to concede that the injured person’s degree of permanent impairment is greater than 10%, and the claimant may request an internal review of that decision.
Late damages claims – specific requirements
4.119 If the insurer does not accept that the claimant’s explanation for the delay in lodging a claim is full and satisfactory, the insurer must explain the reasons for its decision, including informing the claimant of the matters or grounds upon which is does not consider the explanation to be full or satisfactory or both.
4.120 The insurer must not delay its investigation of the claim including each of the elements of liability on the basis that the claim is lodged late.
4.121 When exercising discretion relating to late claims (received by the insurer more than three years from the date of the accident or Nominal Defendant claims received by the Authority more than three years from the date of the accident), the insurer must act reasonably and in accordance with its duties to resolve claims justly and expeditiously. The insurer should not delay the progress of claims by relying on technical defences or minor procedural defects or irregularities.
Notice of a damages claim
4.122 A notice of a damages claim is made when an insurer receives a signed Application for Damages Under Common Law form and all information required within the Application for Personal Injury Benefits form.
4.123 The notice of claim must contain the following information:
(a) for a damages claim – the CTP Green Slip claim form – Application for damages under common law, containing the information relevant to the claim as set out in Table 4.5 of Schedule 4.1 (below)
(b) for notice for a compensation to relatives claim – the CTP Green Slip claim form - Application to compensate relatives containing the information relevant to the claim as set out in Table 4.4 of Schedule 4.1 (below).
4.124 A claimant must provide a signed authority with the notice of claim authorising the insurer to release information and documents to relevant parties and obtain information and documents relevant to the claim.
Liability decisions in a damages claim
4.125 When the insurer makes a determination of liability under section 6.20 of the Act, it must notify the claimant of its decision in writing. The notice must be clearly identified as a Liability Notice – Claim for damages, and must explain the insurer’s decision to admit or deny liability, including:
(a) whether its insured driver or owner owed the claimant a duty of care and whether they breached that duty
(b) whether the claimant suffered loss, injury or damage as a result of the insured’s breach of duty
(c) a reference to the nature and the source of the evidence that supports the allegation
(d) if liability is admitted for only part of the claim, sufficient detail to ascertain the extent to which liability is admitted with reference to the nature and the source of the evidence that supports the allegation
(e) if the insurer alleges contributory negligence, the degree of contributory negligence it says can be attributed to the injured person and the reasons for that allegation, with reference to the nature and the source of the evidence that supports the allegation
(f) an explanation of the consequences of the decision, including any effects on the claimant’s entitlements
(g) explanation of the review process, including the timeframe in which an application for review must be made
(h) explanation that the claimant may seek further information from the insurer or the Authority and/or a lawyer to understand the decision and rights of review.
4.126 The notice Liability Notice – Claim for damages must also contain copies of all the information relevant to the decision, regardless of whether the information supports the decision. The insurer must provide copies of all listed information to the claimant regardless of whether the information has previously been provided to the claimant.
(a) This requirement does not apply to a claim for damages under the Compensation to Relatives Act 1897 if the insurer admits liability for the claim.
Claimant failure to provide relevant particulars – damages claim
4.127 Under Division 6.4, section 6.26 of the Act, if a claimant has failed without reasonable excuse to provide the insurer with all relevant particulars of their claim within two years and six months, insurers may send a Direction to Provide Particulars form.
4.128 Before making a request for further information, the insurer must take into account all relevant information already available, including any information from a related statutory benefits claim.
Non-economic loss – specific requirements
4.129 The insurer must make decisions relating to non-economic loss based on all the available information and documents, consistent with the facts and in accordance with the law. For example, the insurer should concede an entitlement to non-economic loss when it is in possession of health service provider examination reports that indicate that a claimant’s WPI is greater than 10%.
4.130 The insurer must in every case, regardless of whether the claimant makes a damages claim for non-economic loss:
(a) clearly indicate that it has determined whether or not the claimant is entitled to non-economic loss
(b) when a claimant claims to be entitled to non-economic loss but the insurer disagrees, clearly explain the reasons and detail any medical information considered in the course of making its decision that the injured person’s degree of permanent impairment is not greater than 10%
(c) ensure that the explanation is sufficient to enable the claimant to make an informed decision about whether to accept the insurer’s decision
(d) where a claimant has sufficiently recovered to enable the claim to be quantified, and the insurer is unable to determine whether the claimant’s degree of permanent impairment is greater than 10%, refer the matter to the President of the Personal Injury Commission for assessment.
Reasonable offers of settlement and finalising claims
4.131 In acting to resolve a claim justly and expeditiously, insurers should continually review and identify whether a claimant who is eligible for economic and/or non-economic loss has sufficiently recovered to enable quantification of the claim, and if so, make a reasonable offer of settlement. A reasonable offer is one that is based on the facts and evidence, and is reflective of the injuries and losses the injured person has suffered as a consequence of the motor vehicle accident.
4.132 The insurer must make a reasonable offer of settlement to the claimant, as required by Division 6.4, section 6.22 of the Act, unless it wholly denies liability for the claim. The offer of settlement must be recorded on the claim file.
4.133 The insurer’s initial and final offer of settlement must:
(a) be set out in writing to the claimant (and copied to their legal representative where the claimant is represented)
(b) list amounts (including zero) offered for economic loss and non-economic loss separately or include a method for determining an amount of damages
(c) where the insurer admits liability for only part of the claim, include details necessary to determine the extent to which liability is admitted
(d) where applicable, identify as a separate amount any allowance for the claimant’s legal costs and disbursements
(e) where applicable, identify any deductions that have been made or are likely to be made, and how they have been determined or calculated
(f) include a reference to the insurer’s duty under the Act to make an offer of settlement on a damages claim.
4.134 Under section 6.23(2) of the Act, a damages claim cannot be settled until the Commission has approved it, unless the claimant is legally represented. Where the claimant is not legally represented, the insurer must proactively approach the Personal Injury Commission to have the settlement approved.
Confirming payment of a settlement amount
4.135 When a damages claim settles, the insurer must notify the claimant confirming:
(a) the total settlement amount
(b) to whom the payment has been made
(c) the method of payment (for example, cheque or EFT)
(d) the date the payment was made
(e) if the claimant has engaged legal representation, the insurer must also provide them with a copy of the correspondence.
Nominal Defendant claims
4.136 The insurer acting for the Nominal Defendant in a claim regarding an unidentified motor vehicle will explain to the claimant in writing that they are required to make due inquiry and search to ascertain the identity of the vehicle alleged to have been at fault in the accident.
4.137 The insurer will promptly advise the claimant in writing whether the claimant has, in the insurer’s view, satisfied the requirement for due inquiry and search, and:
(a) if the insurer determines that the requirement has not been met, it must provide details of the deficiency and how the claimant could go about satisfying the requirement.
4.138 In statutory benefits claims made on the Nominal Defendant, the insurer must make the liability decision within the timeframes specified under section 6.19(1)-(2) of the Act. If the insurer has not yet determined due inquiry and search at the time the liability decision is due, the insurer must inform the claimant in the notices of liability that it will make:
(a) a decision on whether due inquiry and search has been established
(b) a further liability decision once it is satisfied that due inquiry and search has been established.
4.139 The insurer will promptly advise the claimant in writing whether the claimant has, in the insurer’s view, satisfied the requirement for due inquiry and search.
4.140 An insurer’s decision must be based on all available information and should be consistent with the facts. Where the insurer alleges that the requirement has not been met, the insurer must include sufficiently detailed written reasons for its decision and details of the deficiency and manner by which the requirement could be satisfied by the claimant.
4.141 The insurer must perform as a model litigant in Nominal Defendant claims, which includes acting with complete propriety, fairly, and in accordance with the highest professional standards.
Investigations
4.142 The insurer should always consider whether investigations are required in the first instance and, if so, ensure that such investigations are appropriate with respect to the issues arising in the claim. The insurer must only undertake investigations when required information cannot be obtained by another less intrusive means.
4.143 If the insurer deems that an investigation is required, it must promptly investigate liability for a claim by requesting information and documents about the claim in a timely manner, and regularly following up any requests.
Factual Investigations
4.144 Factual investigations may be undertaken by or on behalf of the insurer to investigate and report on the circumstances of the motor accident and facts of the claim. Factual investigations may be used to gather information to assist the insurer in its management of the claim and making decisions about liability and the claimant’s entitlements to statutory benefits and damages. Factual investigations are not to provide an opinion on medical aspects of the claim.
4.145 If a factual investigation involves interview with a claimant, the factual investigation must comply with Part 15 of the Insurance Council of Australia’s ‘General Insurance Code of Practice’ (the Code) subject to the following modifications:
(a) clauses 194(c), 196, 197, 198, 199, 202(e), 203, 231(g), 232, 233, 234, and 235 do not apply to motor accident claims under the Act
(b) the maximum time for a single interview as referred to in clause 214 of the Code is to be read as 120 minutes not 90 minutes
(c) the Guidelines take precedence over the Code to the extent of any inconsistency.
4.146 Where the insurer engages an external investigator to conduct the investigation, it must ensure that the investigator holds a valid licence under the Commercial Agents and Private Inquiry Agents Act 2004 (NSW) 4, and conducts the investigation in compliance with that Act.
Surveillance
4.147 The insurer must conduct surveillance of the claimant only when there is evidence to indicate that the claimant is exaggerating an aspect of the claim or providing misleading information or documents in relation to a claim, or where the insurer reasonably believes that the claim is inconsistent with information or documents in the insurer’s possession regarding the circumstances of the accident or medical evidence.
4.148 The insurer must only conduct surveillance in places regarded as public or where the claimant, while on private property, is observable by members of the public going about their ordinary daily activities.
4.149 The investigator acting on behalf of the insurer must not actively interfere with the claimant’s activities while under observation or interact with the claimant so as to have an impact on their activities.
4.150 The insurer or investigator acting on behalf of the insurer must not engage in any acts of inducement, entrapment or trespass when carrying out factual investigations and/or surveillance activities. Inducement or entrapment can include social media activities such as sending friend requests with the intention to induce, entrap or deceive.
4.151 The insurer must be sensitive to the privacy rights of children, take reasonable action to avoid unnecessary video surveillance of children and, where possible, hide images of children in reports that contain still photographs of children. Persons who are under the age of 18 years are regarded as children.
4.152 Where the insurer sends surveillance material to a third party, it must inform that party about confidentiality and relevant privacy obligations.
4.153 The insurer must ensure that, where possible, investigation reports and recordings are redacted or censored to minimise the likelihood of uninvolved individuals being identifiable, and recordings and any other materials collected are securely stored.
4.154 Where the insurer becomes aware that a person has a mental health condition, surveillance of that person is only permitted if the insurer:
(a) clearly identifies any mental health conditions in the request for surveillance
(b) develops a risk management plan assessing the mental health conditions and identifying risk mitigation strategies that reduce the potential for impact on these conditions, and ensures that surveillance is conducted in line with this plan.
- Risk mitigation strategies may include, but are not limited to, restriction of mobile forms of surveillance and greater use of static or passive forms of surveillance, use of multiple investigators and/or increased rotation of investigators, consideration of investigator characteristics (e.g., gender), and reduction of surveillance hours.
- Note: Insurers have obligations under the Privacy Act 1988 (Cth) and the Health Records and Information Privacy Act 2002 (NSW) that must be complied with, including when undertaking investigations through surveillance.
Medical examinations
4.155 Before arranging a medical examination, the insurer must inquire with the injured person’s treating medical, rehabilitation and health service practitioners promptly to try to resolve the issue. The insurer must provide copies of all documents obtained in this process to the injured person as soon as possible (and in any event within 10 working days of receipt) unless the treating medical, rehabilitation or health service practitioner indicates otherwise.
4.156 The insurer should not arrange unnecessarily frequent examinations. The request to arrange a medical examination should be reasonable in the circumstances and, where applicable, the medical examination should be conducted by the same examiner who previously examined the claimant if they are available.
4.157 A claimant is required to comply with the insurer’s request to undergo a medical examination unless it is unreasonable, unnecessarily repetitious or dangerous. A request will ordinarily be considered reasonable if:
(a) the treating practitioner has not responded to a request for information from the insurer,
(b) information provided by the treating practitioner to the insurer is inadequate, or
(c) the insurer’s communication with the treating practitioner cannot resolve a dispute.
4.158 The insurer must retain evidence to support its decision to request a medical examination and provide this information to the Authority on request.
4.159 For the purpose of medical examinations, an insurer may use the Authorised Health Practitioners list on the Authority’s website to search for health practitioners who are authorised under Division 7.7, section 7.52(1)(b) of the Act to give evidence when required during the management of a claim.
4.160 If practitioners on the list are unavailable for an appointment within the required timeframes for the issues to be assessed, an independent medical examiner with availability chosen by the insurer or claimant may be proposed to the Authority for authorisation, following the guidelines prescribed in ‘Part 8 of the Motor Accident Guidelines’.
4.161 A rehabilitation service provider cannot be deemed a health practitioner with regard to Division 7.7, section 7.52 of the Act.
Schedule 4.1 CTP Green Slip Claim Forms
Table 4.1: Application for personal injury benefits
Form field | Form field | Form field |
|---|---|---|
Full name | Date of birth | Gender |
Interpreter language | Medicare number and reference number | Driver licence number |
Mobile phone number | Home phone number | Work phone number |
Email address | Home address | Contact preference |
Preferred contact time | Payment preference and details | Account name |
BSB | Account number | Have you ever made a CTP claim for injury |
Date of injury | Claim number | CTP insurer at time of injury |
Please provide your police event number | Date of the accident | Approximate time of accident |
Where did the accident occur | In the accident, were you the | In your own words, please describe (or draw) the motor vehicle accident you were involved in |
In your own words, please outline all injuries you received as a result of the accident you have described above | Details of all vehicles involved in the accident | What is the registration number of the car you believe to be most at fault |
Did you receive treatment at hospital after the accident | Name of the hospital where you were treated | Were you taken to hospital in an ambulance |
Have you been discharged from hospital | Date of discharge | Were you suffering an illness or injury affecting the same or similar parts of your body at the time of the accident |
Have you been away from work as a result of the accident | Length of time off work due to the accident | What was your employment status at the time of the accident |
What is your usual occupation | Please outline your earnings at the time of the accident (Please circle whichever time frame applies) | Please provide your/your employer’s company name |
Were you receiving Centrelink benefits at the time of the accident | Would you like us to obtain your wages information directly from your employer | Employer contact name |
Email address | Mobile phone number | Contact address (unit, street number, street name, suburb, state, postcode) |
I, (print name) | Claimant's declaration, authorisation and signature | Date |
Table 4.2: Online application for personal injury benefits
Form field | Form field | Form field |
|---|---|---|
Accident description | Accident location | Accident location description |
Accident postcode | Accident role | Accident role other |
Accident state | Accident street | Accident street number |
Accident suburb | Date of accident | Did the accident take place in NSW |
Police event number | Time of accident | At fault vehicle known |
Claimant agrees to continue (late claims) | Confirm most at fault vehicle details | Correct registration entered |
Description – most at fault vehicle information does not match | Enter name – final declaration | Enter name – initial declaration |
Existing claim number | Final declaration | Has claim number been provided |
Initial declaration | Registration of vehicle most at fault | State of registration known |
Submitter is claimant | Vehicles involved are known | Date of birth |
First name | Gender | Home address |
Home street address | Home suburb | Home state |
Home postcode | Home country | Employer phone number |
Home phone | Interpreter language | Last name |
Mobile phone | Preferred contact method | Preferred contact time |
Preferred email address (injured person) | Work phone | Away from |
Away from work due to accident | Away until | Previous illness or injury description |
Currently away from work | Earning period | Employee or self‑employed |
Employer company name | Employer contact address | Employer contact first name |
Employer street address | Employer suburb | Employer State |
Employer postcode | Employer country | Were you in this vehicle |
Employer contact last name | Employer contact email | Employment status at the time of accident |
Length of time off work | Occupation description | Permission to obtain wages directly from employer |
Receiving Centrelink benefits | Total earnings | Type of benefits received |
Injury description | Account name | Account number |
BSB | Driver license number | Medicare number |
Medicare reference number | Payment method | State of driver license |
Month of previous CTP claim | Year of previous CTP claim | Previous claim number |
Previous CTP claim | Previous CTP insurer | Previous CTP insurer |
Injury description | Previous illness or injury | Send correspondence to |
Nominated representative required | Representative email | Representative first name |
Representative language required | Representative last name | Representative phone |
Representative preferred contact time | Representative role | Representative role other |
Preferred submitter email address | Reason submitting | Submitter SNSW email address |
Submitter first name | Submitter is a nominated representative | Submitter last name |
Submitter phone | Submitter type | Submitter type other |
Ambulance service received | Ambulance used | Date of discharge |
Discharged from hospital | Hospital name | Treatment description |
Treatment received at hospital post accident | Approximate date of previous injury | Driver's email |
Driver's first name | Driver's last name | Driver's phone number |
Number of passengers | Number of passengers known | Registration number |
Vehicle make | Vehicle model | Vehicle state |
Vehicle year |
Table 4.3: Application for funeral expenses
Form field | Form field | Form field |
|---|---|---|
Full name | Date of birth | Gender |
Home address (unit, street number, street name, suburb, state, postcode) | Email address | Mobile phone number |
Home phone number (if applicable) | Work phone number (if applicable) | Contact preference |
Preferred contact time | If you need an interpreter, please tell us your preferred language | Full name of the deceased |
Date of birth | Date of death | Address of the deceased (unit, street number, street name, suburb, state, postcode) |
What is your relationship to the deceased | Please provide the police event number (e.g. E12345678) | Date of the accident |
Approximate time of accident | Where did the accident occur (e.g. corner, intersection, street, number/name, suburb, state) | In the accident, the deceased was the: driver/passenger/cyclist/ pedestrian/other |
Please provide a brief description of the accident. | Details of all vehicles involved in the accident | Registration |
Driver’s name and contact (e.g. phone, email) | Number of passengers | What is the registration number of the car you believe to be most at fault (if known) |
At-fault: Still being determined/I’m unsure | Funeral director name | Funeral director contact number |
How would you like to be reimbursed | Account name | BSB |
Account number | I, [Name] | Signature |
Table 4.4: Application to compensate relatives
Form field | Form field | Form field |
|---|---|---|
If you need an interpreter, please tell us your preferred language | Are you the executor/administrator of the person deceased Yes / No | If no, what is your relationship to the deceased |
Full name | Date of birth | Gender |
Mobile phone number | Home phone number (if applicable) | Work phone number (if applicable) |
Email address | Home address (unit, street number, street name, suburb, state, postcode) | Contact preference - mobile, email, home phone, work phone |
Preferred contact time | Are you representing or acting on behalf of the claimant identified above Yes / No | Full name |
Relationship to the claimant | Mobile phone number | Home phone number (if applicable) |
Work phone number (if applicable) | Contact address (unit, street number, street name, suburb, state, postcode) | Full name |
Date of birth | Gender | Medicare number and reference number (if known) |
Driver’s licence number (if known) | What is your relationship to the deceased | Date of the accident |
Please provide the police event number (e.g. E12345678) | Who was involved in the accident (Provide as much information as you can) | Were there any expenses or financial losses suffered by the deceased resulting from the accident in the time between the accident and the date of death (e.g. intensive care fees, lost wages) |
If yes, please outline these expenses or financial losses | If no, skip to next page | Registration number |
Driver’s name | Driver’s contact (e.g. phone, email) | Number of passengers |
Funeral director name | Funeral director contact number | If the claimant hasn’t been reimbursed for the cost of funeral expenses, please provide payment details. |
Direct deposit | Cheque | Account name |
BSB | Account number | Was the deceased employed at the time of the accident No / Yes |
What was the deceased’s employment status at the time of the accident | Company name | Employer’s phone number |
Standard weekly earnings of the deceased (include overtime, regular bonuses and commission) | Name of business | Type of business (e.g. building, accounting, optometry, childcare) |
Accountant’s name | Estimated earnings lost (weekly) | Accountant’s phone number |
Employer’s name | Employer’s address (unit, number, street, suburb, state, postcode) | Self-employed (go to next section) |
Retired/student | Was the deceased receiving any other form of income at the time of the accident | (e.g. investments, workers compensation, social security benefits or income protection payments) |
Prior to the accident, had the deceased person made any firm arrangements to stop work, start a new job, change duties, change working hours or earnings | If yes, please provide workers compensation insurer and claim number; Centrelink benefit number; disability or income protection policy insurer and policy number; details of investment bonds, stocks, property etc. | New job. If yes, please provide details of when the new arrangements were expected to start and the name of the proposed employer (if applicable). |
Dependant number | Full name | Relationship to the deceased |
Date of birth | Gender | Relationship to the deceased |
Describe how much financial support the deceased person provided the dependant each week. For example, consider money for board and allowances, food, clothing, housing services (housekeeping and childcare) rent, mortgage payments, car payments, car expenses, education expenses, health and medication expenses, utilities and entertainment. | Type of support. $ per week; how it was provided | Is the dependant employed |
Does the dependant have any other employment | Does the dependant have any other income (e.g. investments, pension, Centrelink, workers compensation, disability or income protection policy) | If yes, please provide employment details below |
If yes, please attach details of all other employers to this form | If yes, please describe what other kinds of income the dependant receives, including a weekly sum | Employer’s phone number |
Dependant’s weekly earnings at time of deceased’s death | Dependant’s weekly earnings at present | Employer’s name |
Employer’s address (unit, number, street, suburb, state, postcode) | Interpreter language | I, [name] |
Signature | Date |
Table 4.5: Application for damages under common law
Form field | Form field | Form field |
|---|---|---|
Full name | Date of birth | Gender |
Mobile | Home phone | |
Work phone | Email address | Home address (unit, street number, street name, suburb, state, postcode) |
Mobile phone number | Home phone number (if applicable) | Work phone number (if applicable) |
Contact preference | Preferred contact time | Medicare number and reference number |
Driver licence number (if applicable) | Direct deposit | Cheque |
Please provide your CTP claim number (if known) | Payment preference and details | Account name |
BSB | Account number | Claimant’s signature |
Interpreter language | I, (print name) | Signature |
Date |
Part 5 of the Motor Accident Guidelines: Threshold injury (Soft tissue and threshold psychological or psychiatric injuries)
Threshold Injury
Introduction
5.1 This Part of these Guidelines is made under the Motor Accident Injuries Act 2017 (NSW) (the Act), including sections 1.6(5), 3.31 and 10.2 of the Act with respect to:
(a) assessing whether an injury caused by the motor accident is a threshold injury for the purposes of the Act
(b) the approval of domestic services and home maintenance as appropriate treatment and care for soft tissue or threshold psychological or psychiatric injury or injuries.
5.2 Division 1.2, section 1.6 of the Act and Part 1, clause 4 of the Regulation provides the definition of a threshold injury.
Assessment for soft tissue and threshold psychological or psychiatric injuries
General provisions for assessment
5.3 The assessment will determine whether the injury related to the claim is a soft tissue injury or a threshold psychological or psychiatric injury caused by the motor accident.
5.4 Insurers should not require injured persons to undergo diagnostic imaging for the purpose of the insurer determining whether the injury related to the claim is a threshold injury. Diagnostic imaging is not considered necessary to assess threshold injury.
5.5 A diagnosis for the purpose of a threshold injury decision must be based on a clinical assessment by a medical practitioner or other suitably qualified person independent from the insurer.
5.6 The assessment of whether an injury caused by the accident is a threshold injury for the purposes of the Act should be based on the evidence available and include all relevant findings derived from:
(a) a comprehensive accurate history, including pre-accident history and pre-existing conditions
(b) a review of all relevant records available at the assessment
(c) a comprehensive description of the injured person’s current symptoms
(d) a careful and thorough physical and/or psychological examination
(e) diagnostic tests available at the assessment. Imaging findings that are used to support the assessment should correspond with symptoms and findings on examination.
Soft tissue assessment – injury to a spinal nerve root
5.7 In assessing whether an injury to the neck or spine is a soft tissue injury, an assessment of whether or not radiculopathy is present is essential.
5.8 Radiculopathy means the impairment caused by dysfunction of a spinal nerve root or nerve roots when two or more of the following clinical signs are found on examination when they are assessed in accordance with ‘Part 6 of the Motor Accident Guidelines: Permanent impairment’.
(a) loss or asymmetry of reflexes (see the definitions of clinical findings in Table 6.8 in these Guidelines)
(b) positive sciatic nerve root tension signs(see the definitions of clinical findings in Table 6.8 in these Guidelines)
(c) muscle atrophy and/or decreased limb circumference (see the definitions of clinical findings in Table 6.8 in these Guidelines)
(d) muscle weakness that is anatomically localised to an appropriate spinal nerve root distribution
(e) reproducible sensory loss that is anatomically localised to an appropriate spinal nerve root distribution.
5.9 Where the neurological symptoms associated with the injured person’s injury of the neck or spine do not meet the assessment criteria for radiculopathy, the injury will be assessed as a threshold injury.
Threshold psychological or psychiatric injury assessment
5.10 In assessing whether an injury is a threshold psychological or psychiatric injury, an assessment of whether a psychiatric illness is present is essential.
5.11 The assessment of whether a psychiatric illness is present must be made using the Diagnostic & Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), published by the American Psychiatric Association.
5.12 Where the symptoms associated with the injured person’s psychological or psychiatric injury do not meet the assessment criteria for a recognised psychiatric illness, with the exception of acute stress disorder and adjustment disorder, the injury will be considered a threshold injury.
Limits to domestic services and home maintenance
5.13 Domestic services and/or home maintenance may be approved as appropriate treatment and care for a person whose only injuries are threshold injuries if the domestic service and/or home maintenance is all of the following:
(a) required as a result of injuries caused by the accident
(b) required because the person has reduced fitness for domestic tasks
(c) reasonable and necessary in the circumstances
(d) required for tasks the person used to do before the accident
(e) safe and effective
(f) a properly verified expense as set out in Part 4 of these Guidelines.
Table 5.1: Domestic services and home maintenance availability
Weeks post the accident | Available hours |
|---|---|
1–4 | Up to 12 hours in total over the 4 weeks |
5–8 | Up to 8 hours in total over the 4 weeks |
9–52 | Up to 6 hours in total over the 44 weeks |
5.14 The domestic services and home maintenance limit of hours may be exceeded in agreement with the insurer where the injured person’s medical restrictions described in the certificate of fitness place a limit on the completion of pre-injury domestic tasks and responsibilities.
Part 6 of the Motor Accident Guidelines: Permanent impairment
Permanent impairment
Introduction
6.1 'Part 6 of the Motor Accident Guidelines: Permanent impairment' has been developed for the purpose of assessing the degree of permanent impairment arising from the injury caused by a motor accident, in accordance with Division 7.5, section 7.21, and clause 2 of Schedule 2 of the Motor Accident Injuries Act 2017(NSW)(the Act).
6.2 This Part of the Motor Accident Guidelines is based on the American Medical Association's Guides to the Evaluation of Permanent Impairment, Fourth Edition (third printing, 1995) (AMA4 Guides). However, in this Part of the Motor Accident Guidelines, there are some very significant departures from that document. A medical assessor undertaking impairment assessments for the purposes of the Act must read this Part in conjunction with the AMA4 Guides. This Part is definitive with regard to the matters it addresses. Where it is silent on an issue, the AMA4 Guides should be followed. In particular, chapters 1 and 2 of the AMA4 Guides should be read carefully in conjunction with clauses 6.1 to 6.46 of this Part. Some of the examples in the AMA4 Guides are not valid for the assessment of impairment under the Act. It may be helpful for medical assessors to mark their working copy of the AMA4 Guides with the changes required by this Part.
Application of these Guidelines
6.3 This Part of the Motor Accident Guidelines applies under the Act to the assessment of the degree of permanent impairment that has resulted from an injury caused by a motor accident on or after 1 December 2017.
6.4 For accidents that occurred between 5 October 1999 and 30 November 2017 (inclusive), the Motor Accident Permanent Impairment Guidelines apply, as amended or replaced from time to time, as published by the Authority
Causation of injury
6.5 An assessment of the degree of permanent impairment is a medical assessment matter under clause 2(a) of Schedule 2 of the Act. The assessment must determine the degree of permanent impairment of the injured person as a result of the injury caused by the motor accident. A determination as to whether the injured person's impairment is related to the accident in question is therefore implied in all such assessments. Medical assessors must be aware of the relevant provisions of the AMA4 Guides, as well as the common law principles that would be applied by a court (or the Personal Injury Commission) in considering such issues.
6.6 Causation is defined in the Glossary at page 316 of the AMA4 Guides as follows:
'Causation means that a physical, chemical or biologic factor contributed to the occurrence of a medical condition. To decide that a factor alleged to have caused or contributed to the occurrence or worsening of a medical condition has, in fact, done so, it is necessary to verify both of the following:
- The alleged factor could have caused or contributed to worsening of the impairment, which is a medical determination.
- The alleged factor did cause or contribute to worsening of the impairment, which is a non-medical determination.'
This, therefore, involves a medical decision and a non-medical informed judgement.
6.7 There is no simple common test of causation that is applicable to all cases, but the accepted approach involves determining whether the injury (and the associated impairment) was caused or materially contributed to by the motor accident. The motor accident does not have to be a sole cause as long as it is a contributing cause, which is more than negligible. Considering the question 'Would this injury (or impairment) have occurred if not for the accident?' may be useful in some cases, although this is not a definitive test and may be inapplicable in circumstances where there are multiple contributing causes.
Impairment and disability
6.8 It is critically important to clearly define the term impairment and distinguish it from the disability that may result.
6.9 Impairment is defined as an alteration to a person's health status. It is a deviation from normality in a body part or organ system and its functioning. Hence, impairment is a medical issue and is assessed by medical means.
6.10 This definition is consistent with that of the World Health Organisation's (WHO) International Classification of Impairments, Disabilities & Handicaps, Geneva 1980, which has defined impairment as 'any loss or abnormality of psychological, physiological or anatomical structure or function'.
6.11 Disability, on the other hand, is a consequence of an impairment. The WHO definition is 'any restriction or lack of ability to perform an activity in the manner or within the range considered normal for a human being'.
6.12 Confusion between the two terms can arise because in some instances the clearest way to measure an impairment is by considering the effect on a person's activities of daily living (that is, on the consequent disability). The AMA4 Guides, in several places, refer to restrictions in the activities of daily living of a person. Hence the disability is being used as an indicator of severity of impairment.
6.13 Where alteration in activities of daily living forms part of the impairment evaluation, for example when assessing brain injury or scarring, refer to the 'Table of activities of daily living' on page 317 of the AMA4 Guides. The medical assessor should explain how the injury impacts on activities of daily living in the impairment evaluation report.
6.14 Two examples may help emphasise the distinction between impairment and disability:
(a) the loss of the little finger of the right hand would be an equal impairment for both a bank manager and a concert pianist and so, for these Guidelines, the impairment is identical. But the concert pianist has sustained a greater disability.
(b) an upper arm injury might make it impossible for an injured person to contract the fingers of the right hand. That loss of function is an impairment. However, the consequences of that impairment, such as an inability to hold a cup of coffee or button up clothes, constitute a disability.
6.15 A handicap is a further possible consequence of an impairment or disability, being a disadvantage that limits or prevents fulfilment of a role that is/was normal for that individual. The concert pianist in the example above is likely to be handicapped by their impairment.
6.16 It must be emphasised, in the context of these Guidelines, that it is not the role of the medical assessor to determine disability, other than as described in clause 6.12 (above).
Evaluation of impairment
6.17 The medical assessor must evaluate the available evidence and be satisfied that any impairment:
(a) is an impairment arising from an injury caused by the accident, and
(b) is an impairment as defined in clause 6.9 (above).
6.18 An assessment of the degree of permanent impairment involves three stages:
(a) a review and evaluation of all the available evidence including:
- medical evidence (doctors', hospitals' and other health practitioners' notes, records and reports)
- medico-legal reports
- diagnostic findings
- other relevant evidence
(b) an interview and a clinical examination, wherever possible, to obtain the information specified in these Guidelines and the AMA4 Guides necessary to determine the percentage impairment
(c) the preparation of a certificate using the methods specified in these Guidelines that determines the percentage of permanent impairment, including the calculations and reasoning on which the determination is based. The applicable parts of these Guidelines and the AMA4 Guides should be referenced.
Permanent impairment
6.19 Before an evaluation of permanent impairment is undertaken, it must be shown that the impairment has been present for a period of time, and is static, well stabilised and unlikely to change substantially regardless of treatment. The AMA4 Guides (page 315) state that permanent impairment is impairment that has become static or well stabilised with or without medical treatment and is not likely to remit despite medical treatment. A permanent impairment is considered to be unlikely to change substantially (i.e. by more than 3% whole person impairment (WPI) in the next year with or without medical treatment. If an impairment is not permanent, it is inappropriate to characterise it as such and evaluate it according to these Guidelines.
6.20 Generally, when an impairment is considered permanent, the injuries will also be stabilised. However, there could be cases where an impairment is considered permanent because it is unlikely to change in future months regardless of treatment, but the injuries are not stabilised because future treatment is intended and the extent of this is not predictable. For example, for an injured person who suffers an amputation or spinal injury, the impairment is permanent and may be able to be assessed soon after the injury as it is not expected to change regardless of treatment. However, the injuries may not be stabilised for some time as the extent of future treatment and rehabilitation is not known.
6.21 The evaluation should only consider the impairment as it is at the time of the assessment.
6.22 The evaluation must not include any allowance for a predicted deterioration, such as osteoarthritis in a joint many years after an intra-articular fracture, as it is impossible to be precise about any such later alteration. However, it may be appropriate to comment on this possibility in the impairment evaluation report.
Non-assessable injuries
6.23 Certain injuries may not result in an assessable impairment covered by these Guidelines and the AMA4 Guides. For example, uncomplicated healed sternal and rib fractures do not result in any assessable impairment.
Impairments not covered by these Guidelines and the AMA4 Guides
6.24 A condition may present that is not covered in these Guidelines or the AMA4 Guides. If objective clinical findings of such a condition are present, indicating the presence of an impairment, then assessment by analogy to a similar condition is appropriate. The medical assessor must include the rationale for the methodology chosen in the impairment evaluation report.
Adjustment for the effects of treatment or lack of treatment
6.25 The results of past treatment (for example, operations) must be considered, since the injured person is being evaluated as they present at the time of assessment.
6.26 Where the effective long-term treatment of an injury results in apparent, substantial or total elimination of a physical permanent impairment, but the injured person is likely to revert to the fully impaired state if treatment is withdrawn, the medical assessor may increase the percentage of WPI by 1%, 2% or 3% WPI. This percentage must be combined with any other impairment percentage using the 'Combined values' chart (pages 322-324, AMA4 Guides). An example might be long-term drug treatment for epilepsy. This clause does not apply to the use of analgesics or anti-inflammatory drugs for pain relief.
6.27 For adjustment for the effects of treatment on a permanent psychiatric impairment, refer to clauses 6.222 to 6.224 under 'Mental and behavioural disorders' within this part of the Motor Accident Guidelines.
6.28 If an injured person has declined a particular treatment or therapy that the medical assessor believes would be beneficial, this should not change the impairment estimate. However, a comment on the matter should be included in the impairment evaluation report.
6.29 Equally, if the medical assessor believes substance abuse is a factor influencing the clinical state of the injured person, a comment on the matter should be included in the impairment evaluation report.
Adjustment for the effects of prostheses or assistive devices
6.30 Whenever possible, the impairment assessment should be conducted without assistive devices, except where these cannot be removed. The visual system must be assessed in accordance with clauses 6.242 to 6.243 in this Part of the Motor Accident Guidelines.
Pre-existing impairment
6.31 The evaluation of the permanent impairment may be complicated by the presence of an impairment in the same region that existed before the relevant motor accident. If there is objective evidence of a pre-existing symptomatic permanent impairment in the same region at the time of the accident, then its value must be calculated and subtracted from the current WPI value. If there is no objective evidence of the pre-existing symptomatic permanent impairment, then its possible presence should be ignored.
6.32 The capacity of a medical assessor to determine a change in physical impairment will depend upon the reliability of clinical information on the pre-existing condition. To quote the AMA4 Guides (page 10): 'For example, in apportioning a spine impairment, first the current spine impairment would be estimated, and then impairment from any pre-existing spine problem would be estimated. The estimate for the pre-existing impairment would be subtracted from that for the present impairment to account for the effects of the former. Using this approach to apportionment would require accurate information and data on both impairments.' Refer to clause 6.218 for the approach to a pre-existing psychiatric impairment.
6.33 Pre-existing impairments should not be assessed if they are unrelated or not relevant to the impairment arising from the motor accident.
Subsequent injuries
6.34 The evaluation of permanent impairment may be complicated by the presence of an impairment in the same region that has occurred subsequent to the relevant motor accident. If there is objective evidence of a subsequent and unrelated injury or condition resulting in permanent impairment in the same region, its value should be calculated. The permanent impairment resulting from the relevant motor accident must be calculated. If there is no objective evidence of the subsequent impairment, its possible presence should be ignored.
Psychiatric impairment
6.35 Psychiatric impairment is assessed in accordance with 'Mental and behavioural disorders' within this part of the Motor Accident Guidelines.
Psychiatric and physical impairments
6.36 Impairment resulting from a physical injury must be assessed separately from the impairment resulting from a psychiatric or psychological injury (see section 1.7(2) of the Act).
6.37 When determining whether the degree of permanent impairment of the injured person resulting from the motor accident is greater than 10%, the impairment rating for a physical injury cannot be combined with the impairment rating for a psychiatric or psychological injury.
Pain
6.38 Some tables require the pain associated with a particular neurological impairment to be assessed. Because of the difficulties of objective measurement, medical assessors must not make separate allowance for permanent impairment due to pain, and Chapter 15 of the AMA4 Guides must not be used. However, each chapter of the AMA4 Guides includes an allowance for associated pain in the impairment percentages.
Rounding up or down
6.39 Medical assessors must not round WPI values at any point of the assessment process. During the impairment calculation process, however, fractional values might occur when evaluating the regional impairment (for example, an upper extremity impairment value of 13.25%) and this should be rounded (in this case to 13%). WPI values can only be integers (not fractions).
Consistency
6.40 The medical assessor must use the entire gamut of clinical skill and judgement in assessing whether or not the results of measurements or tests are plausible and relate to the impairment being evaluated. If, in spite of an observation or test result, the medical evidence appears not to verify that an impairment of a certain magnitude exists, the medical assessor should modify the impairment estimate accordingly, describe the modification and outline the reasons in the impairment evaluation report.
6.41 Where there are inconsistencies between the medical assessor's clinical findings and information obtained through medical records and/or observations of non-clinical activities, the inconsistencies must be brought to the injured person's attention; for example, inconsistency demonstrated between range of shoulder motion when undressing and range of active shoulder movement during the physical examination. The injured person must have an opportunity to confirm the history and/or respond to the inconsistent observations to ensure accuracy and procedural fairness.
Assessment of children
6.42 The determination of the degree of permanent impairment in children may be impossible in some instances due to the natural growth and development of the child (examples are injuries to growth plates of bones or brain damage). In some cases, the effects of the injury may not be considered permanent and the assessment of permanent impairment may be delayed until growth and development is complete.
Additional investigations
6.43 The injured person who is being assessed should attend with radiological and medical imaging. It is not appropriate for a medical assessor to order additional investigations such as further spinal imaging.
6.44 There are some circumstances where testing is required as part of the impairment assessment; for example, respiratory; cardiovascular; ophthalmology; and ear, nose and throat (ENT). In these cases, it is appropriate to conduct the prescribed tests as part of the assessment.
Combining values
6.45 In general, when separate impairment percentages are obtained for various impairments being assessed, these must be combined using the 'Combined values' chart (pages 322-324, AMA4 Guides). This process is necessary to ensure the total whole person or regional impairment does not exceed 100% of the person or region (see page 53 of the AMA4 Guides for examples). Note, however, that in a few specific instances, for example for ranges of motion of the thumb joints (AMA4 Guides, page 16), the impairment values are directly added. Multiple impairment scores should be treated precisely as the AMA4 Guides or these Guidelines instruct.
Lifetime Care & Support Scheme
6.46 An injured person who has been accepted as a lifetime participant of the Lifetime Care & Support Scheme under section 9 of the Motor Accidents (Lifetime Care and Support) Act 2006 (NSW) has a degree of permanent impairment greater than 10%.
Upper extremity
Introduction
6.47 The hand and upper extremity are discussed in section 3.1 of Chapter 3 of the AMA4 Guides (pages 15-74). This section provides guidance on methods of assessing permanent impairment involving the upper extremity. It is a complex section that requires an organised approach with careful documentation of findings.
Assessment of the upper extremity
6.48 Assessment of the upper extremity involves a physical evaluation that can use a variety of methods. The assessment in this Part of the Motor Accident Guidelines does not include a cosmetic evaluation, which should be done with reference to 'Other body systems' within this part of the Motor Accident Guidelines and Chapter 13 of the AMA4 Guides.
6.49 The assessed impairment of a part or region can never exceed the impairment due to amputation of that part or region. For an upper limb, therefore, the maximum evaluation is 60% WPI.
6.50 Although range of motion appears to be a suitable method for evaluating impairment, it can be subject to variation because of pain during motion at different times of examination and/or a possible lack of cooperation by the person being assessed. Range of motion is assessed as follows:
(a) a goniometer should be used where clinically indicated
(b) passive range of motion may form part of the clinical examination to ascertain clinical status of the joint, but impairment should only be calculated using active range of motion measurements
(c) if the medical assessor is not satisfied that the results of a measurement are reliable, active range of motion should be measured with at least three consistent repetitions
(d) if there is inconsistency in range of motion, then it should not be used as a valid parameter of impairment evaluation (see clause 6.40 of these Guidelines)
(e) if range of motion measurements at examination cannot be used as a valid parameter of impairment evaluation, the medical assessor should then use discretion in considering what weight to give other available evidence to determine if an impairment is present.
6.51 If the contralateral uninjured joint has a less than average mobility, the impairment value(s) corresponding with the uninjured joint can serve as a baseline, and are subtracted from the calculated impairment for the injured joint only if there is a reasonable expectation that the injured joint would have had similar findings to the uninjured joint before injury. The rationale for this decision must be explained in the impairment evaluation report.
6.52 When using clause 6.51 (above), the medical assessor must subtract the total upper extremity impairment (UEI) for the uninjured joint from the total UEI for the injured joint. The resulting percentage UEI is then converted to WPI. Where more than one joint in the upper limb is injured and clause 6.51 is used, clause 6.51 must be applied to each joint.
6.53 Figure 1 of the AMA4 Guides (pages 16-17) is extremely useful to document findings and guide assessment of the upper extremity. Note, however, that the final summary part of Figure 1 (pages 16-17, AMA4 Guides) does not make it clear that impairments due to peripheral nerve injuries cannot be combined with other impairments in the upper extremities unless they are separate injuries.
6.54 The hand and upper extremity are divided into the regions of the thumb, fingers, wrist, elbow and shoulder. The medical assessor must follow the instructions in Figure 1 (pages 16-17, AMA4 Guides) regarding adding or combining impairments.
6.55 The measurement of radial and ulnar deviation must be rounded to the nearest 5° and the appropriate impairment rating read from Figure 29 (page 38, AMA4 Guides).
6.56 Table 3 (page 20, AMA4 Guides) is used to convert UEI to WPI. Note that 100% UEI is equivalent to 60% WPI.
6.57 If the condition is not in the AMA4 Guides it may be assessed using another like condition. For example, a rotator cuff injury may be assessed by impairment of shoulder range of movement or other disorders of the upper extremity (pages 58-64, AMA4 Guides).
Specific interpretation of the AMA4 Guides
Impairment of the upper extremity due to peripheral nerve disorders
6.58 If an impairment results solely from a peripheral nerve injury, the medical assessor must not evaluate impairment from sections 3.1f to 3.1j (pages 24-45, AMA4 Guides). section 3.1k and subsequent sections must be used for evaluation of such impairment. For peripheral nerve lesions, use Table 15 (page 54, AMA4 Guides) together with Tables 11a and 12a (pages 48-49, AMA4 Guides) for evaluation. Table 16 (page 57, AMA4 Guides) must not be used.
6.59 When applying Tables 11a and 12a (pages 48-49, AMA4 Guides), the maximum value for each grade must be used unless assessing complex regional pain syndrome (CRPS).
6.60 For the purposes of interpreting Table 11 (page 48, AMA4 Guides), abnormal sensation includes disturbances in sensation such as dysaesthesia, paraesthesia and cold intolerance. Decreased sensibility includes anaesthesia and hypoaesthesia.
Impairment of the upper extremity due to CRPS
6.61 The section, 'Causalgia and reflex sympathetic dystrophy' (page 56, AMA4 Guides) must not be used. These conditions have been better defined since the AMA4 Guides were published. The current terminology is CRPS type I (referring to what was termed reflex sympathetic dystrophy) and CRPS type II (referring to what was termed causalgia).
6.62 For a diagnosis of CRPS, at least eight of the following 11 criteria must be present:
(a) skin colour is mottled or cyanotic
(b) cool skin temperature
(c) oedema
(d) skin is dry or overly moist
(e) skin texture is smooth and non-elastic
(f) soft tissue atrophy (especially fingertips)
(g) joint stiffness and decreased passive motion
(h) nail changes with blemished, curved or talon-like nails
(i) hair growth changes with hair falling out, longer or finer
(j) X-rays showing trophic bone changes or osteoporosis
(k) bone scan showing findings consistent with CRPS.
6.63 When the diagnosis of CRPS has been established, impairment due to CRPS type I is evaluated as follows:
(a) rate the UEI resulting from the loss of motion of each individual joint affected by CRPS
(b) rate the UEI resulting from sensory deficits and pain according to the grade that best describes the severity of interference with activities of daily living as described in Table 11a (page 48, AMA4 Guides). The maximum value is not applied in this case (clause 6.59 above). The value selected represents the UEI. A nerve multiplier is not used;
(c) combine the upper extremity value for loss of joint motion (clause (a)) with the value for pain and sensory deficits (clause (b)) using the 'Combined values' chart (pages 322-324, AMA4 Guides).
(d) convert the UEI to WPI by using Table 3 (page 20, AMA4 Guides).
6.64 When the diagnosis of CRPS has been established, impairment due to CRPS type II is evaluated as follows:
(a) rate the UEI resulting from the loss of motion of each individual joint affected by CRPS
(b) rate the UEI resulting from sensory deficits and pain according to the methods described in section 3.1k (pages 46-56, AMA4 Guides) and Table 11a (page 48, AMA4 Guides)
(c) rate the UEI upper extremity impairment resulting from motor deficits and loss of power of the injured nerve according to the determination method described in section 3.1k (pages 46-56, AMA4 Guides) and Table 12a (page 49, AMA4 Guides)
(d) combine the UEI percentages for loss of joint motion (clause (a)), pain and sensory deficits (clause (b)) and motor deficits (clause (c)) using the 'Combined values' chart (pages 322-324, AMA4 Guides)
(e) convert the UEI to WPI by using Table 3 (page 20, AMA4 Guides).
Impairment due to other disorders of the upper extremity
6.65 Section 3.1m 'Impairment due to other disorders of the upper extremity, (pages 58-64, AMA4 Guides) should be rarely used in the context of motor accident injuries. The medical assessor must take care to avoid duplication of impairments.
6.66 Radiographs for carpal instability (page 61, AMA4 Guides) should only be considered if available, along with the clinical signs.
6.67 Strength evaluations and Table 34 (pages 64-65, AMA4 Guides) must not be used as they are unreliable indicators of impairment. Where actual loss of muscle bulk has occurred, the assessment can be completed by analogy, for example, with a relevant peripheral nerve injury. Similar principles can be applied where tendon transfers have been performed or after amputation reattachment if no other suitable methods of impairment evaluation are available.
Lower extremity
Introduction
6.68 The lower extremity is discussed in section 3.2 of Chapter 3 in the AMA4 Guides (pages 75-93). This section provides a number of alternative methods of assessing permanent impairment involving the lower extremity. A lower extremity worksheet may be included as provided in these Guidelines at Table 6.6. Each method should be calculated in lower extremity impairment percentages and then converted to WPI using Table 6.4 in these Guidelines.
Assessment of the lower extremity
6.69 Assessment of the lower extremity involves a physical evaluation that can use a variety of methods. In general, the method that most specifically addresses the impairment should be used. For example, impairment due to a peripheral nerve injury in the lower extremity should be assessed with reference to that nerve rather than by its effect on gait.
6.70 There are several different forms of evaluation that can be used as indicated in sections 3.2a to 3.2m (pages 75-89, AMA4 Guides). Table 6.5 in these Guidelines indicates which evaluation methods can and cannot be combined for the assessment of each injury. This table can only be used to assess one combination at a time. It may be possible to perform several different evaluations as long as they are reproducible and meet the conditions specified below and in the AMA4 Guides. The most specific method, or combination of methods, of impairment assessment should be used. However, when more than one equally specific method or combination of methods of rating the same impairment is available, the method providing the highest rating should be chosen. Table 6.6 can be used to assist the process of selecting the most appropriate method(s) of rating lower extremity impairment.
6.71 If there is more than one injury in the limb, each injury must be assessed separately and then the WPIs combined. For example, a fractured tibial plateau and laxity of the medial collateral ligament are separately assessed and their WPI combined.
6.72 If the contralateral uninjured joint has a less than average mobility, the impairment value(s) corresponding with the uninjured joint can serve as a baseline, and are subtracted from the calculated impairment for the injured joint, only if there is a reasonable expectation that the injured joint would have had similar findings to the uninjured joint before injury. The rationale for this decision must be explained in the impairment evaluation report.
6.73 The assessed impairment of a part or region can never exceed the impairment due to amputation of that part or region. For a lower limb, therefore, the maximum evaluation is 40% WPI.
6.74 When the ‘Combined values’ chart is used, the medical assessor must ensure that the values all relate to the same system (i.e. WPI or lower extremity impairment or foot impairment). Lower extremity impairment can then be combined with impairments in other parts of the body using the same table and ensuring only WPIs are combined.
6.75 Refer to Table 6.5 to determine which impairments can and cannot be combined.
Specific interpretation of the AMA4 Guides
Leg length discrepancy
6.76 When true leg length discrepancy is determined clinically (page 75, AMA4 Guides), the method used must be indicated (for example, tape measure from anterior superior iliac spine to medial malleolus). Clinical assessment of legislation length discrepancy is an acceptable method, but if computerised tomography films are available they should be used in preference, but only when there are no fixed deformities that would make them clinically inaccurate.
6.77 Table 35 (page 75, AMA4 Guides) must have the element of choice removed such that impairments for leg length should be read as the higher figure of the range quoted, being 0, 3, 5, 7 or 8 for WPI, or 0, 9, 14, 19 or 20 for lower limb impairment.
Gait derangement
6.78 Assessment of impairment based on gait derangement should be used as the method of last resort (pages 75-76, AMA4 Guides). Methods most specific to the nature of the disorder must always be used in preference. If gait derangement is used, it cannot be combined with any other impairment evaluation in the lower extremity. It can only be used if no other valid method is applicable, and reasons why it was chosen must be provided in the impairment evaluation report.
6.79 The use of any walking aid must be necessary and permanent.
6.80 Item b of Table 36 (page 76, AMA4 Guides) is deleted as the Trendelenburg sign is not sufficiently reliable.
Muscle atrophy (unilateral)
6.81 This section (page 76, AMA4 Guides) is not applicable if the limb other than that being assessed is abnormal (for example, if varicose veins cause swelling, or if there are other injuries).
6.82 Table 37 'Impairments from leg muscle atrophy' (page 77, AMA4 Guides) must not be used. Unilateral leg muscle atrophy must be assessed using Table 6.1(a) and (b) (below).
Table 6.1(a): Impairment due to unilateral leg muscle atrophy
Thigh: The circumference is measured 10 cm above the patella with the knee fully extended and the muscles relaxed.
Difference in circumference (cm) | Impairment degree | Whole person impairment (%) | Lower extremity impairment (%) |
|---|---|---|---|
0–0.9 | None | 0 | 0 |
1–1.9 | Mild | 2 | 6 |
2–2.9 | Moderate | 4 | 11 |
3+ | Severe | 5 | 12 |
Table 6.1(b): Impairment due to unilateral leg muscle atrophy
Calf: The maximum circumference on the normal side is compared with the circumference at the same level on the affected side.
Difference in circumference (cm) | Impairment degree | Whole person impairment (%) | Lower extremity impairment (%) |
|---|---|---|---|
0–0.9 | None | 0 | 0 |
1–1.9 | Mild | 2 | 6 |
2–2.9 | Moderate | 4 | 11 |
3+ | Severe | 5 | 12 |
Manual muscle strength testing
6.83 The Medical Research Council (MRC) grades for muscle strength are universally accepted. They are not linear in their application, but ordinal. The descriptions in Table 38 (page 77, AMA4 Guides) are to be used. The results of electrodiagnostic methods and tests are not to be considered in the evaluation of muscle testing, which is performed manually. Table 39 (page 77, AMA4 Guides) must be used for this method of evaluation.
Range of motion
6.84 Although range of motion (pages 77-78, AMA4 Guides) appears to be a suitable method for evaluating impairment, it can be subject to variation because of pain during motion at different times of examination and/or a possible lack of cooperation by the injured person being assessed. Range of motion is assessed as follows:
(a) a goniometer should be used where clinically indicated
(b) passive range of motion may form part of the clinical examination to ascertain clinical status of the joint, but impairment should only be calculated using active range of motion measurements
(c) if the medical assessor is not satisfied that the results of a measurement are reliable, active range of motion should be measured with at least three consistent repetitions
(d) if there is inconsistency in range of motion, then it should not be used as a valid parameter of impairment evaluation (see clause 6.40 of these Guidelines)
(e) if range of motion measurements at examination cannot be used as a valid parameter of impairment evaluation, the medical assessor should then use discretion in considering what weight to give other evidence available to determine if an impairment is present.
6.85 Tables 40 to 45 (page 78, AMA4 Guides) are used to assess range of motion in the lower extremities. Where there is loss of motion in more than one direction/axis of the same joint, only the most severe deficit is rated - the ratings for each motion deficit are not added or combined. However, motion deficits arising from separate tables can be combined.
Ankylosis
6.86 For the assessment of impairment when a joint is ankylosed (pages 79-82, AMA4 Guides), the calculation to be applied is to select the impairment if the joint is ankylosed in optimum position and then, if not ankylosed in the optimum position (Table 6.2), by adding (not combining) the values of WPI using Tables 46-61 (pages 79-82, AMA4 Guides). Note: The example listed under the heading 'Hip' on page 79 of the AMA4 Guides is incorrect.
Table 6.2: Impairment for ankylosis in the optimum position
Joint | Whole person (%) | Lower extremity (%) | Ankle or foot (%) |
Hip | 20 | 50 | – |
Knee | 27 | 67 | – |
Ankle | 4 | 10 | 14 |
Foot | 4 | 10 | 14 |
6.87 Note that the WPI from ankylosis of a joint, or joints, in the lower limb cannot exceed 40% WPI or 100% lower limb impairment. If this figure is exceeded when lower limb impairments are combined, then only 40% can be accepted as the maximum WPI.
Arthritis
6.88 Impairment due to arthritis (pages 82-83, AMA4 Guides) can be assessed by measuring the distance between the subchondral bone ends (joint space) if radiography is performed in defined positions. It indicates the thickness of articular cartilage. No notice is to be taken of other diagnostic features of arthritis such as osteophytes or cystic changes in the bone.
6.89 Hip radiography can be done in any position of the hip, but specified positions for the knee and ankle (page 82, AMA4 Guides) must be achieved by the radiographer.
6.90 Table 62 (page 83, AMA4 Guides) indicates the impairment assessment for arthritis based on articular cartilage thickness.
6.91 If arthritis is used as the basis for impairment assessment in this way, then the rating cannot be combined with gait derangement, muscle atrophy, muscle strength or range of movement assessments. It can be combined with a diagnosis-based estimate (Table 6.5).
6.92 When interpreting Table 62 (page 83, AMA4 Guides), if the articular cartilage interval is not a whole number, round to the higher impairment figure.
Amputation
6.93 Where there has been amputation of part of a lower extremity Table 63 applies (page 83, AMA4 Guides). The references to 3 inches below knee amputation should be converted to 7.5 centimetres.
Diagnosis-based estimates (lower extremity)
6.94 Section 3.2i (pages 84-88, AMA4 Guides) lists a number of conditions that fit a category of diagnosis-based estimates. They are listed in Table 64 (pages 85-86, AMA4 Guides). It is essential to read the footnotes.
6.95 It is possible to combine impairments from Table 64 for diagnosis-based estimates with other injuries (for example, nerve injury) using the 'Combined values' chart (pages 322-324, AMA4 Guides).
6.96 Pelvic fractures must be assessed using section 3.4 (page 131, AMA4 Guides). Fractures of the acetabulum should be assessed using Table 64 (pages 85 86, AMA4 Guides).
6.97 Residual signs must be present at examination and may include anatomically plausible tenderness, clinically obvious asymmetry, unilateral limitation of hip joint range of motion not associated with fractured acetabulum and/or clear evidence of malalignment.
6.98 Where both collateral and cruciate ligament laxity of mild severity is present, these must be assessed separately as 3% WPI for each ligament and then combined, resulting in a total of 6% WPI.
6.99 Rotational deformity following tibial shaft fracture must be assessed analogously to Table 64 'Tibial shaft fracture, malalignment of' (page 85, AMA4 Guides).
6.100 To avoid the risk of double assessment, if avascular necrosis of the talus is used as the basis for assessment, it cannot be combined with intra-articular fracture of the ankle with displacement or intra-articular fracture of the hind foot with displacement in Table 64, column 1 (page 86, AMA4 Guides).
6.101 Tables 65 and 66 (pages 87-88, AMA4 Guides) use a different method of assessment. A point score system is applied, and then the total of points calculated for the hip or knee joint respectively is converted to an impairment rating from Table 64. Tables 65 and 66 refer to the hip and knee joint replacement respectively. Note that, while all the points are added in Table 65, some points are deducted when Table 66 is used.
6.102 In Table 65, references to distance walked under 'b. Function', six blocks should be construed as being 600 metres, and three blocks as being 300 metres.
Skin loss (lower extremity)
6.103 Skin loss can only be included in the calculation of impairment if it is in certain sites and meets the criteria listed in Table 67 (page 88, AMA4 Guides). Scarring otherwise in the lower extremity must be assessed with reference to 'Other body systems' within this part of the Motor Accident Guidelines.
Impairment of the lower extremity due to peripheral nerve injury
6.104 Peripheral nerve injury should be assessed by reference to section 3.2k (pages 88-89, AMA4 Guides). Separate impairments for the motor, sensory and dysaesthetic components of nerve dysfunction in Table 68 (page 89, AMA4 Guides) are combined.
6.105 The posterior tibial nerve is not included in Table 68, but its contribution can be calculated by subtracting common peroneal nerves rating from sciatic nerve rating as shown in Table 6.3 (below). The values in brackets are lower extremity impairment values.
Table 6.3: Impairment for selected lower extremity peripheral nerves
Nerve | Motor % | Sensory % | Dysaesthesia % |
|---|---|---|---|
Sciatic nerve | 30 (75) | 7 (17) | 5 (12) |
Common peroneal nerve | 15 (42) | 2 (5) | 2 (5) |
Tibial nerve | 15 (33) | 5 (12) | 3 (7) |
6.106 Peripheral nerve injury impairments can be combined with other impairments, but not those for muscle strength, gait derangement, muscle atrophy and CRPS, as shown in Table 6.5. When using Table 68, refer to Tables 11a and 12a (pages 48-49, AMA4 Guides) and clauses 6.58, 6.59 and 6.60 of these Guidelines.
Impairment of the lower extremity due to CRPS
6.107 The section 'Causalgia and reflex sympathetic dystrophy' (page 89, AMA4 Guides) must not be used. These conditions have been better defined since the AMA4 Guides were published. The current terminology is CRPS type I (referring to what was termed reflex sympathetic dystrophy) and CRPS type II (referring to what was termed causalgia).
6.108 When complex CRPS occurs in the lower extremity it must be evaluated as for the upper extremity using clauses 6.61-6.64 within this part of the Motor Accident Guidelines.
Impairment of the lower extremity due to peripheral vascular disease
6.109 Lower extremity impairment due to peripheral vascular disease is evaluated using Table 69 (page 89, AMA4 Guides). Table 14 (page 198, AMA4 Guides) must not be used. In Table 69, there is a range of lower extremity impairments, not WPI, within each of the classes 1 to 5. Where there is a range of impairment percentages listed, the medical assessor must nominate an impairment percentage based on the complete clinical circumstances revealed during the examination and provide reasons.
6.110 Lower extremity impairment values must be converted to WPI using Table 6.4.
Table 6.4: WPI values calculated from lower extremity impairment – % of impairment
Lower extremity | Whole person | Lower extremity | Whole person | Lower extremity | Whole person | Lower extremity | Whole person |
|---|---|---|---|---|---|---|---|
1 = 2 = 3 = 4 = 5 = | 0 1 1 2 2 | 26 = 27 = 28 = 29 = 30 = | 10 11 11 12 12 | 51 = 52 = 53 = 54 = 55 = | 20 21 21 22 22 | 76 = 77 = 78 = 79 = 80 = | 30 31 31 32 32 |
6 = 7 = 8 = 9 = 10 = | 2 3 3 4 4 | 31 = 32 = 33 = 34 = 35 = | 12 13 13 14 14 | 56 = 57 = 58 = 59 = 60 = | 22 23 23 24 24 | 81 = 82 = 83 = 84 = 85 = | 32 33 33 34 34 |
11 = 12 = 13 = 14 = 15 = | 4 5 5 6 6 | 36 = 37 = 38 = 39 = 40 = | 14 15 15 16 16 | 61 = 62 = 63 = 64 = 65 = | 24 25 25 26 26 | 86 = 87 = 88 = 89 = 90 = | 34 35 35 36 36 |
16 = 17 = 18 = 19 = 20 = | 6 7 7 8 8 | 41 = 42 = 43 = 44 = 45 = | 16 17 17 18 18 | 66 = 67 = 68 = 69 = 70 = | 26 27 27 28 28 | 91 = 92 = 93 = 94 = 95 = | 36 37 37 38 38 |
21 = 22 = 23 = 24 = 25 = | 8 9 9 10 10 | 46 = 47 = 48 = 49 = 50 = | 18 19 19 20 20 | 71 = 72 = 73 = 74 = 75 = | 28 29 29 30 30 | 96 = 97 = 98 = 99 = 100 = | 38 39 39 40 40 |
Table 6.5: Permissible combinations of lower extremity assessment methods
Limb length discrepancy | Gait derangement | Muscle atrophy | Muscle strength | Range of motion or ankylosis | Arthritis | Amputations | Diagnosis-based estimates | Skin loss | Peripheral nerve injuries | CRPS | Vascular disorders | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Limb length discrepancy | – |
| x | x | x | x |
| x | x | x | x | x |
Gait derangement |
| – |
|
|
|
|
|
|
|
|
|
|
Muscle atrophy | x |
| – |
|
|
|
|
| x |
|
| x |
Muscle strength | x |
|
| – |
|
| x |
| x |
| ● | x |
Range of motion or ankylosis | x |
|
|
| – |
| x |
| x | x | ● | x |
Arthritis | x |
|
|
|
| – | x | x | x | x | x | x |
Amputations |
|
|
| x | x | x | – | x | x | x | x | x |
Diagnosis-based estimates | x |
|
|
|
| x | x | – | x | x | x | x |
Skin loss | x |
| x | x | x | x | x | x | – | x | x | x |
Peripheral nerve injuries | x |
|
|
| x | x | x | x | x | – |
| x |
Complex regional pain syndrome | x |
|
| ● | ● | x | x | x | x |
| – |
|
Vascular disorders | x |
| x | x | x | x | x | x | x | x |
| – |
Key: x You may combine these methods of assessment
● See specific instructions for CRPS in lower extremity
Source: American Medical Association, The Guides Newsletter, January/February, 1998, Lower Extremity section, pages 3/75–3/93, American Medical Association’s Guides to the Evaluation of Permanent Impairment, Fourth Edition. Organisation – Format © 1992, Randall D. Lea MD, FAADEP. Second Revision Feb 1998, Third Revision March 1999. Anthony J. Dorto, MD, FAADEP. Reprinted with permission of American Academy of Disability Evaluating Physicians, DISABILITY, May 1999, Vol. 8, No. 2
Table 6.6: Lower extremity worksheet
Line | Impairment | Table | AMA4 | Potential impairment | Selected impairment |
|---|---|---|---|---|---|
1 | Gait derangement | 36 | 76 | ||
2 | Unilateral muscle atrophy | 37 | 77 | ||
3 | True muscle weakness | 39 | 77 | ||
4 | Range of motion | 40–45 | 78 | ||
5 | Joint ankylosis | 46–61 | 79–82 | ||
6 | Arthritis | 62 | 83 | ||
7 | Amputation | 63 | 83 | ||
8 | Diagnosis-based estimates | 64 | 85–86 | ||
9 | Limb length discrepancy | 35 | 75 | ||
10 | Skin loss | 67 | 88 | ||
11 | Peripheral nerve deficit | 68 | 89 | ||
12 | Peripheral vascular disease | 69 | 89 | ||
13 | Complex regional pain syndrome | See clauses | AMA4 |
Note: For a combined impairment rating, refer to Table 6.5 for permissible combinations.
Spine
Introduction
6.111 The spine is discussed in section 3.3 of Chapter 3 in the AMA4 Guides (pages 94-138). Only the diagnosis-related estimate (DRE) method must be used for evaluating impairment of the spine, as modified by this Part of the Motor Accident Guidelines. The AMA4 Guides use the term injury model for this method.
6.112 The injury model relies especially on evidence of neurological deficits and uncommon, adverse structural changes, such as fractures and dislocations. Under this model, DREs are differentiated according to clinical findings that are verifiable using standard medical procedures.
6.113 The assessment of spinal impairment is made at the time the injured person is examined. If surgery has been performed, then the effect of the surgery, as well as the structural inclusions, must be taken into consideration when assessing impairment. Refer also to clause 6.20 in these Guidelines.
6.114 Medical assessors must consider whether any pre-existing spinal condition or surgery is related to the motor accident, is symptomatic and whether this would result in any or total apportionment. Where a pre-existing spinal condition, or spinal surgery, is unrelated to the injury from the relevant motor accident, the medical assessor should rely on clause 6.33.
6.115 The AMA4 Guides use the terms cervicothoracic, thoracolumbar and lumbosacral for the three spine regions. These terms relate to the cervical, thoracic and lumbar regions respectively.
Assessment of the spine
6.116 The range of motion (ROM) model and Table 75 are not to be used for spinal impairment evaluation (pages 112-130, AMA4 Guides).
6.117 The medical assessor may consider Table 6.7 (below) to establish the appropriate category for the spine impairment. Its principal difference from Table 70 (page 108, AMA4 Guides) is the removal of the term motion segment integrity wherever it appears (see clause 6.123).
Table 6.7: Assessing spinal impairment - DRE category
Injured person’s condition | I | II | III | IV | V |
|---|---|---|---|---|---|
Low back pain, neck pain, back pain or symptoms | I | ||||
Vertebral body compression < 25% | II | ||||
Low back pain or neck pain with guarding or | II | ||||
Posterior element fracture, healed, stable, no dislocation or radiculopathy | II | ||||
Transverse or spinous process fracture with displacement of fragment, healed, stable | II | ||||
Low back or neck pain with radiculopathy | III | ||||
Vertebral body compression fracture 25–50% | III | ||||
Posterior element fracture with spinal canal deformity or radiculopathy, stable, healed | III | ||||
Radiculopathy | III | ||||
Vertebral body compression > 50% | IV | V | |||
Multilevel structural compromise | IV | V | |||
Spondylolysis with radiculopathy | III | IV | V | ||
Spondylolisthesis without radiculopathy | I | II | |||
Spondylolisthesis with radiculopathy | III | IV | V | ||
Vertebral body fracture without radiculopathy | II | III | IV | ||
Vertebral body fracture with radiculopathy | III | IV | V | ||
Vertebral body dislocation without radiculopathy | II | III | IV | ||
Vertebral body dislocation with radiculopathy | III | IV | V | ||
Previous spine operation without radiculopathy | II | III | IV | ||
Previous spine operation with radiculopathy | III | IV | V | ||
Stenosis, facet arthrosis or disease | I | II | |||
Stenosis, facet arthrosis or disease with radiculopathy | III |
6.118 The evaluation must not include any allowance for predicted long-term change. For example, a spinal stenosis syndrome after vertebral fracture or increased back pain due to osteoarthritis of synovial joints after intervertebral disc injury must not be factored into the impairment evaluation.
6.119 All impairments in relation to the spine should be calculated in terms of WPI and assessed in accordance with clauses 6.1 to 6.46 within these Motor Accident Guidelines and Chapter 3.3 of AMA4 Guides.
6.120 The assessment should include a comprehensive accurate history, a review of all relevant records available at the assessment, a comprehensive description of the individual's current symptoms, a careful and thorough physical examination and all findings of relevant diagnostic tests available at the assessment. Imaging findings that are used to support the impairment rating should be concordant with symptoms and findings on examination. The medical assessor should record whether diagnostic tests and radiographs were seen or whether they relied on reports.
6.121 While imaging and other studies may assist medical assessors in making a diagnosis, it is important to note that the presence of a morphological variation from what is called normal in an imaging study does not make the diagnosis. Several reports indicate that approximately 30% of people who have never had back pain will have an imaging study that can be interpreted as positive for a herniated disc, and 50% or more will have bulging discs. Further, the prevalence of degenerative changes, bulges and herniations increases with advancing age. To be of diagnostic value, imaging findings must be concordant with clinical symptoms and signs, and the history of injury. In other words, an imaging test is useful to confirm a diagnosis, but an imaging result alone is insufficient to qualify for a DRE category.
6.122 The medical assessor must include in the report a description of how the impairment rating was calculated, with reference to the relevant tables and/or figures used.
Specific interpretation of the AMA4 Guides
Loss of motion segment integrity
6.123 The section 'Loss of motion segment integrity' (pages 98-99, AMA4 Guides) and all subsequent references to it must not be applied, as the injury model (DRE method) covers all relevant conditions.
Definitions of clinical findings used to place an individual in a DRE category
6.124 Definitions of clinical findings, which are used to place an individual in a DRE category, are provided in Table 6.8 (below). A definition of a muscle spasm has been included; however, it is not a clinical finding used to place an individual in a DRE category.
Table 6.8: Definitions of clinical findings
Term | Definition |
|---|---|
Atrophy | Atrophy is measured with a tape measure at identical levels on both limbs. For reasons of reproducibility, the difference in circumference should be 2 cm or greater in the thigh and 1 cm or greater in the arm, forearm or calf. The medical assessor can address asymmetry due to extremity dominance in the report. Measurements should be recorded to the nearest 0.5 cm. The atrophy should be clinically explicable in terms of the relevant nerve root affected. |
Muscle guarding | Guarding is a contraction of muscle to minimise motion or agitation of the injured or diseased tissue. It is not a true muscle spasm because the contraction can be relaxed. In the lumbar spine, the contraction frequently results in loss of the normal lumbar lordosis, and it may be associated with reproducible loss of spinal motion. |
Muscle spasm | Muscle spasm is a sudden, involuntary contraction of a muscle or a group of muscles. Paravertebral muscle spasm is common after acute spinal injury but is rare in chronic back pain. It is occasionally visible as a contracted paraspinal muscle but is more often diagnosed by palpation (a hard muscle). To differentiate true muscle spasm from voluntary muscle contraction, the individual should not be able to relax the contractions. The spasm should be present standing as well as in the supine position and frequently causes scoliosis. The medical assessor can sometimes differentiate spasm from voluntary contraction by asking the individual to place all their weight first on one foot and then the other while the medical assessor gently palpates the paraspinal muscles. With this manoeuvre, the individual normally relaxes the paraspinal muscles on the weight-bearing side. If the medical assessor witnesses this relaxation, it usually means that true muscle spasm is not present. |
Non-uniform loss of spinal motion (dysmetria) | Non-uniform loss of motion of the spine in one of the three principle planes is sometimes caused by muscle spasm or guarding. To qualify as true non-uniform loss of motion, the finding must be reproducible and consistent, and the medical assessor must be convinced that the individual is cooperative and giving full effort. When assessing non-uniform loss of range of motion (dysmetria), medical assessors must include all three planes of motion for the cervicothoracic spine (flexion/extension, lateral flexion and rotation), two planes of motion for the thoracolumbar spine (flexion/extension and rotation) and two planes of motion for the lumbosacral spine (flexion/ extension and lateral flexion). Medical assessors must record the range of spinal motion as a fraction or percentage of the normal range, such as cervical flexion is 3/4 or 75% of the normal range. Medical assessors must not refer to body landmarks (such as able to touch toes) to describe the available (or observed) motion. |
Non-verifiable radicular complaints | Non-verifiable radicular complaints are symptoms (for example, shooting pain, burning sensation, tingling) that follow the distribution of a specific nerve root, but there are no objective clinical findings (signs) of dysfunction of the nerve root (for example, loss or diminished sensation, loss or diminished power, loss or diminished reflexes). |
Reflexes | Reflexes may be normal, increased, reduced or absent. For reflex abnormalities to be considered valid, the involved and normal limbs should show marked asymmetry on repeated testing. Abnormal reflexes such as Babinski signs or clonus may be signs of corticospinal tract involvement. |
Sciatic nerve root tension signs | Sciatic nerve tension signs are important indicators of irritation of the lumbosacral nerve roots. While most commonly seen in individuals with a herniated lumbar disc, this is not always the case. In chronic nerve root compression due to spinal stenosis, tension signs are often absent. A variety of nerve tension signs have been described. The most commonly used is the straight leg raising (SLR) test. When performed in the supine position, the hip is flexed with the knee extended. In the sitting position, with the hip flexed 90 degrees, the knee is extended. The test is positive when thigh and/or leg pain along the appropriate dermatomal distribution is reproduced. The degree of elevation at which pain occurs is recorded. Research indicates that the maximum movement of nerve roots occurs when the leg is at an angle of 20 degrees to 70 degrees relative to the trunk. However, this may vary depending on the individual’s anatomy. Further, the L4, L5 and S1 nerve roots are those that primarily change their length when straight leg raising is performed. Thus, pathology at higher levels of the lumbar spine is often associated with a negative SLR test. Root tension signs are most reliable when the pain is elicited in a dermatomal distribution. Back pain on SLR is not a positive test. Hamstring tightness must also be differentiated from posterior thigh pain due to root tension. |
Weakness and loss of sensation | To be valid, the sensory findings must be in a strict anatomic distribution, i.e. follow dermatomal patterns. Motor findings should also be consistent with the affected nerve structure(s). Significant longstanding weakness is usually accompanied by atrophy. |
Diagnosis-related estimates model
6.125 To determine the correct diagnosis-related estimates (DRE) category, the medical assessor may start with Table 6.7 in these Guidelines, and use this table in conjunction with the DRE descriptors (pages 102-107, AMA4 Guides), as clarified by the definitions in Table 6.8 (above), with the following amendments to pages 102-107 of the AMA4 Guides:
(a) or history of guarding is deleted from DRE category I for the lumbosacral spine (page 102) and DRE category I for the cervicothoracic spine (page 103)
(b) no significant…roentgenograms is deleted from DRE category I for the lumbosacral spine (page 102) and DRE category I for the cervicothoracic spine (page 103) and DRE category I for the thoracolumbar (page 106)
(c) documented or as it relates to muscle guarding is deleted from DRE category I for the thoracolumbar spine (page 106)
(d) replace that has been observed and documented by a physician with that has been observed and documented by the medical assessor in DRE category II for the lumbosacral spine (page 102)
(e) replace observed by a physician with observed by the medical assessor in the descriptors for DRE category II for the cervicothoracic spine (page 104) and thoracolumbar spine (page 106)
(f) replace or displacement with with displacement in the descriptors for DRE category II for the thoracolumbar spine (page 106).
6.126 If unable to distinguish between two DRE categories, the higher of those two categories must apply. The inability to differentiate must be noted and explained in the medical assessor's report.
6.127 Table 71 (page 109, AMA4 Guides) is not to be used. The definitions of clinical findings in Table 6.8 should be the criteria by which a diagnosis and allocation of a DRE category are made.
Applying the DRE method
6.128 Section 3.3f 'Specific procedures and directions' (page 101, AMA4 Guides) indicates the steps that should be followed. Table 6.7 in these Guidelines is a simplified version of that section and must be interpreted in conjunction with the amendments listed in clause 6.125 (above).
6.129 DRE I applies when the injured person has symptoms but there are no objective clinical findings by the medical assessor. DRE II applies when there are clinical findings made by the medical assessor, as described in the sections 'Description and Verification' (pages 102-107, AMA4 Guides) with the amendments in clause 6.125, for each of the three regions of the spine. Note that symmetric loss of movement is not dysmetria and does not constitute an objective clinical finding.
6.130 When allocating the injured person to a DRE category, the medical assessor must reference the relevant differentiators and/or structural inclusions.
6.131 Separate injuries to different regions of the spine must be combined.
6.132 Multiple impairments within one spinal region must not be combined. The highest DRE category within each region must be chosen.
Loss of structural integrity
6.133 The AMA4 Guides (page 99) use the term structural inclusions to define certain spine fracture patterns that may lead to significant impairment and yet not demonstrate any of the findings involving differentiators. Some fracture patterns are clearly described in the examples of DRE categories in sections 3.3g, 3.3h and 3.3i. They are not the only types of injury in which there is a loss of structural integrity of the spine. In addition to potentially unstable vertebral body fractures, loss of structural integrity can occur by purely soft tissue flexion-distraction injuries.
Spondylolysis and spondylolisthesis
6.134 Spondylolysis and spondylolisthesis are conditions that are often asymptomatic and are present in 5-6% of the population. In assessing their relevance, the degree of slip (anteroposterior translation) is a measure of the grade of spondylolisthesis and not in itself evidence of loss of structural integrity. To assess an injured person as having symptomatic spondylolysis or spondylolisthesis requires a clinical assessment as to the nature and pattern of the injury, the injured person's symptoms and the medical assessor's findings on clinical examination. Table 6.8 can be used to allocate spondylolysis or spondylolisthesis to categories I-V depending on the descriptor's clinical findings in the appropriate DRE. The injured person's DRE must fit the description of clinical findings described in Table 6.8.
6.135 Medical assessors should be aware that acute traumatic spondylolisthesis is a rare event.
Sexual functioning
6.136 Sexual dysfunction should only be assessed as an impairment related to spinal injury where there is other objective evidence of spinal cord, cauda equina or bilateral nerve root dysfunction (Table 19, page 149, AMA4 Guides). There is no additional impairment rating for sexual dysfunction in the absence of objective neurological impairment.
6.137 Chapter 11 'The urinary and reproductive systems' of the AMA4 Guides should only be used to assess impairment for impotence where there has been a direct injury to the urinary tract. If this occurs, the impairment for impotence must be combined with any spine-related WPI. An example is provided in the AMA4 Guides (page 257) where there is a fracture and dissociation of the symphysis pubis and a traumatic disruption of the urethra.
Radiculopathy
6.138 Radiculopathy is the impairment caused by dysfunction of a spinal nerve root or nerve roots. To conclude that a radiculopathy is present, two or more of the following signs should be found:
(a) loss or asymmetry of reflexes (see the definitions of clinical findings in Table 6.8 in these Guidelines)
(b) positive sciatic nerve root tension signs (see the definitions of clinical findings in Table 6.8 in these Guidelines)
(c) muscle atrophy and/or decreased limb circumference (see the definitions of clinical findings in Table 6.8 in these Guidelines)
(d) muscle weakness that is anatomically localised to an appropriate spinal nerve root distribution
(e) reproducible sensory loss that is anatomically localised to an appropriate spinal nerve root distribution.
6.139 Spinal injury causing sensory loss at C2 or C3 must be assessed by first using Table 23 (page 152) of the AMA4 Guides, rather than classifying the injury as DRE cervicothoracic category III (radiculopathy). The value must then be combined with the DRE rating for the cervical vertebral injury.
6.140 Note that complaints of pain or sensory features that follow anatomical pathways but cannot be verified by neurological findings do not by themselves constitute radiculopathy. They are described as non-verifiable radicular complaints in the definitions of clinical findings (Table 6.8 in these Guidelines).
6.141 Global weakness of a limb related to pain or inhibition or other factors does not constitute weakness due to spinal nerve malfunction.
6.142 Electrodiagnostic tests are rarely necessary investigations and a decision about the presence of radiculopathy can generally be made on clinical grounds. The diagnosis of radiculopathy should not be made solely from electrodiagnostic tests.
Multilevel structural compromise
6.143 Multilevel structural compromise (Table 70, page 108, AMA4 Guides) refers to those DREs that are in categories IV and V. It is constituted by structural inclusion, which by definition (page 99, AMA4 Guides) is related to spine fracture patterns and is different from the differentiators and clinical findings in Table 6.8.
6.144 Multilevel structural compromise must be interpreted as fractures of more than one vertebra. To provide consistency of interpretation of the meaning of multiple vertebral fractures, the definition of a vertebral fracture includes any fracture of the vertebral body or of the posterior elements forming the ring of the spinal canal (the pedicle or lamina). It does not include fractures of transverse processes or spinous processes, even at multiple levels (see also clause 6.149 in these Guidelines).
6.145 Multilevel structural compromise also includes spinal fusion and intervertebral disc replacement.
6.146 Multilevel structural compromise or spinal fusion across regions is assessed as if it is in one region. The region giving the highest impairment value must be chosen. A fusion of L5 and S1 is considered to be an intervertebral fusion.
6.147 A vertebroplasty should be assessed on the basis of the fracture for which it was performed.
6.148 Compression fracture: The preferred method of assessing the amount of compression is to use a lateral X-ray of the spinal region with the beam parallel to the disc spaces. If this is not available, a CT scan can be used. Caution should be used in measuring small images as the error rate will be significant unless the medical assessor has the ability to magnify the images electronically. Medical assessors should not rely on the estimated percentage compression reported on the radiology report, but undertake their own measurements to establish an accurate percentage using the following method:
(a) the area of maximum compression is measured in the vertebra with the compression fracture
(b) the same area of the vertebrae directly above and below the affected vertebra is measured and an average obtained.
(c) the measurement from the compressed vertebra is then subtracted from the average of the two adjacent vertebrae
(d) the resulting figure is divided by the average of the two unaffected vertebrae and turned into a percentage
(e) if there are not two adjacent normal vertebrae, then the next vertebra that is normal and adjacent (above or below the affected vertebra) is used.
The calculations must be documented in the impairment evaluation report.
6.149 Fractures of transverse or spinous processes (one or more) with displacement within a spinal region are assessed as DRE category II because they do not disrupt the spinal canal (pages 102, 104, 106, AMA4 Guides) and they do not cause multilevel structural compromise.
6.150 One or more end-plate fractures in a single spinal region without measurable compression of the vertebral body are assessed as DRE category II.
6.151 In the application of Table 6.7 regarding multilevel structural compromise:
(a) multiple vertebral fractures without radiculopathy are classed as category IV
(b) multiple vertebral fractures with radiculopathy are classed as category V.
Spinal cord injury
6.152 The assessment of spinal cord injury is covered in clause 6.161 in these Guidelines.
6.153 Cauda equina syndrome: In the AMA4 Guides, this term does not have its usual medical meaning. For the purposes of the AMA4 Guides, an injured person with cauda equina syndrome has objectively demonstrated permanent partial loss of lower extremity function bilaterally. This syndrome may have associated objectively demonstrated bowel or bladder impairment.
Pelvic fractures
6.154 Pelvic fractures must be assessed using section 3.4 (page 131, AMA4 Guides). Fractures of the acetabulum must be assessed using Table 64 (pages 85-86, AMA4 Guides).
6.155 Multiple fractures of the pelvis must be assessed separately and then combined.
The terms cervicothoracic, thoracolumbar and lumbosacral have been defined in clause 6.115.
Nervous system
Introduction
6.156 Chapter 4 (pages 139-152, AMA4 Guides) provides guidance on methods of assessing permanent impairment involving the central nervous system. Elements of the assessment of permanent impairment involving the peripheral nervous system can be found in relevant parts of the 'Upper extremity', 'Lower extremity' and 'Spine' sections.
6.157 Chapter 4 is logically structured and consistent with the usual sequence of examining the nervous system. Cortical functions are discussed first, followed by the cranial nerves, the brain stem, the spinal cord and the peripheral nervous system.
6.158 Spinal cord injuries (SCI) must be assessed using the 'Nervous system' and 'Musculoskeletal system' chapters of the AMA4 Guides and these Guidelines. See clause 6.161.
6.159 The relevant parts of the 'Upper extremity', 'Lower extremity' and 'Spine' chapters of the AMA4 Guides must be used to evaluate impairments of the peripheral nervous system.
Assessment of the nervous system
6.160 The introduction to Chapter 4 'Nervous system' in the AMA4 Guides is ambiguous in its statement about combining nervous system impairments. The medical assessor must consider the categories of:
(a) aphasia or communication disorders
(b) mental status and integrative functioning abnormalities
(c) emotional and behavioural disturbances
(d) disturbances of consciousness and awareness (permanent and episodic).
The medical assessor must select the highest rating from categories 1 to 4. This rating can then be combined with ratings of other nervous system impairments or from other body regions.
6.161 A different approach is taken in assessing spinal cord impairment (section 4.3, pages 147-148, AMA4 Guides). In this case, impairments due to this pathology can be combined using the 'Combined values' chart (pages 322-324, AMA4 Guides). It should be noted that section 4.3 'Spinal cord' must be used for motor or sensory impairments caused by a central nervous system lesion. Impairment evaluation of spinal cord injuries should be combined with the associated DRE I-V from section 3.3 in the 'Musculoskeletal system' Chapter (pages 101-107, AMA4 Guides). This section covers hemiplegia due to cortical injury as well as SCI.
6.162 Headache or other pain potentially arising from the nervous system, including migraine, is assessed as part of the impairment related to a specific structure. The AMA4 Guides state that the impairment percentages shown in the chapters of the AMA4 Guides make allowance for the pain that may accompany the impairing condition.
6.163 The 'Nervous system' Chapter of the AMA4 Guides lists many impairments where the range for the associated WPI is from 0% to 9% or 0% to 14%. Where there is a range of impairment percentages listed, the medical assessor must nominate an impairment percentage based on the complete clinical circumstances revealed during the examination and provide reasons.
Specific interpretation of the AMA4 Guides
The central nervous system - cerebrum or forebrain
6.164 For an assessment of mental status impairment and emotional and behavioural impairment there should be:
(a) evidence of a significant impact to the head or a cerebral insult, or that the motor accident involved a high-velocity vehicle impact, and
(b) one or more significant, medically verified abnormalities such as an abnormal initial post-injury Glasgow Coma Scale score, or post traumatic amnesia, or brain imaging abnormality.
6.165 The results of psychometric testing, if available, must be taken into consideration.
6.166 Assessment of disturbances of mental status and integrative functioning: Table 6.9 in these Guidelines - the clinical dementia rating (CDR), which combines cognitive skills and function, must be used for assessing disturbances of mental status and integrative functioning.
6.167 When using the CDR, the injured person's cognitive function for each category should be scored independently. The maximum CDR score is 3. Memory is considered the primary category; the other categories are secondary.
(a) if at least three secondary categories are given the same numeric score as memory, then the CDR = M
(b) if three or more secondary categories are given a score greater or less than the memory score, CDR = the score of the majority of secondary categories, unless
- three secondary categories are scored less than M and two secondary categories are scored greater than M, then the CDR = M
(c) similarly, if two secondary categories are greater than M, two are less than M and one is the same as M, CDR = M.
6.168 In Table 6.9, 'Personal care' (PC) for the level of impairment is the same for a CDR score of 0 and a CDR score of 0.5, being fully capable of self-care. In order to differentiate between a personal care CDR score of 0 and 0.5, a rating that best fits with the pattern of the majority of other categories must be allocated. For example, when the personal care rating is fully capable of self-care and at least three other components of the CDR are scored at 0.5 or higher, the PC must be scored at 0.5. If three or more ratings are less than 0.5, then a rating of 0 must be assigned. Reasons to support all ratings allocated must be provided.
6.169 Corresponding impairment ratings for CDR scores are listed in Table 6.10 in these Guidelines.
6.170 Emotional and behavioural disturbances assessment: Table 3 (page 142, AMA4 Guides) must be used to assess emotional or behavioural disturbances.
6.171 Sleep and arousal disorders assessment: Table 6 (page 143, AMA4 Guides) must be used to assess sleep and arousal disorders. The assessment is based on the clinical assessment normally done for clinically significant disorders of this type.
6.172 Visual impairment assessment: An ophthalmologist must assess all impairments of visual acuity, visual fields or extra-ocular movements (page 144, AMA4 Guides).
6.173 Trigeminal nerve assessment: Sensory impairments of the trigeminal nerve must be assessed with reference to Table 9 (page 145, AMA4 Guides). The words or sensory disturbance are added to the table after the words neuralgic pain in each instance. Impairment percentages for the three divisions of the trigeminal nerve must be apportioned with extra weighting for the first division (for example, division 1 - 40%, and division 2 and 3 - 30% each). If present, motor loss for the trigeminal nerve must be assessed in terms of its impact on mastication and deglutition (page 231, AMA4 Guides).
6.174 As per clause 6.189, regarding bilateral total facial paralysis in Table 4 (page 230, AMA4 Guides) total means all branches of the facial nerve.
6.175 Sexual functioning assessment: Sexual dysfunction is assessed as an impairment only if there is an associated objective neurological impairment (page 149, AMA4 Guides). This is consistent with clauses 6.136 and 6.137 in these Guidelines.
6.176 Olfaction and taste assessment: The assessment of olfaction and taste is covered in clauses 6.192 and 6.193 in these Guidelines.
Table 6.9: Clinical dementia rating (CDR)
Impairment level and CDR score | |||||
|---|---|---|---|---|---|
None 0 | Questionable 0.5 | Mild 1.0 | Moderate 2.0 | Severe 3.0 | |
Memory (M) | No memory loss or slight inconsistent forgetfulness | Consistent slight forgetfulness; partial recollection of events; benign forgetfulness | Moderate memory loss; more marked for recent events; defect interferes with everyday activities | Severe memory loss; only highly learned material retained; new material rapidly lost | Severe memory loss; only fragments remain |
Orientation (O) | Fully oriented | Fully oriented except for slight difficulty with time relationships | Moderate difficultly with time relationships; oriented in place at examination; may have geographic disorientation elsewhere | Severe difficulty with time relationships; usually disoriented to time, often to place | Oriented to person only |
Judgement and problem solving (JPS) | Solves everyday problems and handles business and financial affairs well; judgement good in relation to past performance | Slight impairment in solving problems, similarities and differences | Moderate difficulty in handling problems, similarities and differences; social judgement usually maintained | Severely impaired in handling problems, similarities and differences; social judgement usually impaired | Unable to make judgements or solve problems |
Community affairs (CA) | Independent function at usual level in job, shopping, volunteer and social groups | Slight impairment in these activities | Unable to function independently in these activities although may still be engaged in some; appears normal to casual inspection | No pretence of independent function outside home; appears well enough to be taken to functions outside a family home | No pretence of independent function outside home; appears too ill to be taken to functions outside a family home |
Home and hobbies (HH) | Life at home, hobbies and intellectual interests well maintained | Life at home, hobbies and intellectual interests slightly impaired | Mild but definite impairment of function at home; more difficult chores abandoned; more complicated hobbies and interests abandoned | Only simple chores preserved; very restricted interests, poorly maintained | No significant function at home |
Personal care (PC) | Fully capable of self-care | Fully capable of self-care* *see clause 6.168 | Needs prompting | Requires assistance in dressing, hygiene, keeping of personal effects | Requires much help with personal care; frequent incontinence |
Table 6.10: Criteria for rating impairment related to mental status
Class 1 1-14% WPI | Class 2 15-29% WPI | Class 3 30-49% WPI | Class 4 50-70% WPI |
|---|---|---|---|
Impairment exists, but ability remains to perform satisfactorily most activities of daily living | Impairment requires direction of some activities of daily living | Impairment requires assistance and supervision for most activities of daily living | Unable to care for self and be safe in any situation without supervision |
CDR = 0.5 | CDR = 1.0 | CDR = 2.0 | CDR = 3.0 |
Ear, nose and throat, and related structures
Introduction
6.177 Chapter 9 of the AMA4 Guides (pages 223-234) provides guidance on methods of assessing permanent impairment involving the ear, nose and throat, and related structures, including the face.
6.178 Chapter 9 discusses the ear, hearing, equilibrium, the face, respiratory (air passage) obstruction, mastication and deglutition, olfaction and taste, and speech. There is potential overlap with other chapters, particularly the nervous system, in these areas.
Assessment of ear, nose and throat, and related structures
6.179 To assess impairment of the ear, nose and throat, and related structures, the injured person must be assessed by the medical assessor. While the assessment may be based principally on the results of audiological or other investigations, the complete clinical picture must be elaborated through direct consultation with the injured person by the medical assessor.
Specific interpretation of the AMA4 Guides
Ear and hearing
6.180 Ear and hearing (pages 223-224, AMA4 Guides): Tinnitus is only assessable in the presence of hearing loss, and both must be caused by the motor accident. An impairment of up to 5% can be added, not combined, to the percentage binaural hearing impairment before converting to WPI hearing loss if tinnitus is permanent and severe.
Hearing impairment
6.181 Hearing impairment (pages 224-228, AMA4 Guides): sections 9.1a and 9.1b of the AMA4 Guides are replaced with the following section.
6.182 Impairment of an injured person's hearing is determined according to evaluation of the individual's binaural hearing impairment.
6.183 Hearing impairment must be evaluated when the impairment is permanent. Prosthetic devices (i.e. hearing aids) must not be used during evaluation of hearing sensitivity.
6.184 Hearing threshold level for pure tones is defined as the number of decibels above a standard audiometric zero level for a given frequency at which the listener's threshold of hearing lies when tested in a suitable sound-attenuated environment. It is the reading on the hearing level dial of an audiometer calibrated according to current Australian standards.
6.185 Binaural hearing impairment is determined by using the 1988 National Acoustics Laboratory tables 'Improved procedure for determining percentage loss of hearing', with allowance for presbyacusis according to the presbyacusis correction table in the same publication (NAL Report No. 118, National Acoustics Laboratory, Commonwealth of Australia, 1988).
6.186 Table 3 (page 228, AMA4 Guides) is used to convert binaural hearing impairment to impairment of the whole person. For example, a person aged 50 with a total unilateral hearing loss in the right ear and no hearing loss in the left ear has 17% binaural hearing impairment less 0% presbyacusis correction, which is equivalent to 6% WPI.
Equilibrium
6.187 Assessment of impairment due to disorders of equilibrium (pages 228-229, AMA4 Guides) is dependent on objective findings of vestibular dysfunction. Such data must be available to the medical assessor.
6.188 There is an error in the description of classes 3, 4 and 5 in 'Criteria of vestibular impairment' (page 229, AMA4 Guides). Class 3 of impairment of vestibular function is associated with a WPI of 11% to 30%. Class 4 is 31% to 60% and class 5, 61% to 95%.
Face
6.189 Facial scarring and disfigurement are assessed separately to scarring elsewhere on the body. This scarring is combined with any other assessment of scarring and/or other permanent impairment assessments. In Table 4 (page 230, AMA4 Guides), total means all branches of the facial nerve.
6.190 Loss of the entire outer ear is 11% WPI.
6.191 The assessment of permanent impairment involving scarring of the face may be undertaken using Chapter 13 'The skin' (pages 279-280, AMA4 Guides) and/or section 9.2 'The face' (pages 229-230, AMA4 Guides).
Olfaction and taste
6.192 There is a discrepancy in the AMA4 Guides in the treatment of olfaction and taste between the 'Nervous system' Chapter (pages 144, 146) and the 'ENT' Chapter (pages 231-232). To resolve this difference, the medical assessor may assign a value of WPI from 1% to 5% for loss of sense of taste and a value of WPI from 1% to 5% for loss of sense of olfaction. Where there is a range of impairment percentages listed, the medical assessor must nominate an impairment percentage based on the complete clinical circumstances revealed during the examination and provide reasons.
6.193 However, the very rare case of total permanent loss of taste and olfaction is deemed in these Guidelines to constitute greater than 10% permanent impairment.
Teeth
6.194 An impairment assessment for loss of teeth must be done with the injured person wearing their dental prosthesis if this was normal for the injured person before the accident. If, as a result of the motor accident, the injured person required a removable dental prosthesis for the first time, or a different dental prosthesis, the difference should be accounted for in the assessment of permanent impairment.
6.195 Damage to the teeth can only be assessed when there is a permanent impact on mastication and deglutition (page 231, AMA4 Guides) and/or loss of structural integrity of the face (pages 229-230, AMA4 Guides).
6.196 Where loss of structural integrity occurs as a result of a dental injury, the injury must be assessed for a loss of functional capacity (mastication) and a loss of structural integrity (cosmetic deformity) and any impairment combined.
6.197 When using Table 6 'Relationship of dietary restrictions to permanent impairment' (page 231, AMA4 Guides) the first category must be 0-19%, not 5-19%.
6.198 In some cases, it will be necessary to access current dental X-rays to assess permanent impairment.
Respiration
6.199 When Table 5 (page 231, AMA4 Guides) is used for the evaluation of air passage defects, these Guidelines allow 0-5% WPI where there is significant difficulty in breathing through the nose and examination reveals significant partial obstruction of the right and/or left nasal cavity or nasopharynx, or significant septal perforation.
Speech
6.200 When Table 7 'Speech impairment criteria' (page 233, AMA4 Guides) is used, the percentage from the table must be converted to WPI using Table 9 (page 234, AMA4 Guides).
Mental and behavioural disorders
Introduction
6.201 Psychiatric disorders have complex effects on the individual, and impairment must be assessed by a psychiatrist.
6.202 The AMA4 Guides do not give percentages of psychiatric impairment in Chapter 14 (pages 291-302), which deals with mental and behavioural disorders. Medically determinable impairments in thinking, affect, intelligence, perception, judgement and behaviour are difficult to translate into functional limitations.
6.203 The assessment of mental and behavioural disorders must be undertaken in accordance with the psychiatric impairment rating scale (PIRS) as set out in these Guidelines. Chapter 14 of the AMA4 Guides (pages 291-302) is to be used for background or reference only.
6.204 The PIRS draws heavily on Chapter 14 of the AMA4 Guides.
6.205 The AMA4 Guides provide a framework to determine whether a motor accident has caused psychiatric impairment. They bridge the gap between impairment and disability by focusing on four areas or aspects of functioning:
(a) activities of daily living (ADL). Three aspects of ADL are used in the PIRS system
(b) social functioning
(c) concentration, persistence and pace
(d) adaptation.
6.206 These areas are described in detail on pages 294-295 of the AMA4 Guides.
6.207 Activities of daily living include self-care, personal hygiene, communication, ambulation, travel and social and recreational activities.
6.208 Social functioning refers to the capacity to get along with others and communicate effectively.
6.209 Concentration, persistence and pace is defined as the ability to sustain focused attention, for long enough to permit the timely completion of tasks commonly found in work settings.
6.210 Adaptation (also called deterioration or de-compensation in work or work-like settings) refers to the repeated failure to adapt to stressful circumstances.
6.211 Impairment is divided into five classes ranging from no impairment to extreme impairment.
6.212 Mental and behavioural disorders resulting from an organic brain injury are most suitably assessed as an organic problem under clause 6.156 to 6.176 in these Guidelines.
Assessment of mental and behavioural disorders
6.213 The impairment must be attributable to a psychiatric diagnosis recognised by the current edition of the Diagnostic & Statistical Manual of Mental Disorders (DSM) or the current edition of the International Statistical Classification of Diseases & Related Health Problems (ICD). The impairment evaluation report must specify the diagnostic criteria on which the diagnosis is based.
6.214 Impairment due to physical injury is assessed using different criteria outlined in other parts of these Guidelines.
6.215 The PIRS must not be used to measure impairment due to somatoform disorders or pain.
6.216 Where cognitive deficits are suspected, the medical assessor must carefully consider the history of the injury, medical treatment and progress through rehabilitation. The medical assessor must also take into account the results of CT and MRI scans, electroencephalograms (EEGs) and psychometric tests.
6.217 The scale must be used by a properly trained medical assessor. The psychiatrist's clinical judgement is the most important tool in the application of the scale. The impairment rating must be consistent with a recognised psychiatric diagnosis and based on the psychiatrist's clinical experience.
6.218 In order to measure impairment caused by a specific event, the medical assessor must, in the case of an injured person with a pre-existing psychiatric diagnosis or diagnosable condition, estimate the overall pre-existing impairment using precisely the method set out in this part of the Guidelines, and subtract this value from the current impairment rating.
The psychiatric impairment rating scale
6.219 Behavioural consequences of psychiatric disorders are assessed on six areas of function, each of which evaluates an area of functional impairment:
(a) self-care and personal hygiene (Table 6.11)
(b) social and recreational activities (Table 6.12)
(c) travel (Table 6.13)
(d) social functioning (relationships) (Table 6.14)
(e) concentration, persistence and pace (Table 6.15)
(f) adaptation (Table 6.16).
6.220 Impairment in each area of function is rated using class descriptors. Classes range from 1 to 5 according to severity. The standard form (Figure 6.2) must be used when scoring the PIRS. The classes in each area of function are described through the use of common examples. These are intended to be illustrative rather than literal criteria. The medical assessor should obtain a history of the injured person's pre-accident lifestyle, activities and habits, and then assess the extent to which these have changed as a result of the psychiatric injury. The medical assessor should take into account variations in lifestyle due to age, gender, cultural, economic, educational and other factors.
6.221 Where adaptation cannot be assessed by reference to work or a work-like setting, consideration must be given to the injured person's usual pre-injury roles and functions such as caring for others, housekeeping, managing personal/family finances, voluntary work, education/study or the discharge of other obligations and responsibilities.
Adjustment for the effects of treatment
6.222 An adjustment for the effects of prescribed treatment may be made by the medical assessor if all of the following requirements are met:
(a) there is research evidence demonstrating that the treatment prescribed is effective for the injured person's diagnosed psychiatric condition
(b) the medical assessor is satisfied that the treatment has been appropriate, for example, medication has been taken in the appropriate dose and duration
(c) there is clear clinical evidence that the treatment has been effective, that is, the injured person's symptoms have improved and/or functioning has improved
(d) it is the clinical judgement of the medical assessor that ceasing treatment will result in a deterioration of symptoms and/or a worsening in function.
6.223 The medical assessor may increase the percentage of WPI by:
(a) 0% WPI (no or negligible treatment effect)
(b) 1% WPI (a mild treatment effect)
(c) 2% WPI (a moderate treatment effect)
(d) 3% WPI (a full remission).
6.224 This clause does not apply to the use of analgesics, anti-inflammatory or antidepressant drugs for analgesia or pain management.
Table 6.11: Psychiatric impairment rating scale (PIRS)
Self-care and personal hygiene | |
|---|---|
Class 1 | No deficit, or minor deficit attributable to normal variation in the general population. |
Class 2 | Mild impairment. Able to live independently and look after self adequately, although may look unkempt occasionally. Sometimes misses a meal or relies on takeaway food. |
Class 3 | Moderate impairment. Cannot live independently without regular support. Needs prompting to shower daily and wear clean clothes. Cannot prepare own meals, frequently misses meals. Family member or community nurse visits (or should visit) 2–3 times per week to ensure minimum level of hygiene and nutrition. |
Class 4 | Severe impairment. Needs supervised residential care. If unsupervised, may accidentally or purposefully hurt self. |
Class 5 | Totally impaired. Needs assistance with basic functions, such as feeding and toileting. |
Table 6.12: Psychiatric impairment rating scale (PIRS)
Social and recreational activities | |
|---|---|
Class 1 | No deficit or minor deficit attributable to normal variation in the general population. Able to go out regularly to cinemas, restaurants or other recreational venues. Belongs to clubs or associations and is actively involved with these. |
Class 2 | Mild impairment. Able to occasionally go out to social events without needing a support person, but does not become actively involved; for example, in dancing, cheering favourite team. |
Class 3 | Moderate impairment. Rarely goes to social events, and mostly when prompted by family or close friend. Unable to go out without a support person. Not actively involved, remains quiet and withdrawn. |
Class 4 | Severe impairment. Never leaves place of residence. Tolerates the company of family member or close friend, but will go to a different room or the garden when others visit family or flatmate. |
Class 5 | Totally impaired. Cannot tolerate living with anybody, extremely uncomfortable when visited by close family member. |
Table 6.13: Psychiatric impairment rating scale (PIRS)
Travel | |
|---|---|
Class 1 | No deficit, or minor deficit attributable to normal variation in the general population. Able to travel to new environments without supervision. |
Class 2 | Mild impairment. Able to travel without support person, but only in a familiar area such as local shops or visiting a neighbour. |
Class 3 | Moderate impairment. Unable to travel away from own residence without support person. Problems may be due to excessive anxiety or cognitive impairment. |
Class 4 | Severe impairment. Finds it extremely uncomfortable to leave own residence even with a trusted person. |
Class 5 | Totally impaired. Cannot be left unsupervised, even at home. May require two or more persons to supervise when travelling. |
Table 6.14: Psychiatric impairment rating scale (PIRS)
Social functioning | |
|---|---|
Class 1 | No deficit, or minor deficit attributable to normal variation in the general population. No difficulty in forming and sustaining relationships; for example, a partner or close friendships lasting years. |
Class 2 | Mild impairment. Existing relationships strained. Tension and arguments with partner or close family member, loss of some friendships. |
Class 3 | Moderate impairment. Previously established relationships severely strained; evidenced, for example, by periods of separation or domestic violence. Partner, relatives or community services looking after children. |
Class 4 | Severe impairment. Unable to form or sustain long-term relationships. Pre-existing relationships ended; for example, lost partner, close friends. Unable to care for dependants; for example, own children, elderly parent. |
Class 5 | Totally impaired. Unable to function within society. Living away from populated areas, actively avoids social contact. |
Table 6.15: Psychiatric impairment rating scale (PIRS)
Concentration, persistence and pace | |
|---|---|
Class 1 | No deficit, or minor deficit attributable to normal variation in the general population. Able to operate at previous educational level; for example, pass a TAFE or university course within normal timeframe. |
Class 2 | Mild impairment. Can undertake a basic retraining course, or a standard course at a slower pace. Can focus on intellectually demanding tasks for up to 30 minutes, for example, then feels fatigued or develops headache. |
Class 3 | Moderate impairment. Unable to read more than newspaper articles. Finds it difficult to follow complex instructions; for example, operating manuals, building plans, make significant repairs to motor vehicle, type detailed documents, follow a pattern for making clothes, tapestry or knitting. |
Class 4 | Severe impairment. Can only read a few lines before losing concentration. Difficulties following simple instructions. Concentration deficits obvious even during brief conversation. Unable to live alone, or needs regular assistance from relatives or community services. |
Class 5 | Totally impaired. Needs constant supervision and assistance within an institutional setting. |
Table 6.16: Psychiatric impairment rating scale (PIRS)
Adaptation | |
|---|---|
Class 1 | No deficit, or minor deficit attributable to normal variation in the general population. Able to work full time. Duties and performance are consistent with injured person’s education and training. The injured person is able to cope with the normal demands of the job. |
Class 2 | Mild impairment. Able to work full time in a different environment. The duties require comparable skill and intellect. Can work in the same position, but no more than 20 hours per week; for example, no longer happy to work with specific persons, work in a specific location due to travel required. |
Class 3 | Moderate impairment. Cannot work at all in same position as previously. Can perform less than 20 hours per week in a different position, which requires less skill or is qualitatively different; for example, less stressful. |
Class 4 | Severe impairment. Cannot work more than one or two days at a time, less than 20 hours per fortnight. Pace is reduced, attendance is erratic. |
Class 5 | Totally impaired. Cannot work at all. |
Calculation of psychiatric impairment
6.225 Rating psychiatric impairment using the PIRS is a three-step procedure:
(a) determine the median class score
(b) calculate the aggregate score
(c) convert the median class and aggregate score to % WPI.
6.226 Determining the median class score: Each area of function described in the PIRS is given an impairment rating ranging from class 1 to class 5. The six class scores are arranged in ascending order using the standard form (Figure 6.2). The median class is then calculated by averaging the two middle scores. For example:
Example | Impairment rating | Median class |
|---|---|---|
A | 1, 2, 3, 3, 4, 5 | = 3 |
B | 1, 2, 2, 3, 3, 4 | = 2.5 = 3 |
C | 1, 2, 3, 5, 5, 5 | = 4 |
If a score falls between two classes, it is rounded up to the next class. A median class score of 2.5 thus becomes 3. The median class score method was chosen as it is not influenced by extremes. Each area of function is assessed separately. While impairment in one area is neither equivalent to nor interchangeable with impairment in other areas, the median seems the fairest way to translate different impairments onto a linear scale.
6.227 Calculation of the aggregate score: The aggregate score is used to determine an exact percentage of impairment within a particular class range. The six class scores are added to give the aggregate score.
6.228 Converting the median class and aggregate score: The median class and aggregate score are converted to a percentage impairment score using Table 6.17 'Conversion table'.
Table 6.17: Conversion table
Aggregate score | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | |
Class 1 | 0 | 0 | 1 | 1 | 2 | 2 | 2 | 3 | 3 | ||||||||||||||||
Class 2 | 4 | 5 | 5 | 6 | 7 | 7 | 8 | 9 | 9 | 10 | |||||||||||||||
Class 3 | 11 | 13 | 15 | 17 | 19 | 22 | 24 | 26 | 28 | 30 | |||||||||||||||
Class 4 | 31 | 34 | 37 | 41 | 44 | 47 | 50 | 54 | 57 | 60 | |||||||||||||||
Class 5 | 61 | 65 | 70 | 74 | 78 | 83 | 87 | 91 | 96 | 100 | |||||||||||||||
Conversion table - Explanatory notes
1. Distribution of aggregate scores:
- The lowest aggregate score that can be produced is 1 + 1 + 1 + 1 + 1 + 1 = 6.
- The highest score that can be produced is 5 + 5 + 5 + 5 + 5 + 5 = 30.
- Table 6.17 therefore has aggregate scores ranging from 6 to 30.
- Each median class score has a range of possible aggregate scores and hence a range of possible impairment scores (for example, class 3 = 11% - 30% WPI).
- Table 6.17 distributes the impairment percentages across the possible range of aggregate scores.
2. Same aggregate score in different classes:
- Table 6.17 shows that the same aggregate score leads to different impairment percentages for different median classes. For example, an aggregate score of 18 is equivalent to an impairment rating of:
- 10% in class 2
- 22% in class 3
- 34% in class 4.
- This is because the injured person whose impairment is in median class 2 is likely to have a lower score across most areas of function. The injured person may be significantly impaired in one aspect of their life, such as travel, yet have low impairment in social function, self-care or concentration. In contrast, someone whose impairment reaches median class 4 will experience significant impairment across most aspects of their life.
Examples
Example A
List classes in ascending order | Median class value | |||||||
|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 3 | 4 | 5 | 3 | ||
Aggregate score | Total | % | ||||||
1 + | 2 + | 3 + | 3 + | 4 + | 5 | = | 18 | 22% WPI |
Example B
List classes in ascending order | Median class value | |||||||
|---|---|---|---|---|---|---|---|---|
1 | 2 | 2 | 3 | 3 | 5 | 3 | ||
Aggregate score | Total | % | ||||||
1 + | 2 + | 2 + | 3 + | 3 + | 5 | = | 16 | 17% WPI |
Example C
List classes in ascending order | Median class value | |||||||
|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 5 | 5 | 5 | 4 | ||
Aggregate score | Total | % | ||||||
1 + | 2 + | 3 + | 5 + | 5 + | 5 | = | 21 | 44% WPI |
Figure 6.2: Psychiatric impairment rating scale – Assessment form
Psychiatric diagnoses | 1. | 2. | |||||||||
3. | 4. | ||||||||||
Psychiatric treatment | |||||||||||
Category | Class | Reason for decision | |||||||||
Self-care and personal hygiene | |||||||||||
Social and recreational activities | |||||||||||
Travel | |||||||||||
Social functioning | |||||||||||
Concentration, persistence and pace | |||||||||||
Adaptation | |||||||||||
List classes in ascending order | Median class value | ||||||||||
Aggregate score | Total | % | |||||||||
+ | + | + | + | + | = | ||||||
Pre-existing/subsequent impairment? If applicable, determine % as above | |||||||||||
List classes in ascending order | Median class value | ||||||||||
Aggregate score | Total | % | |||||||||
+ | + | + | + | + | = | ||||||
Final % WPI ___________ | |||||||||||
Other body systems
Respiratory system
6.229 The system of respiratory impairment classification is based on a combination of forced vital capacity (FVC), forced expiratory volume (FEV1) and diffusing capacity of carbon monoxide (DCO) or measurement of exercise capacity (VO2 max). Chapter 5 (pages 153-167, AMA4 Guides) should be infrequently used in assessing impairment following a motor accident. Healed sternal and rib fractures do not result in any assessable impairment unless they result in a permanent impairment of respiratory function.
6.230 Table 8 (page 162, AMA4 Guides) provides the classification of respiratory impairment. A footnote to the table reinforces that conditions other than respiratory disease may reduce maximum exercise capacity and medical assessors must carefully interpret the clinical presentation of the injured person.
6.231 The medical assessor must provide a specific percentage impairment for permanent impairment due to respiratory conditions. Table 8 (page 162, AMA4 Guides) must be used to classify the injured person's impairment. Classes 2, 3 and 4 define a range of WPI percentages. The medical assessor must provide a specific percentage impairment within the range for the class that best describes the clinical status of the injured person. Class 2 (10-25% WPI) will need careful consideration.
6.232 Use of Tables 2 to 7 (pages 156-161, AMA4 Guides) may give rise to an inaccurate interpretation of lung function and impairment due to age or race. Where appropriate, Tables 2 to 7 should be replaced with relevant guidelines from a substantial body of peer-reviewed research literature, which must be referenced.
Cardiovascular system
Introduction and assessment of the cardiovascular system
6.233 Chapter 6 (pages 169-199, AMA4 Guides) provides a clear explanation of the methods required for the assessment of the cardiovascular system.
6.234 The results from all relevant diagnostic tests must be taken into account by the medical assessor, including:
(a) ECG (including an exercise ECG)
(b) standard and trans-oesophageal echocardiogram
(c) exercise thallium scan, exercise echo scan
(d) coronary angiograms
(e) operative notes for coronary artery bypass grafts, coronary angioplasty or other surgery
(f) Holter monitoring results
(g) electrodiagnostic studies
(h) serum urea/electrolytes and urinalysis (particularly if hypertensive).
6.235 Diagnostic tests should not be ordered by the medical assessor for the purpose of rating impairment. This is in keeping with the approach taken elsewhere in Part 6 of the Guidelines.
6.236 Functional classification of cardiovascular system impairments: Table 2 (page 171, AMA4 Guides) should be used as an option if the medical assessor is not sure into which category the injured person should be placed based on specific pathology (refer to Tables 4-12, pages 172-195, AMA4 Guides). Table 2 can be used as a referee or umpire if there is doubt about the level of impairment that is obtained using the other recommended tables in this section.
6.237 Hypertensive cardiovascular disease (section 6.4, pages 185-188, AMA4 Guides): This type of cardiovascular disease (Table 9, page 187, AMA4 Guides) requires medical documentation of the hypertension. If the injured person's illness is controlled with medication, then they might not be assessable under this table. The medical assessor should refer to clauses 6.25-6.29 of these Guidelines.
6.238 Vascular diseases affecting the extremities (pages 196-198, AMA4 Guides): Impairments due to upper or lower extremity peripheral vascular disease resulting from vascular trauma must be assessed using the 'Musculoskeletal' Chapter of the AMA4 Guides. Tables 13 and 14 (pages 197-198, AMA4 Guides) must not be used.
6.239 Impairment scores from Table 17 'Impairment of the upper extremity due to peripheral vascular disease' (page 57, AMA4 Guides) and Table 69 'Impairment of the lower extremity due to peripheral vascular disease' (page 89, AMA4 Guides) must be converted to WPI.
Haematopoietic system
Introduction and assessment of the haematopoietic system
6.240 Chapter 7 (pages 201-207, AMA4 Guides) will be infrequently used in the motor accident context. The methods of impairment assessment suggested in this Part of the Motor Accident Guidelines should be used.
6.241 Splenectomy is covered in this chapter (page 205, AMA4 Guides). An injured person with post-traumatic splenectomy must be assessed as having 3% WPI.
Visual system
Introduction and assessment of the visual system
6.242 The visual system must be assessed by an ophthalmologist. Chapter 8 of the AMA4 Guides (pages 210-222) must be used.
6.243 Impairment of vision should be measured with the injured person wearing their corrective spectacles or contact lenses, if it was normal for the injured person to wear them before the motor accident, or if the need for such spectacles has become necessary due to normal physiological changes to the refractive error either in distance or near vision. If as a result of the injury, the injured person has been prescribed corrective spectacles and/or contact lenses for the first time, or different spectacles and/or contact lenses than those prescribed pre-injury, the difference should be accounted for in the assessment of permanent impairment.
Digestive system
Introduction and assessment of the digestive system
6.244 Assessments must be performed using the methods outlined in Chapter 10 (pages 235-248, AMA4 Guides).
6.245 Tables 2 to 7 in Chapter 10 (pages 239-247, AMA4 Guides) give details of the components to be assessed. Examples are given that assist by describing illustrative cases. Note that splenectomy is discussed in the 'Haematopoietic system' chapter.
6.246 In Table 2, 'Classes of impairment of the upper digestive tract' (page 239, AMA4 Guides), the reference to Loss of weight below desirable weight does not exceed 10% in class 2 must be replaced with Loss of weight below desirable weight (if any) does not exceed 10%.
6.247 Upper digestive tract disease caused by the commencement and ongoing use of anti-inflammatory medications must be assessed as 0-2% WPI class 1 impairment according to Table 2 (page 239, AMA4 Guides). Upper digestive tract disease caused by the use of anti-inflammatory medications resulting in severe and specific signs or symptoms must be assessed as a class 2 impairment according to Table 2 (page 239, AMA4 Guides).
6.248 Colonic and/or rectal disease caused by the use of opiate medication must be assessed as 0-2% WPI class 1 impairment according to Table 2 (page 239, AMA4 Guides). Assessment of constipation alone results in 0% WPI.
6.249 Table 7 (page 247, AMA4 Guides): In classes 1 and 2 the first criterion must be present, together with the second or third criterion. In class 3, all three criteria must be present.
Urinary and reproductive systems
Introduction and assessment of the urinary and reproductive systems
6.250 Chapter 11 (pages 249-262, AMA4 Guides) is used for the assessment of urinary and reproductive systems and provides clear methods for assessing impairment in these systems.
6.251 For male and female sexual dysfunction, objective pathology should be present for an impairment percentage to be given.
6.252 Objective evidence of neurological impairment is necessary to assess incontinence related to spinal injury (AMA4 Guides, Chapter 4, 4.3d). Objective evidence of injury to the bladder and urethra associated with urinary incontinence is necessary to assess urinary incontinence due to trauma (AMA4 Guides, Chapter 11, 11.3 and 11.4)
Endocrine system
Introduction and assessment of the endocrine system
6.253 Chapter 12 (pages 263-275, AMA4 Guides) is used to assess the endocrine system. Each endocrine organ or system is listed separately.
6.254 Where an impairment class defines a range of WPI percentages, the medical assessor must define a specific percentage impairment within the range described by the class that best describes the clinical status of the injured person and provide reasons.
6.255 Where injury has resulted in fat necrosis in the mammary glands, this must be assessed using Chapter 13 'The skin' (pages 278-289, AMA4 Guides).
6.256 Section 12.8 'Mammary glands' (page 275, AMA4 Guides) is replaced by these Guidelines. Total loss of one or both mammary glands is deemed to be an impairment of greater than 10% WPI.
6.257 Injury to the breast(s) caused by damage to a breast implant(s) must be assessed as class 1, Table 2 (page 280, AMA4 Guides).
Skin
Introduction and assessment of the skin
6.258 Chapter 13 (pages 277-289, AMA4 Guides) refers to skin diseases generally. In the context of injury, sections 13.4 'Disfigurement' (page 279, AMA4 Guides) and 13.5 'Scars and skin grafts' are particularly relevant.
6.259 The assessment of permanent impairment involving scarring of the face may be undertaken using Chapter 13 'The skin' (pages 279-280, AMA4 Guides) and/or section 9.2 'The face' (pages 229-230, AMA4 Guides). Criteria for facial impairment are listed on page 229 of the AMA4 Guides. Specific facial disfigurements may also be assessed by reference to Table 4 (page 230, AMA4 Guides).
6.260 Disfigurement, scars and skin grafts may be assessed as causing significant permanent impairment when the skin condition causes limitation in performance of activities of daily living. Assessment should include a history that sets out any alterations in activities of daily living. The AMA4 Guides (page 317) contain a table of activities of daily living. Any impairment secondary to severe scarring, such as contracture or nerve damage, is assessed using other chapters and combined with the assessment for scarring.
6.261 A scar may be present and rated 0% WPI.
6.262 Table 2 (page 280, AMA4 Guides) provides the method of classifying impairment due to skin disorders. Three components - namely signs and symptoms of skin disorder, limitation of activities of daily living and requirements for treatment - define five classes of impairment. Determining which class is applicable is primarily dependent on the impact of the skin disorder on daily activities. The medical assessor must derive a specific percentage impairment within the range described by the class that best describes the clinical status of the injured person. All three criteria must be present. Impairment values are WPI.
6.263 When using Table 2 (page 280, AMA4 Guides), the medical assessor is reminded to consider the skin as an organ. The effect of scarring (whether single or multiple) must be considered as the total effect of the scar on the organ system as it relates to the criteria in Table 2 'Table for the evaluation of minor skin impairment' (TEMSKI). Multiple scars must not be assessed individually. The medical assessor must not add or combine the assessment of individual scars but assess the total effect of the scarring on the entire organ system.
6.264 The TEMSKI (Table 6.18) is an extension of Table 2 (page 280, AMA4 Guides). The TEMSKI divides class 1 into five categories of impairment. When a medical assessor determines that a skin disorder falls into class 1, they must assess the skin disorder in accordance with the TEMSKI criteria. The medical assessor must evaluate all scars either individually or collectively with reference to the five criteria and 10 descriptors of the TEMSKI. The medical assessor should address all descriptors.
6.265 The TEMSKI must be used in accordance with the principle of best fit. The medical assessor must be satisfied that the criteria within the chosen category of impairment best reflect the skin disorder being assessed. The skin disorder should meet most, but does not need to meet all, of the criteria within the impairment category in order to satisfy the principle of best fit. The medical assessor must provide reasons as to why this category has been selected.
6.266 Where there is a range of values in the TEMSKI categories, the medical assessor should use clinical judgement to determine the exact impairment value and provide reasons that clearly link their clinical judgement to the impairment value selected.
6.267 For the purpose of assessing fat necrosis, Chapter 13 'The skin' (pages 277- 289, AMA4 Guides) may be used by analogy where appropriate.
Table 6.18: Table for the evaluation of minor skin impairment (TEMSKI)
Criteria | 0% WPI | 1% WPI | 2% WPI | 3–4% WPI | 5–9% WPI |
|---|---|---|---|---|---|
Description of the scar(s) and/or skin condition(s) (shape, texture, colour) | Injured person is not conscious or is barely conscious of the scar(s) or skin condition | Injured person is conscious of the scar(s) or skin condition | Injured person is conscious of the scar(s) or skin condition | Injured person is conscious of the scar(s) or skin condition | Injured person is conscious of the scar(s) or skin condition |
Good colour match with surrounding skin and the scar(s) or skin condition is barely distinguishable | Some parts of the scar(s) or skin condition colour contrast with the surrounding skin as a result of pigmentary or other changes | Noticeable colour contrast of scar(s) or skin condition with surrounding skin as a result of pigmentary or other changes | Easily identifiable colour contrast of scar(s) or skin condition with surrounding skin as a result of pigmentary or other changes | Distinct colour contrast of scar(s) or skin condition with surrounding skin as a result of pigmentary or other changes | |
Injured person is unable to easily locate the scar(s) or skin condition | Injured person is able to locate the scar(s) or skin condition | Injured person is able to easily locate the scar(s) or skin condition | Injured person is able to easily locate the scar(s) or skin condition | Injured person is able to easily locate the scar(s) or skin condition | |
No trophic changes | Minimal trophic changes | Trophic changes evident to touch | Trophic changes evident to touch | Trophic changes are visible | |
Any staple marks or suture marks are barely visible | Any staple marks or suture marks are visible | Any staple marks or suture marks are clearly visible | Any staple marks or suture marks are clearly visible | Any staple marks or suture marks are clearly visible | |
Location | Anatomic location of the scar(s) or skin condition is not clearly visible with usual clothing/hairstyle | Anatomic location of the scar(s) or skin condition is not usually visible with usual clothing/hairstyle | Anatomic location of the scar(s) or skin condition is usually visible with usual clothing/hairstyle | Anatomic location of the scar(s) or skin condition is usually visible with usual clothing/hairstyle | Anatomic location of the scar(s) or skin condition is usually and clearly visible with usual clothing/hairstyle |
Contour | No contour defect | Minor contour defect | Contour defect visible | Contour defect easily visible | Contour defect easily visible |
ADL/ | No effect on any ADL | Negligible effect on any ADL | Minor limitation in the performance of few ADL | Minor limitation in the performance of few ADL and exposure to chemical or physical agents (for example sunlight, heat, cold, etc.) may temporarily increase limitation | Limitation in the performance of few ADL (in addition torestriction in grooming and dressing) and exposure to chemical or physical agents (for example sunlight, heat, cold, etc.) may temporarily increase limitation or restriction |
No treatment, or intermittent treatment only, required | No treatment, or intermittent treatment only, required | No treatment, or intermittent treatment only, required | No treatment, or intermittent treatment only, required | No treatment, or intermittent treatment only, required | |
Adherence to underlying structures | No adherence | No adherence | No adherence | Some adherence | Some adherence |
Note: This table uses the principle of best fit. Medical assessors should assess the impairment to the whole skin system against each criteria and then determine which impairment category best fits (or describes) the impairment. A skin impairment will usually meet most, but does not need to meet all, criteria to best fit a particular impairment category.
Acknowledgements
The first version of these Guidelines was developed for the-then NSW Motor Accidents Authority by a consortium comprising Dr Jim Stewart, Associate Professor Ian Cameron, Associate Professor Malcolm Sim and Professor Peter Disler. The bulk of the task was undertaken by seven clinical reference groups, whose members are listed below. Particular mention should be made of the extensive contributions of Dr Dwight Dowda, Professor Sydney Nade and Dr Julian Parmegiani.
A number of Victorian clinicians with experience in the use of the AMA Guides (second and fourth editions) have provided valuable assistance. They are Dr Neil Cullen, Dr Michael Epstein, Dr Peter Lothian, Dr Gary Speck, Dr Richard Stark and Dr Nigel Strauss. Dr Alan Rosen provided valuable comment on the PIRS.
Upper extremity
Lower extremity
Spine
| Nervous system
ENT and scarring
Mental and behavioural disorders
Other body systems
|
Part 7 of the Motor Accident Guidelines: Dispute Resolution
Introduction
7.1 The dispute resolution process for motor accidents occurring on and after 1 December 2017 is set out in Part 7 of the Act. The process begins with an internal review by the insurer. If the internal review does not resolve the matter, an application maybe be made to the Personal Injury Commission.
7.2 This Part of the Guidelines is made under sections 6.23, 7.9, 7.12, 7.41, 7.47 and 10.2 of the Act. It provides for matters relating to insurer internal review. It also provides for some matters relating to legal incapacity and appointed representatives, merit review, miscellaneous claims assessments and restrictions on settlement of damages claims at the Personal Injury Commission.
7.3 Other matters relating to practice and procedure at the Personal Injury Commission are governed by the Personal Injury Commission Act 2020, Personal Injury Commission Rules 2021 and Procedural Directions issued by the President of the Personal Injury Commission. The Personal Injury Commission may be contacted for further information by:
Web: www.pi.nsw.gov.au
Telephone: 1800 PIC NSW (1800 742 679)
Email: [email protected]
Insurer internal review
Requesting an internal review
Time for requesting an internal review
7.4 A claimant may request an internal review of a decision within 28 days of receiving notice of the decision from the insurer.
7.5 If a claimant requests an internal review more than 28 days after receiving notice of the decision from the insurer, the insurer may decline or accept the application. The insurer must provide the claimant with a written notice of its decision to decline a late application for internal review. The notice must state that the claimant may refer a dispute of a reviewable decision of the insurer to the Personal Injury Commission for assessment because the insurer has declined to conduct an internal review.
Application requirements
7.6 A claimant may request an internal review by the insurer by:
(a) application form – completing the approved form for requesting an internal review by the insurer and delivering it to the insurer by post, email, facsimile or in person
(b) online application process – completing an approved online application for requesting an internal review by the insurer
(c) letter – contacting the insurer by letter and requesting an internal review
(d) telephone – contacting the insurer by telephone and requesting an internal review.
7.7 A request for an internal review of an insurer’s decision must include:
(a) all requirements specified in any paper or online application form approved by the Authority for making a request for an internal review
(b) details of:
- the decision of the insurer that is being referred for internal review
- the alternative decision sought in the internal review
- issues under review – the elements of the original decision that the claimant wishes to be reviewed
- the reasons the claimant believes the decision should be changed
- any additional documentation or materials that the claimant considers relevant to a review of the decision.
7.8 A claimant may withdraw a request for an internal review of a decision by letter, facsimile, telephone, email, or in person at any time before the insurer sends notification of the internal review decision to the claimant. The insurer must confirm the withdrawal of the request for an internal review in writing to the claimant.
Responding to an internal review application
7.9 The insurer must acknowledge receipt of the application for internal review by notifying the claimant within two business days of receiving the application.
7.10 The notification must be in writing and must be delivered either by post, email, online electronic delivery, or a combination of these methods, depending on the claimant’s preference.
7.11 The notification from the insurer must advise the claimant whether the insurer accepts that it can conduct an internal review of the decision, or alternatively whether the insurer does not accept it can conduct an internal review. The notification must include the date that the application was received and the date the internal review decision is due to be issued.
7.12 If the insurer accepts that it can conduct an internal review of the decision, the insurer must advise the claimant as soon as practicable, and in any event within seven days of receiving the application, of:
(a) issues under review – the elements of the original decision that the insurer understands are under review
(b) internal reviewer – the person allocated as the internal reviewer to conduct the internal review
(c) additional information – any additional relevant documents or information required from the claimant for the internal review, and any additional information or documentation that the insurer has that is relevant to the internal review and has not previously been provided to the claimant
(d) how to make contact – how the claimant can contact the insurer about the internal review, and how the claimant can contact the advisory service about the internal review.
7.13 If the insurer does not accept it can conduct an internal review, the insurer must notify the claimant in writing as soon as practicable and in any event within seven days of receiving the application of:
(a) reasons for decision – brief reasons for the decision to decline to conduct the review
(b) the internal reviewer – the person who decided to decline to conduct the review
(c) how to make contact – how the claimant can contact the insurer about the decision to decline to conduct the review, and how the claimant can contact the advisory service about the decision
(d) next steps for the claimant – the options available to the claimant if they disagree with the decision, including that they can seek legal advice as to the options available
(e) that the claimant may apply to the Personal Injury Commission to dispute a reviewable decision of the insurer because the insurer has declined to conduct an internal review.
7.14 If an insurer accepts it can conduct an internal review and then subsequently determines it cannot do so, the insurer must notify the claimant as soon as practicable and in any event within seven days of its decision to decline the application in accordance with the notification requirements set out above.
The internal review
The internal reviewer
7.15 An internal reviewer:
(a) must have the required skills, experience, knowledge and capability to conduct the internal review in accordance with the objects of the Act
(b) must not have been involved in making or advising on the insurer’s initial decision or previously managed any aspect of the claim, or be someone the initial decision-maker reports to or manages directly
(c) may have previously conducted an internal review for the same claim.
The internal review process
7.16 The internal review must be conducted in the way that best supports the objects of the Act, given the facts and circumstances of the particular claim and the particular internal review, which may include undertaking the review on the papers, using teleconferences, video conferences or face-to-face meetings as appropriate.
7.17 The internal reviewer may determine the internal review procedure, is not bound by the rules of evidence and may inquire into any matter relevant to the issues under review in such manner as the internal reviewer thinks fit.
7.18 The claimant may submit new information to the insurer to be considered by the internal reviewer.
7.19 The internal reviewer may consider information that was not provided before the decision being reviewed was made, under Division 7.3, section 7.9(6) of the Act. The insurer must give any such information to the claimant if it has not already been provided to the claimant. The claimant must also be given the opportunity to respond to the information.
7.20 The insurer may reasonably request information from the claimant for the purposes of the internal review, which the claimant must provide, under section 7.9(2) of the Act.
7.21 If the claimant does not provide the insurer with the information reasonably requested, the insurer may decline to conduct an internal review.
The internal review decision
7.22 In determining an internal review application, the internal reviewer must review the matter on the merits and make their decision having regard to the material before them, including the relevant factual material and applicable law.
7.23 In determining an internal review application, the internal reviewer may decide to:
(a) affirm the original decision
(b) vary the original decision
(c) set aside the original decision and make a decision in substitution for the original decision.
7.24 The insurer must notify the claimant of the results of the internal review within 14 days as required by section 7.9(4) of the Act, unless the Guidelines provide for particular circumstances in which an insurer has a longer period.
7.25 The table below provides for the circumstances in which an insurer has a longer period to complete the internal review and notify the claimant of the result.
Table 7.1: Internal review notification period
Circumstance | Longer review period |
|---|---|
Medical assessment matters about:
| 21 days |
Miscellaneous claims assessment matter about:
| 21 days |
After making the application for internal review, the claimant provides to the insurer new information of their own or at the insurer’s request that is relevant to the issues under review. | 14 days after the information is provided |
7.26 In any case, the maximum period including any longer periods above, must be no more than 28 days after the claimant’s request for the insurer to complete and give notice of the result of the internal review.
7.27 If the internal review decision results in the claimant being entitled to payment of benefits, the insurer must make that payment as soon as possible but in any event within 14 days after the internal review decision.
7.28 In notifying the claimant of the result of the internal review, the insurer must provide the claimant with:
(a) the internal reviewer’s certificate including brief reasons for the decision and supporting documents
(b) details of how and when the insurer will give effect to the internal reviewer’s decision
(c) details of the result of the internal reviewer’s decision on the claimant’s entitlement to statutory benefits
(d) the claimant’s right to seek independent legal advice
(e) information on how a claimant may apply to the Personal Injury Commission to dispute the insurer’s decision, including the Commission’s contact details
(f) information on how a claimant may make a complaint with the Independent Review Office (IRO), including the IRO’s contact details.
Legal costs for internal reviews
7.29 The Regulation in Part 6, Division 2, clause 23 provides that no costs are payable for legal services to a claimant or to an insurer in connection with an application for an internal review by the insurer.
Disputes
Legal incapacity and appointed representatives
7.30 Under Division 7.7, section 7.47(2) of the Act, an appointed representative is a person appointed to represent the claimant under legal incapacity, and may be a relative, friend or other suitable person who is willing and able to be appointed to represent the claimant.
7.31 If the claimant ceases to be a person under legal incapacity during the course of proceedings – for example, where a person turns 18 years of age – the appointed representative’s appointment will cease.
7.32 Any person may be appointed as a representative of a claimant except:
(a) a person under legal incapacity
(b) a person who has an interest in the proceedings that may be adverse to the interests of the person under legal incapacity.
Merit review
7.33 Under Division 7.4, section 7.12(4) of the Act, an insurer is required to provide to the claimant and the merit reviewer a statement of reasons (together with any supporting documentation) for a reviewable decision that is the subject of a merit review application, if requested to do so by a merit reviewer.
7.34 Under section 7.12(9) of the Act, an application for merit review must be made within 28 days of the claimant receiving the insurer’s decision, meaning:
(a) where an internal review is required before a merit review, the merit review application must be made:
- within 28 days of the claimant receiving the insurer’s internal review decision
- within 28 days of the claimant receiving the insurer’s decision to decline to conduct the internal review
- within 28 days after the date the insurer was required to complete the internal review in circumstances where the insurer has failed to complete the internal review and notify the claimant of the result within the period required under section 7.9(4)-(5) of the Act
(b) where an internal review is not required before a merit review as prescribed by the Regulation, the merit review application must be made within 28 days of the claimant receiving the insurer’s reviewable decision.
7.35 These time limits do not apply if a merit reviewer determines that it would best promote the objects of the Act to dispense with the time limit.
Miscellaneous claims assessment
7.36 Under section 7.41(2)(a) of the Act, a miscellaneous claims assessment matter may be referred for assessment without an internal review of the decision by the insurer if the dispute is about which insurer is the insurer of the at-fault motor vehicle for the purposes of section 3.3 (‘Determination of relevant insurer’), as listed in Schedule 2, clause 3(c) of the Act.
Damages settlement
7.37 Under section 6.23(3) of the Act, before the Personal Injury Commission may approve the settlement of a claim for damages, it must be satisfied that:
(a) the proposed settlement satisfies the timing requirements in section 6.23(1) of the Act
(b) the proposed settlement is just, fair and reasonable and within the range of likely potential damages assessments for the claim were the matter to be assessed by the Commission, taking into account the nature and extent of the claim and the injuries, disabilities, impairments and losses sustained by the claimant, and taking into account any proposed reductions or deductions in the proposed settlement
(c) the claimant understands that they are entitled to be represented in respect of the claim by an Australian legal practitioner
(d) the claimant understands the nature and effect of the proposed settlement and is willing to accept the proposed settlement.
Part 8 of the Motor Accident Guidelines: Health Practitioners authorised to give evidence in court and other dispute resolution proceedings
Introduction
8.1 This Part of the Guidelines provides for the appointment of health practitioners for the purposes of authorisation to give evidence under Division 7.7, section 7.52 of the Act.
8.2 This Part of the Guidelines applies to the appointment (including the reappointment) of health practitioners authorised to give evidence under section 7.52 on and from the date that these guidelines commence. A health practitioner holding current appointments under section 7.52 on the date these guidelines commence is appointed for the purposes of section 7.52 for the period of time being the remaining duration of the term of the health practitioner’s appointment or until that appointment is terminated, if terminated at an earlier date.
8.3 A health practitioner, (not being the injured person’s treating health practitioner), is authorised to give evidence in proceedings for the purposes of section 7.52 by:
(a) an agreement between the parties for the health practitioner to conduct a joint medical assessment, or
(b) appointment by the Authority to its list of health practitioners authorised to give evidence, or
(c) appointment by the Authority for a specific purpose and duration on application by a claimant or insurer.
8.4 Health practitioners authorised to give evidence under section 7.52 of the Act and these guidelines, must:
(a) comply with all relevant legal requirements for practice, relevant guidelines, policies and codes of conduct
(b) comply with the relevant law including the Motor Accident Injuries Act 2017 (NSW), the Motor Accident Injuries Regulation 2017 (NSW), these Guidelines, Procedural Direction PIC4 – Expert Witness Evidence and any subsequent procedural directions issued by the President of the Personal Injury Commission relating to expert witness evidence. They should promptly notify the Authority of any compliance breaches.
(c) comply with the standards and conduct for medico-legal consultation, examination and reports set out in the NSW Medical Council Guideline – Medico-Legal Consultations and Examinations
(d) act without bias and in a way that does not give rise to an apprehension of bias in the performance of their responsibilities
(e) act in an ethical, professional and considerate manner when examining injured people and practise procedural fairness when conducting medical assessments and writing reports. This includes respectful communication with injured people and considering their individual needs, providing impartial assessments and ensuring that injured people are given the opportunity to explain any inconsistencies observed during an examination or in supporting material.
(f) comply with all privacy obligations including under the Health Records and Information Privacy Act 2002 (NSW)and the Privacy Act 1988 (Cth)
(g) have successfully completed the relevant Authority’s training requirements in permanent impairment evaluation, before undertaking and providing opinion on whole person impairment (WPI) assessments.
8.5 Health practitioners must not during the term of their appointment:
(a) provide treatment advice and/or services to an injured person about whom they are providing evidence as a health practitioner
(b) accept a referral or examine an injured person if the health practitioner has a conflict of interest
(c) ask for or accept any inducement, gift, or hospitality from individuals or companies, or enter arrangements that could be perceived to provide inducements, that may affect, or be seen to affect, the health practitioner’s ability to undertake the role of a health practitioner authorised to give evidence in an impartial and unbiased manner
(d) engage in activities or publicly express opinions that might be perceived to compromise the health practitioner’s ability to undertake the role of a health practitioner authorised to give evidence in an impartial and unbiased manner
(e) undertake medical assessments and give evidence outside of their area(s) of expertise.
8.6 To be authorised to give evidence in proceedings, a health practitioner must be authorised under section 7.52 and these guidelines at the time the evidence is given. For evidence given by written report, the health practitioner must be authorised at the time the health practitioner examines the claimant and writes the report. If evidence of the health practitioner is admitted into evidence, the health practitioner continues to be authorised to give further evidence on cross-examination and re-examination of that evidence in proceedings.
Joint medical assessments
8.7 Both parties shall use their best endeavours to agree to a joint medical or other health-related assessment, taking into account the individual circumstances and preferences of the injured person, to minimise the number of medical assessments that they are required to attend. Either party may initiate a request for a joint medical or other health-related assessment.
8.8 In a claim, where a legally-represented claimant and an insurer agree to a health practitioner conducting a joint medical assessment, that health practitioner is authorised under section 7.52(1)(b) of the Act for the purposes of the claimant in the claim concerned.
8.9 The parties must instruct the health practitioner in writing to conduct the joint medical assessment, and to send the report and any supplementary reports to both parties on completion.
8.10 If a party identifies an error in the report, it may request the health practitioner to re-issue the report with the correct information. The party must send the request and supporting evidence to the health practitioner in writing within seven days of receiving the initial report and provide a copy of the request and supporting evidence to the other party.
8.11 A supplementary report must be agreed to by both parties to be considered a joint report . A report issued by the health practitioner to correct an error is not considered supplementary.
8.12 The insurer must meet the cost of the joint medical assessment, including the initial report and any supplementary reports agreed by the parties.
Appointment by the Authority to its list of health practitioners authorised to give evidence
8.13 A health practitioner seeking appointment (including re-appointment) to the Authority’s list of health practitioners authorised to give evidence must apply to the Authority by completing and submitting the application form available on the Authority’s website.
8.14 The Authority will determine the application for appointment against the eligibility requirements and notify the applicant in writing of its decision.
8.15 The Authority will publish on its website the details of health practitioners appointed to its list, including their names, contact details, practice locations, and other information relevant to their role as a health practitioner authorised to give evidence.
Eligibility requirements
8.16 The Authority may appoint a health practitioner to its list of health practitioners authorised to give evidence if it is satisfied that the health practitioner:
(a) is a health practitioner registered with the Australian Health Practitioner Regulation Agency (AHPRA), with no conditions, undertakings, reprimands, limitations or restrictions on registration as a result of a disciplinary process, and is not subject to supervisory requirements
(b) has at least five years of full-time equivalent relevant clinical experience, and/or two years of full-time equivalent relevant clinical experience in addition to an advanced qualification recognised by the relevant professional body that sets training standards for its members, where a professional body has requested the Authority consider the qualification as relevant
(c) has knowledge of the treatment and management of injuries in personal injury schemes and return to activity
(d) is in current clinical practice or a teaching position in the relevant specialty, or has recently been in clinical practice, or undertakes professional activities such that they are aware of current clinical practice
(e) has high-level communication skills, including interpersonal skills and report writing skills, such that they would be able to comply with the requirements for consultations, examinations and reports outlined in the NSW Medical Council titled ‘Guidelines for medico-legal consultations and examinations’
8.17 The Authority will consider all relevant information available to assess whether a health practitioner meets the eligibility requirements and may request additional information from the applicant or relevant third parties. This may include:
(a) information related to complaints, compliance, or breaches of legislation, guidelines, or fee schedules within the past 10 years
(b) conditions on registration or current disciplinary proceedings that may affect the practitioner’s registration, ability to undertake the role, or integrity of the NSW Motor Accidents CTP Scheme
(c) any pending criminal charges or any criminal convictions and/or demonstrated behaviour that may affect the practitioner’s ability to undertake the role with impartiality and fairness or may affect the integrity of the CTP Scheme.
8.18 Health practitioners are appointed to the Authority’s list for up to three years, with an option for the Authority to extend the appointment, at its discretion. Health practitioners must re-apply to continue to be authorised to give evidence after the expiration of their term, unless the Authority has notified the health practitioner that the health practitioner’s term has been extended and the period of that extension.
8.19 Health practitioners appointed to the Authority’s list must continue to meet clauses 8.4 and 8.5, the eligibility requirements and comply with the terms of appointment to remain authorised during their period of appointment.
Declining an application
8.20 The Authority may decline a health practitioner’s application. If the Authority declines to appoint a health practitioner, the Authority will notify the practitioner in writing, including:
(a) brief reasons for that decision
(b) a time period, if any, before the health practitioner may re-apply for appointment and the reasons for that nominated period.
8.21 If the health practitioner disagrees with the Authority’s decision, the health practitioner may ask the Authority to review its decision by writing to the Authority at [email protected] within 21 days of receipt of the decision. The health practitioner is to provide any relevant information as to why their application should be accepted. The Authority will undertake the internal review and notify the health practitioner of the outcome within 21 days of receiving the request for review or within 21 days after receiving the last document or information the Authority may request from the health practitioner, if the Authority requested additional information.
8.22 A health practitioner seeking to re-apply must complete a new application form.
Terms of appointment
8.23 In addition to the requirements set out in clauses 8.4 and 8.5, health practitioners appointed to the Authority’s list must:
(a) complete at least two hours of continuing professional development (CPD) related to medico-legal practice during the three-year period of authorisation, including but not limited to training about conducting medico-legal assessments, dispute resolution, communicating with injured people and/or writing medico-legal reports. This may be as part of the general minimum requirements set out by AHPRA for each relevant Board and may be provided by any relevant CPD provider
(b) agree to the Authority publishing on its website the health practitioner’s name, contact details, practice location(s), and other information relevant to the terms and extent of their appointment
(c) notify the Authority at [email protected] within 14 days of any change to name or details
(d) notify the Authority within seven days of changes to any circumstances that may compromise their ability to meet the eligibility requirements and comply with the terms of appointment
(e) have access to the necessary resources and infrastructure to do all administrative activities necessary for the role
(f) establish and maintain appropriate and secure record management systems to manage work and maintain records and data lawfully and efficiently
(g) participate in the Authority’s performance framework for health practitioners authorised to give evidence, including complying with any mandatory training and data reporting requirements
(h) co-operate with the Authority’s complaints-handling framework, including responding to complaints with full and accurate details and, when indicated by the Authority, taking remedial action.
8.24 A health practitioner appointed to the Authority’s list must accept all referrals whether made on behalf of an injured person or an insurer, and must only decline a request if:
(a) they are not adequately qualified or experienced
(b) the request relates to a medical matter for which the health practitioner is not authorised to give evidence
(c) the health practitioner has a conflict of interest (personal, professional, and/or financial)
(d) they are a decision-maker at the Personal Injury Commission for the same claim
(e) for any other reasonable reason the health practitioner is unable to complete the assessment and report within the terms specified by the requesting party.
Restrictions
8.25 The Authority may impose restrictions on a health practitioner authorised to give evidence.
8.26 A restriction may include limiting the authorisation to give evidence in:
(a) specified medical matters, or
(b) medical matters in specified claims, or
(c) medical matters related to specified claimants or kinds of claimants.
8.27 The Authority may also restrict a health practitioner’s appointment to a defined period or for the duration of a specific claim.
8.28 The Authority may impose a restriction on a health practitioner’s appointment at any time during the period of authorisation, after first notifying the health practitioner.
Cessation of appointment
8.29 The Authority may revoke a health practitioner’s appointment at any time. The Authority will notify the health practitioner in writing of its revocation and the reasons for the revocation.
8.30 If the health practitioner disagrees with the Authority’s decision, the health practitioner may request a review of the decision within 14 days of receipt of the decision and provide any relevant information as to why the appointment should not be revoked. The Authority will undertake the review and notify the health practitioner of the outcome within 21 days after receipt or if the authority requests further information, within 21 days after receiving the last document or information.
8.31 A health practitioner may cease their appointment at any time during the term of the appointment by notifying the Authority in writing.
8.32 A health practitioner whose appointment has been revoked, or a health practitioner who ceases their appointment, must as soon as possible cancel any appointments for medical assessments due to take place after the date of revocation or cessation, and notify all affected parties of those cancellations. They must issue any reports related to the medical assessments conducted prior to their revocation or cessation as soon as possible. They must not accept any new bookings for medical assessments as a health practitioner authorised to give evidence under section 7.52 and these guidelines.
8.33 When a health practitioner’s appointment is revoked, or a health practitioner ceases their appointment, the evidence given by the health practitioner in the period when the health practitioner was authorised, including at the examination of the claimant and production of a report, is admissible for the purposes of section 7.52 of the Act. The health practitioner continues to be authorised for any cross-examination and re-examination during the proceedings.
Appointment by the Authority on application by the parties
8.34 If a claimant or insurer proposes to obtain evidence from a health practitioner not appointed to the Authority’s list of health practitioners authorised to give evidence, a claimant or an insurer may apply by writing to the Authority at [email protected] to seek the authorisation of that health practitioner. The health practitioner must be authorised prior to examining the claimant and writing a report.
8.35 A health practitioner appointed under this section must comply with the requirements set out in clauses 8.4 and 8.5 in these guidelines.
8.36 The application to the Authority must include:
(a) reasons why the applicant party cannot obtain evidence from a health practitioner on the Authority’s list
(b) reasons why a joint medical assessment cannot be arranged
(c) the name, address and qualifications and/or experience of the health practitioner the applicant party requests the Authority to appoint
(d) details of the specific claim or claims for which the evidence is being sought, including claim number, claimant name, and other identifying information.
8.37 For the purposes of section 7.52, the Authority may appoint the nominated health practitioner if the Authority is satisfied that:
(a) the applicant party cannot obtain the required evidence from a health practitioner on the Authority’s list, and
(b) the health practitioner has suitable qualifications and skills to give the evidence.
8.38 The Authority will consider all relevant information to assess whether a health practitioner meets the eligibility requirements and may request additional information from the applicant or third parties. This may include:
(a) information related to complaints, compliance, or breaches of legislation, guidelines, or fee schedules within the past 10 years
(b) conditions on registration or current disciplinary proceedings that may affect the practitioner’s registration, ability to undertake the role, or integrity of the CTP Scheme
(c) any pending criminal charges or any criminal convictions and/or demonstrated behaviour that may affect the practitioner’s ability to undertake the role with impartiality and fairness or may affect the integrity of the CTP Scheme.
8.39 The Authority will determine the application for appointment and notify the applicant in writing of its decision. Where the Authority accepts the appointment, the Authority will also notify the health practitioner that the health practitioner is authorised to give evidence and outline the terms of the appointment including any restrictions.
8.40 The claimant or insurer relying on evidence from a health practitioner appointed by the Authority on application by a party must provide to the other party a copy of the Authority’s notification of authorisation at the time the report is served or relied upon, whichever is the earlier.
8.41 Unless otherwise specified by the Authority, a health practitioner appointed by the Authority on application by a party is authorised only for the purposes and duration of the relevant claim or claims. The Authority may impose further restrictions on the appointment at any time during the period of authorisation.
8.42 A health practitioner authorised to give evidence by the Authority on application by a party must include in the health practitioner’s report(s) a statement that they are authorised by the Authority and any restrictions on the appointment that apply.
8.43 The Authority may revoke a health practitioner’s authorisation by the Authority on application by a party at any time. The Authority will notify the applicant and the health practitioner in writing and advise the reasons for the revocation. The guidelines for ‘Cessation of appointment’ in this Part will apply.
Glossary
Abbreviation | Definition |
|---|---|
ABS | Australian Bureau of Statistics |
AF | At fault |
AMA | Australian Medical Association |
AMA4 | Guides to the Evaluation of Permanent Impairment, Fourth Edition (third printing, 1995) published by the American Medical Association |
APRA | Australian Prudential Regulation Authority |
CDR | Clinical dementia rating |
CRPS | Complex regional pain syndrome |
CT scans | Computerized axial tomography scan |
CTP | Compulsory third party |
DCO | Diffusing capacity of carbon monoxide |
DRE | Diagnosis-related estimates |
DSM | Diagnostic & Statistical Manual of Mental Disorders |
DSM-5 | Diagnostic & Statistical Manual of Mental Disorders, Fifth Edition, 2013, published by the American Psychiatric Association. |
EEG | Electroencephalogram |
EFT | Electronic funds transfer |
eGreenSlip | Electronic notification of a third-party policy by an insurer to Roads & Maritime Services |
ENT | Ear, nose and throat |
FEV1 | Forced expiratory volume |
Fund levy | The combined total of the Motor Accidents Operational Fund levy, Lifetime Care & Support Authority Fund levy and Motor Accident Injuries Treatment & Care Benefits Fund levy |
FVC | Forced vital capacity |
ICD | International Statistical Classification of Diseases & Related Health Problems |
ITC | Input tax credit |
LTCS | Lifetime Care & Support Scheme |
MAF | Motor Accidents Operational Fund |
MAI | Motor accident injuries |
MAITC | Motor Accident Injuries Treatment & Care Fund |
MRC | Medical Research Council |
MRI scans | Magnetic Resonance Imaging Scan |
NAF | Not at fault |
PC | Personal care |
PIRS | Psychiatric impairment rating scale |
REM | Risk equalisation mechanism |
RMS | Roads & Maritime Services |
ROM | Range of motion |
SCI | Spinal cord injuries |
SI | Superimposed inflation |
SLR | Straight leg raising |
TAFE | Technical and Further Education |
TEMSKI | Table for the evaluation of minor skin impairment |
| UCD | Universal Claims Database, the claims register established under section 10.25 of the Act |
| UPD | Universal Policy Database |
UEL | Upper extremity impairment |
VIN | Vehicle identification number |
VO2 max | Measurement of exercise capacity |
WHO | World Health Organisation |
WOVR | Written-off vehicles register |
WPI | Whole person impairment |
Version number
The current Motor Accident Guidelines are Version 9.2 published 10 November 2023.
Earlier versions and a summary of the version changes are listed below.
| Version number | Effective date | Summary of changes |
|---|---|---|
| Version 9.2 | 10 November 2023 onwards | Updates to version 9.2 |
| Version 9.1 | 1 April 2023 - 10 November 2023 | Updates to version 9.1 |
| Version 9 | 15 January 2023 - 31 March 2023 | Updates to version 9 |
| Version 8.2 | Clause 4.103 to 4.105 and Part 9 effective date 8 April 2022 to 24 November 2022 - from 25 November 2022 refer to Motor Accidents Guidelines: CTP Care. All other parts effective date 8 April 2022 to 14 January 2023 | Updates to version 8.2 |
| Version 8.1 | 17 December 2021 - 8 April 2022 | Updates to version 8.1 |
| Version 8 | 29 October 2021 - 16 December 2021 | Updates to version 8 |
| Version 7 | 1 March 2021 - 28 October 2021 | Updates to version 7 |
| Version 6 | 18 December 2020 to 28 February 2021 | Updates to version 6 |
| Version 5.1 | 17 April 2020 to 17 December 2020 | - |
| Version 5 | 20 December 2019 to 16 April 2020 | - |
| Version 4 | 15 January 2019 to 19 December 2019 | - |
| Version 3 | 13 July 2018 to 14 January 2019 | - |
| Version 2 | 30 April 2018 to 12 July 2018 | - |
| Version 1 | 1 December 2017 to 29 April 2018 | - |